Rejection Sensitivity Treatment Plan
Access a structured blank Rejection Sensitivity Treatment Plan to help clients manage triggers, build coping skills, and strengthen emotional resilience effectively.


What is rejection sensitivity?
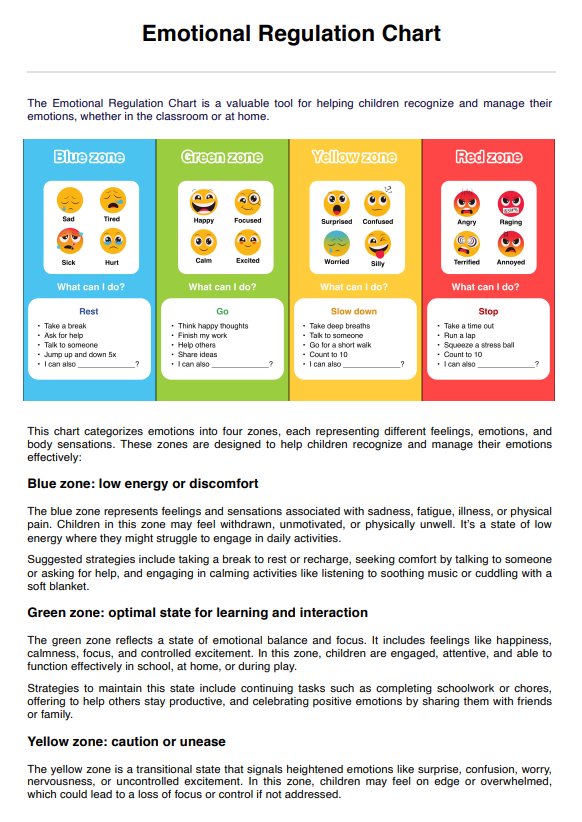
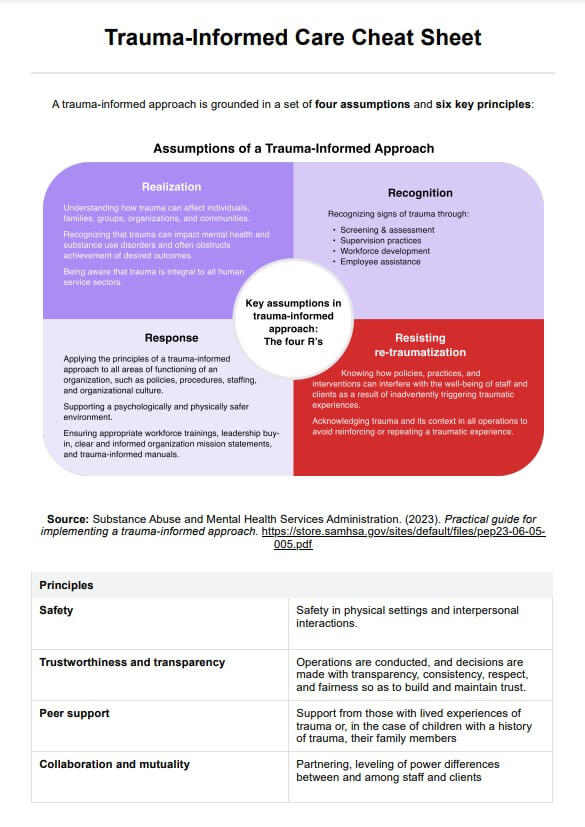
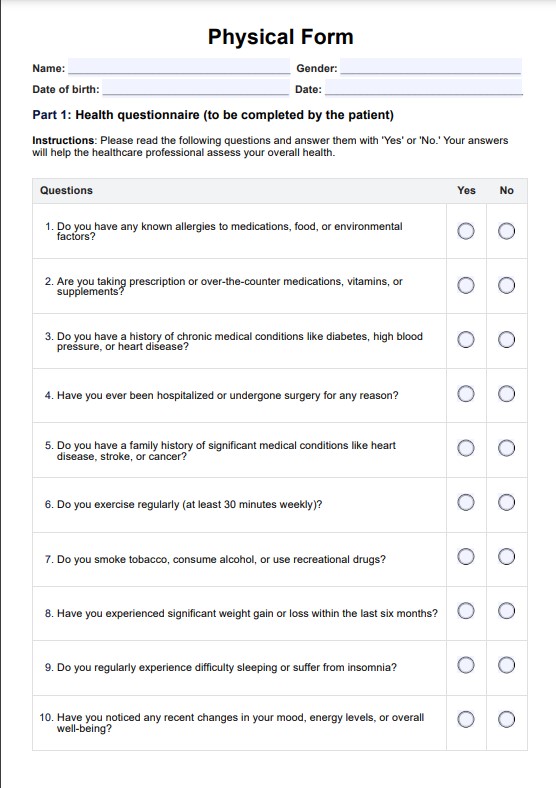
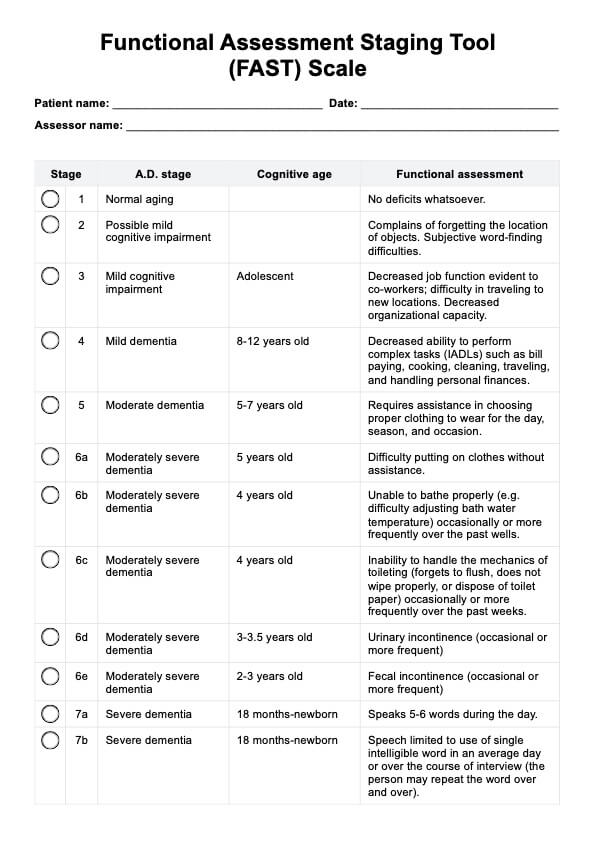
Rejection sensitivity is a heightened emotional response to perceived or actual rejection, commonly linked with rejection-sensitive dysphoria (RSD) and attention deficit hyperactivity disorder (ADHD). It involves severe emotional pain, intense emotional reactions, and overwhelming feelings triggered by negative feedback, perceived rejection, criticism, or social interactions. People with RSD often struggle with emotional dysregulation, low self-esteem, and negative self-talk, which can lead to significant emotional distress and difficulty managing overwhelming emotions.
This condition may also be associated with autism spectrum disorder, borderline personality disorder, or other mental health conditions. Symptoms of rejection sensitivity can include sudden outbursts, emotional intensity, and difficulties in social settings due to heightened sensitivity to perceived criticism or rejection.
