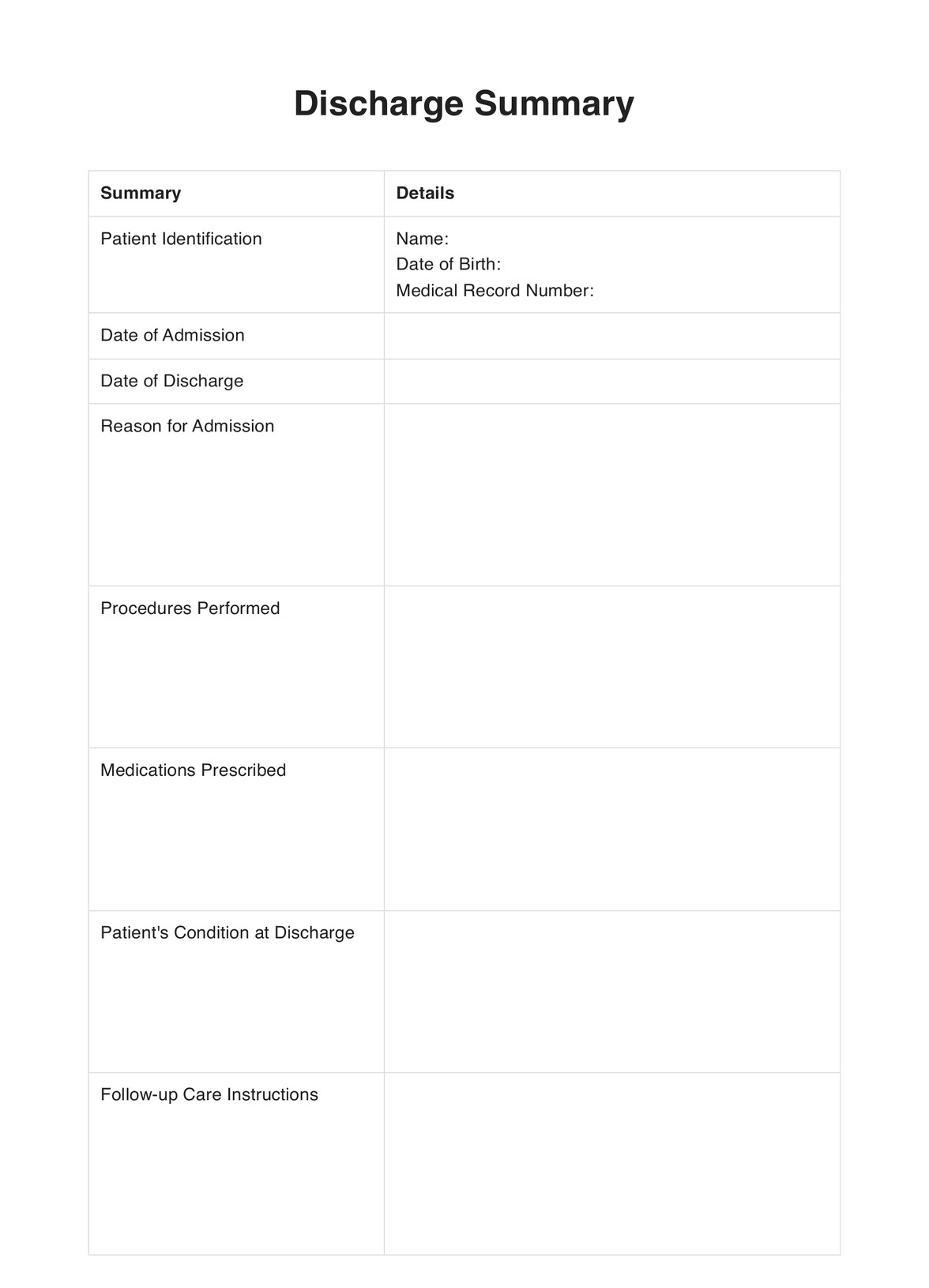
Discharge Summary
Explore a detailed guide on a discharge summary, its requirements, examples, and a free downloadable template to streamline patient care transitions.


What is a Discharge Summary?
A Discharge Summary is a comprehensive report created by healthcare providers, typically doctors or nurse practitioners, at the end of a patient's hospital stay or course of treatment. It is an essential communication tool between hospital care teams and primary care physicians or outpatient providers, ensuring seamless continuity of care. It's an important thing to add to patient records for clinical documentation.