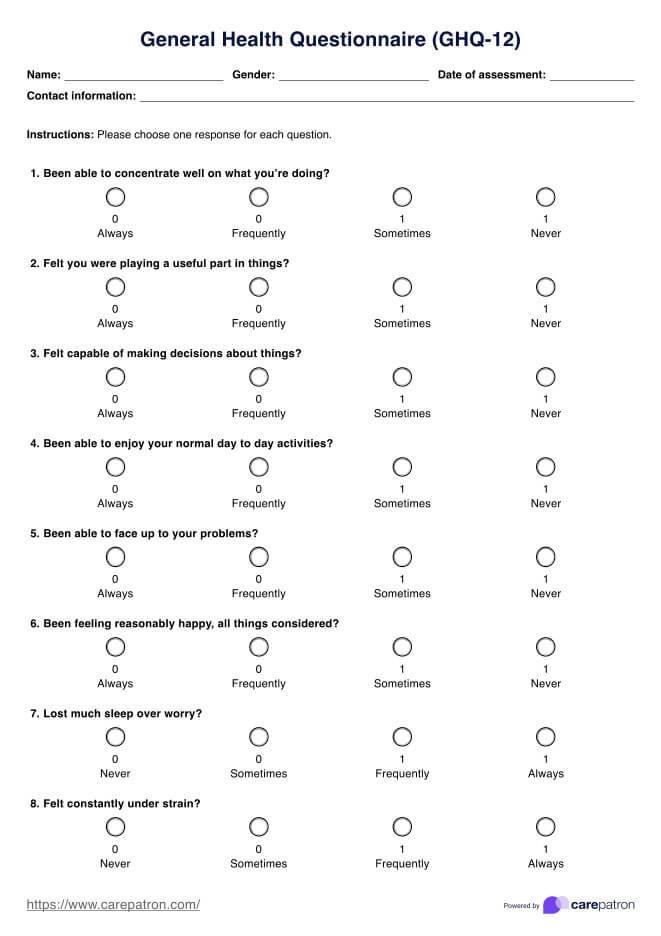
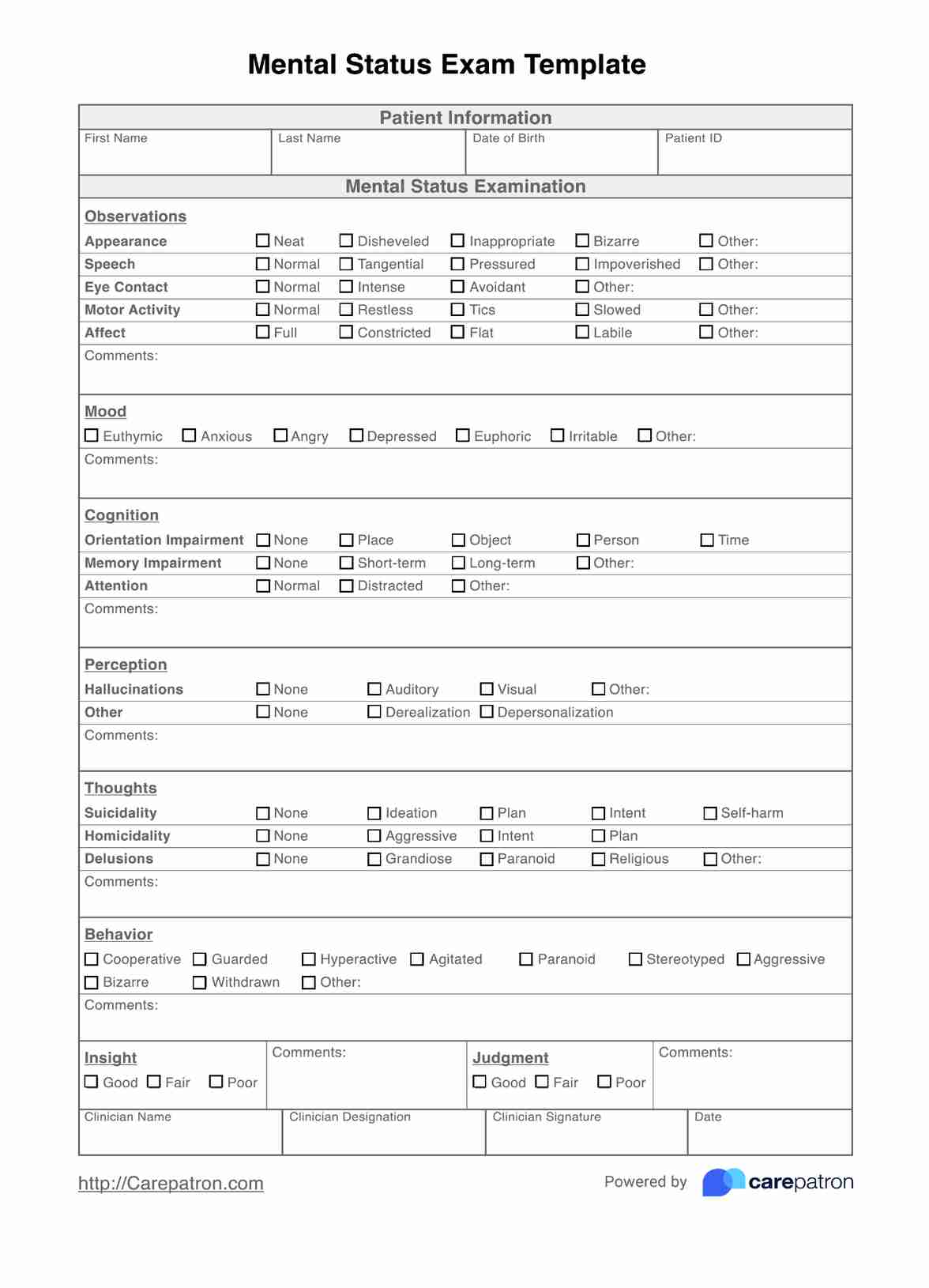
Understanding rejection sensitivity is essential for mental health professionals to assess and diagnose related mental disorders, such as mood disorders, and provide appropriate treatment. Managing rejection sensitivity with tailored coping strategies, emotional regulation techniques, and talk therapy can improve emotional well-being, enhance relationships, and reduce the impact of other negative emotions and thought patterns. Addressing this condition also helps individuals develop self-compassion, gain insight into their emotional responses, and navigate the challenges posed by rejection sensitivity.
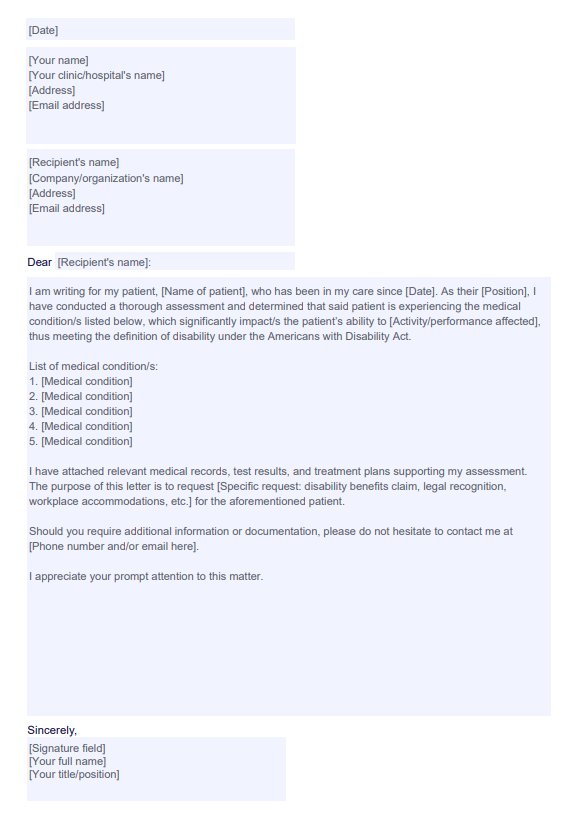
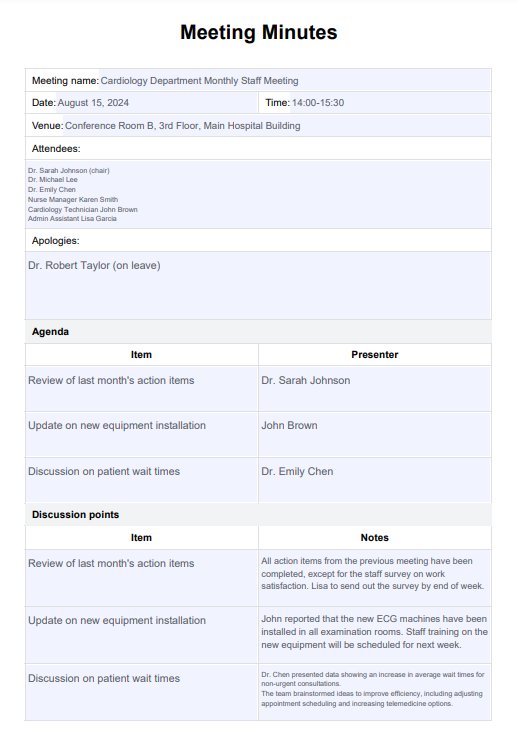
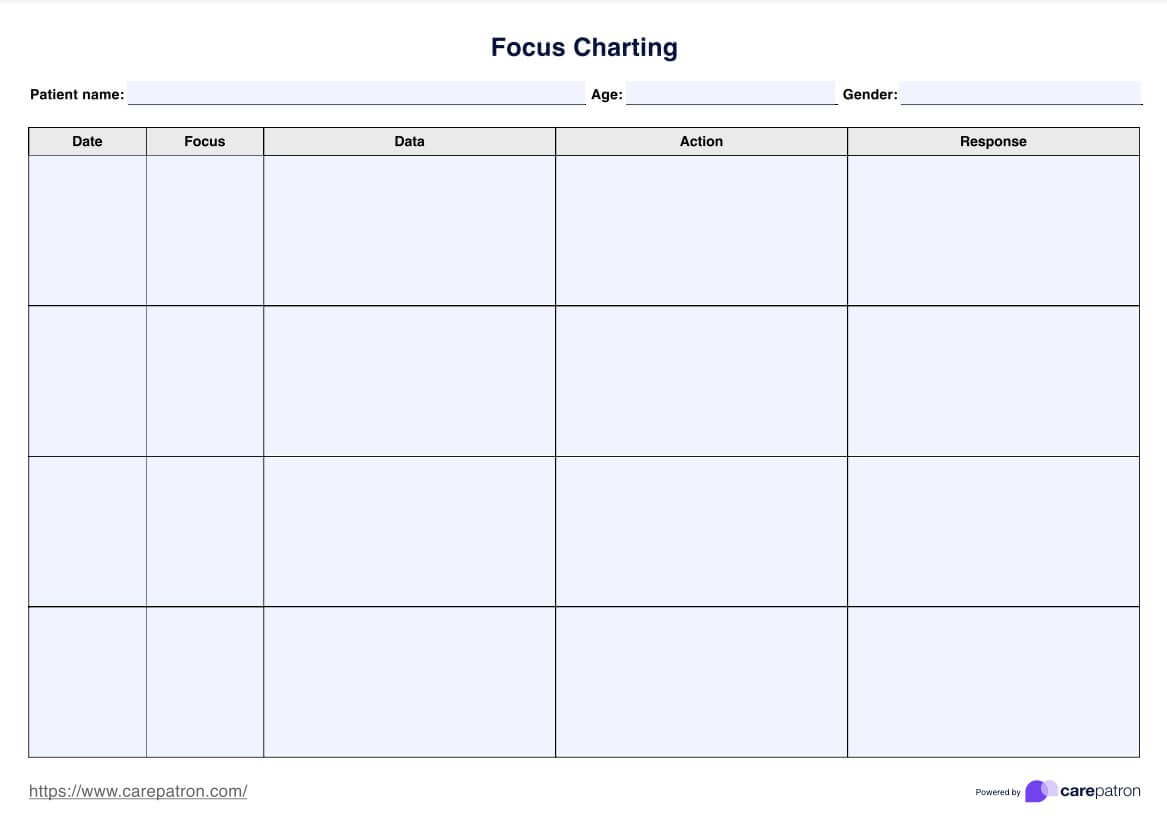
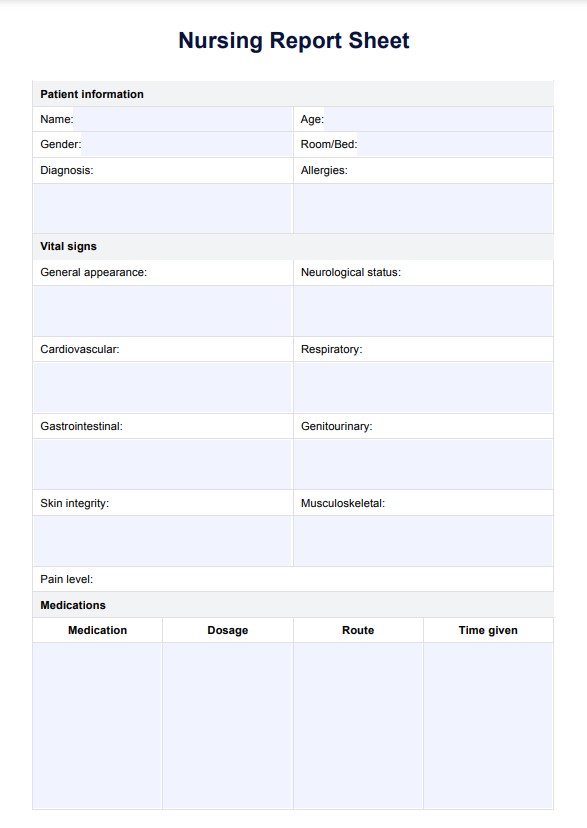
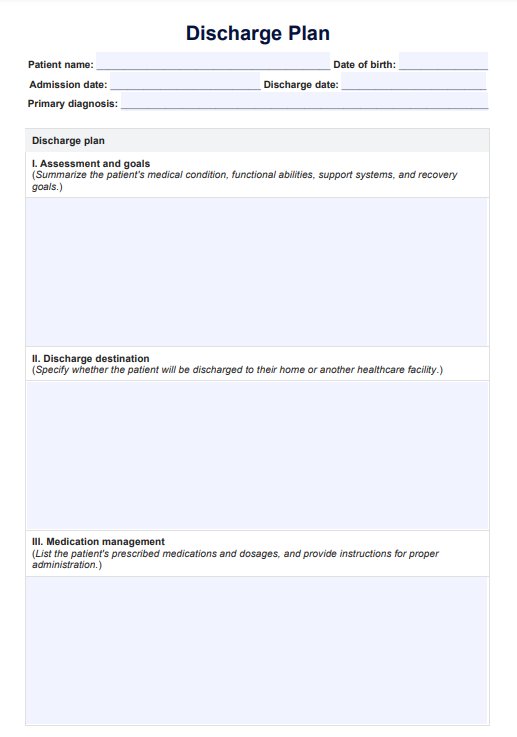