This brief hospital course summary is a critical and comprehensive document that includes information about the patient's hospital stay, the reason for admission, discharge medications and treatments provided, mental health care the patient received (if any), if discharge letters have been sent to the patient and their family, and the patient's health status at discharge. Additionally, it includes instructions for follow-up care, including medications, lifestyle modifications, and future healthcare appointments.
Given its pivotal role in patient care, a well-crafted Discharge Summary can improve patient outcomes, reduce readmission rates, and enhance overall healthcare efficiency.
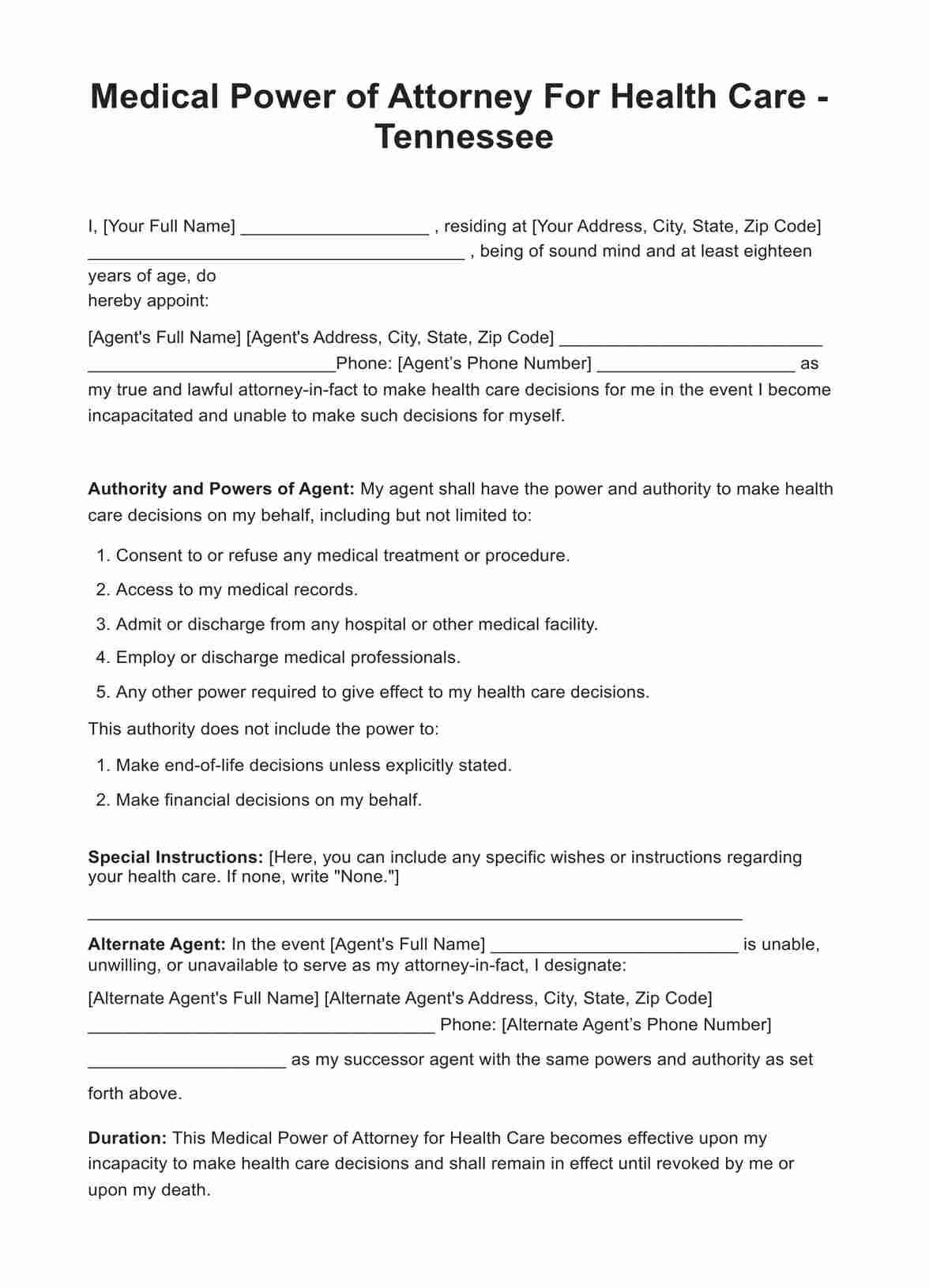
Discharge Summary Template
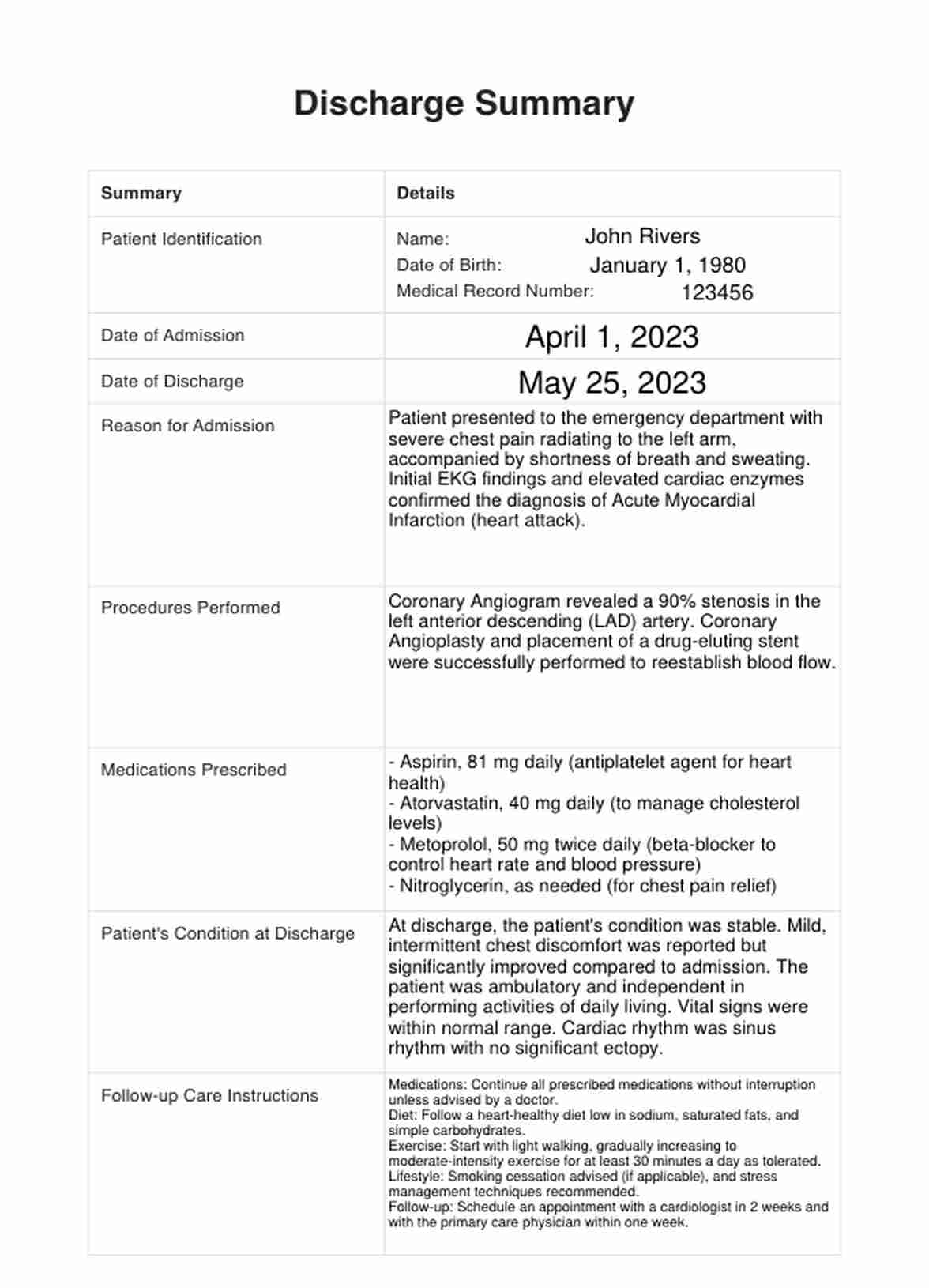
Discharge Summary Example
How do discharge summaries work?
Writing discharge summaries involve multiple steps to ensure all relevant and required information is included. A printable Discharge Summary template can make it easier for you to write a Discharge Summary:
Step 1: Access the template
Click the "Use Template" button to open the template in the Carepatron app, or you can save a PDF version to your device by clicking "Download."
Step 2: Input patient information
Enter the patient's essential information, such as name, date of birth, and medical record number. Include the dates the patient was admitted and the discharge date.
Step 3: Write the reason for admission
Detail the primary diagnosis or condition that necessitated hospitalization. You may also include a history of present illness.
Step 4: Perform procedures
Describe any surgical or non-surgical procedures done during the hospital stay.
Step 5: Prescribe medications
List the medications prescribed to the patient at discharge, including dosages and frequency.
Step 6: Summarize patient's health status at discharge
Provide a summary of the patient's health status at discharge.
Step 7: Create follow-up care instructions
Offer detailed instructions for post-hospital care, including medications, dietary restrictions, physical activity recommendations, and future appointments.
Step 8: Write a hospital stay summary
Summarize the patient's hospital stay, including the course of care during hospitalization, from symptoms and diagnoses to treatments and patient responses. Keeping a Discharge Summary for future use would help monitor a patient's past medical history, primarily through electronic health records.
When would you use this template?
This template for Discharge Summary is a vital tool utilized at the end of a patient's hospital stay. Its primary function is to ensure a smooth transition of care from an inpatient hospital setting to an outpatient or home care setting or even to a different healthcare provider.
This is especially crucial when patients have complex healthcare needs or multiple conditions requiring coordinated care among specialists.
It is also an excellent tool for facilitating communication among healthcare entities, including skilled nursing facilities, rehabilitation centers, home health agencies, and outpatient providers. The information contained within the summary enables these providers to understand the patient's recent medical history and adjust their Care Plans accordingly.
In summary, a Discharge Summary template would be used whenever a patient's care is being transitioned from the hospital to another setting or when the responsibility for the patient's care is transferred to another healthcare provider. Clarity, consistency, and compliance with regulations make the template indispensable in providing high-quality, coordinated patient care.
Benefits
A Discharge Summary is a crucial component of effective healthcare, enabling seamless continuity of care from hospital-based treatment to outpatient or primary care. By using a standardized template for discharge summaries, healthcare providers can ensure that all pertinent information is included, reducing the risk of errors or miscommunications. Here, we delve into the key benefits of using a Discharge Summary template:
Improved care continuity
A comprehensive Discharge Summary enables smoother handovers between healthcare professionals. It offers a concise, organized record of the patient's medical history, treatments received, and progress made during hospitalization, thus facilitating continued care in an outpatient setting or by a new provider.
Standardization
By using a standardized template, healthcare providers can ensure that all discharge summaries follow the same format, thus improving readability and reducing the chance of critical information being missed or overlooked. This standardization also aids in data analysis and research, as data points are consistently recorded across different summaries.
Compliance
Regulatory bodies, such as the Centers for Medicare & Medicaid Services (CMS), require what a Discharge Summary must contain. A template meeting these standards can simplify compliance efforts, ensuring all mandatory information is included and the summary meets the stipulated format.
Efficiency
Drafting a Discharge Summary from scratch can be time-consuming. A template streamlines the process, allowing healthcare professionals to complete summaries more quickly. This can be especially beneficial in busy hospital settings. By saving time on paperwork, clinicians can devote more attention to patient care.
Patient safety
The Discharge Summary is vital to patient safety, particularly during the transition from inpatient to outpatient care. A clear, comprehensive summary ensures that patients, their families, and their ongoing care providers understand the patient's health status, what treatments were provided, and what care should be continued or initiated after hospital discharge. This can help prevent misunderstandings or gaps in care that could compromise patient safety.
Accessibility
With a free, printable Discharge Summary template, all healthcare providers can access a tool that helps them create thorough, standardized discharge summaries regardless of their setting or resources. This can help reduce disparities in care quality and improve overall health outcomes.
Commonly asked questions
A Discharge Summary is used after a patient's hospital stay to transition them from inpatient to outpatient care or transfer care to another healthcare provider.
A Discharge Summary includes patient identification, admission and discharge dates, the reason for admission, procedures performed, medications prescribed, patient's condition at discharge, follow-up care instructions, and a summary of the hospital stay.
A Discharge Summary assesses the patient's health journey during their hospital stay, including their initial condition, progress, treatment responses, and health status at discharge. It also outlines the plan for ongoing care post-hospitalization.




















-template.jpg)