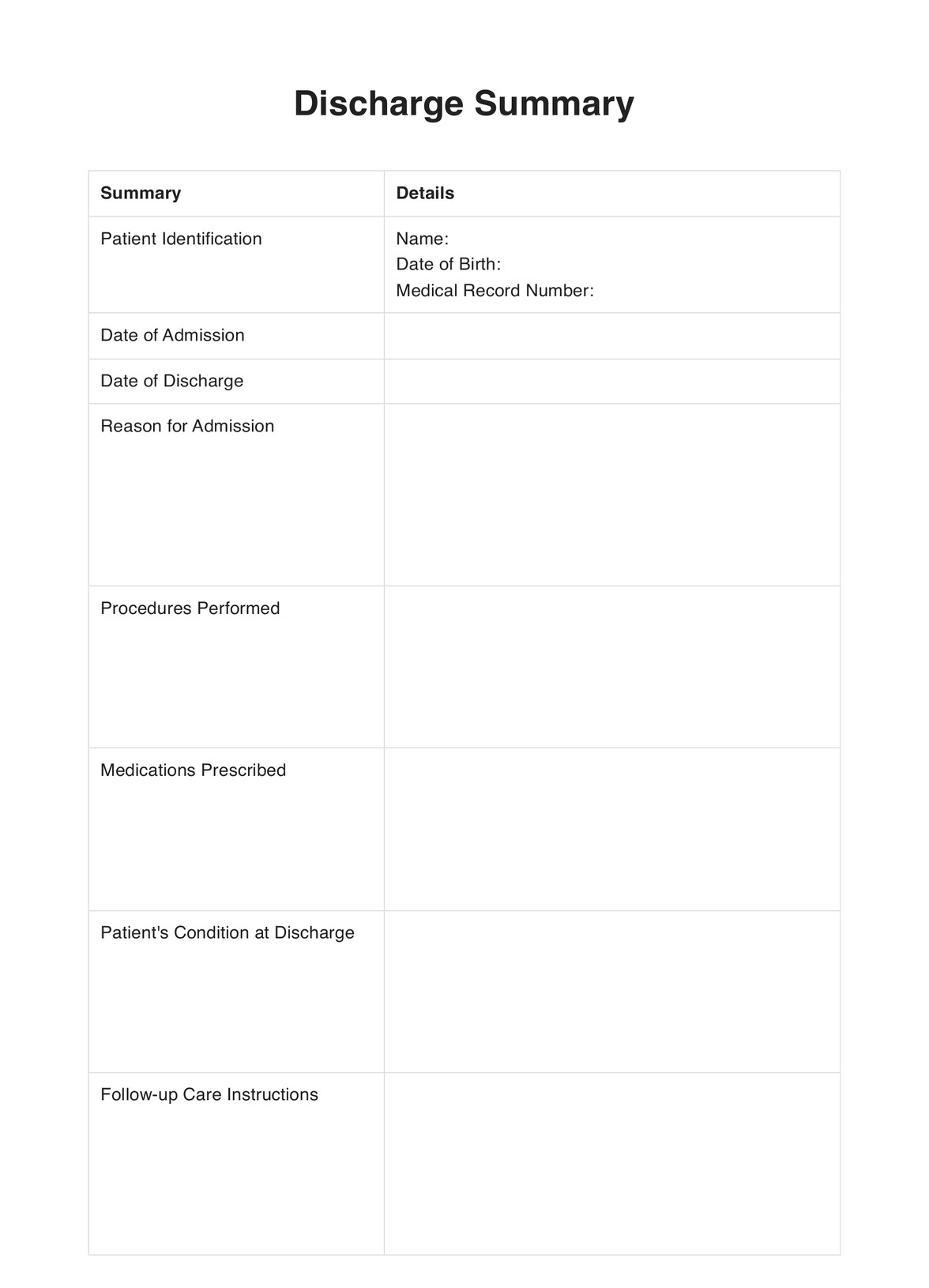
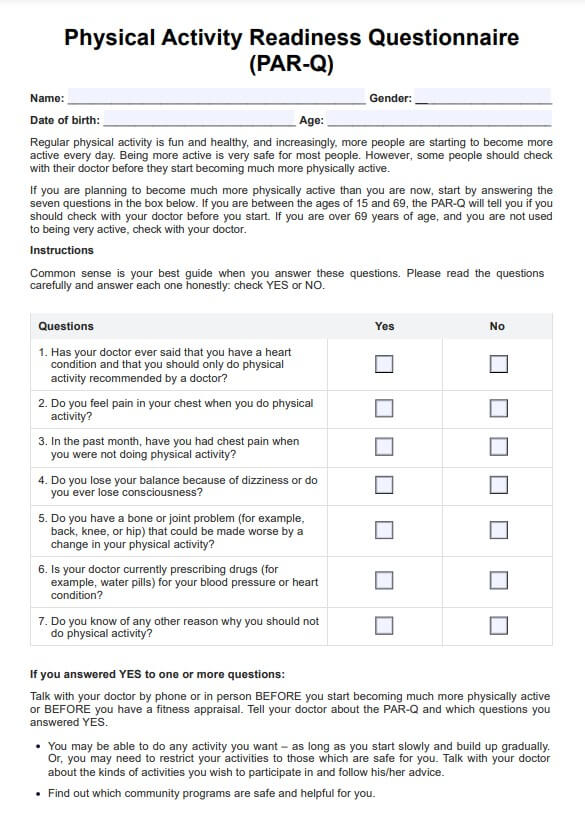
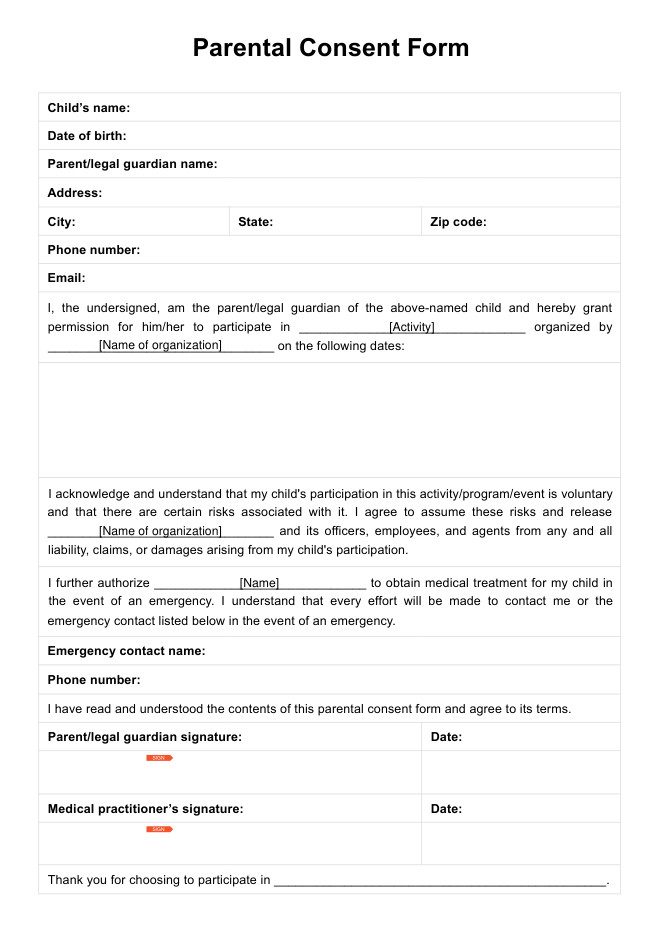
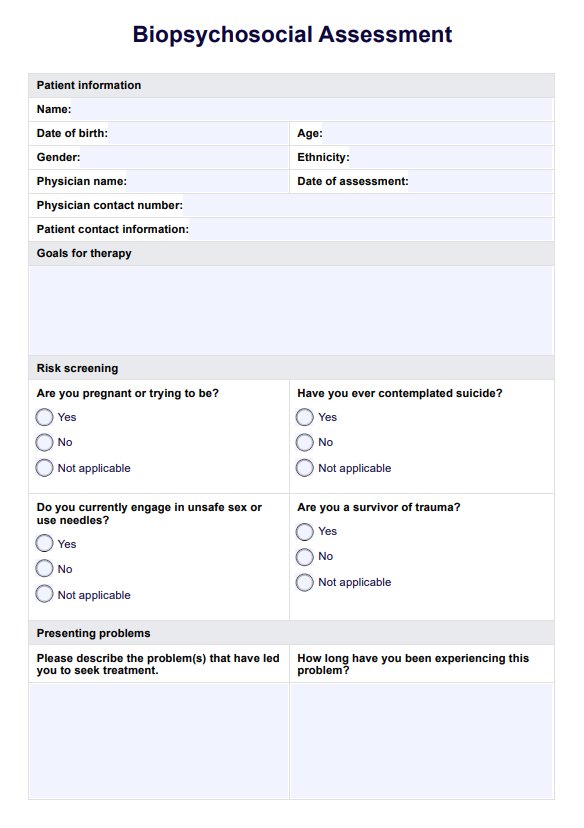
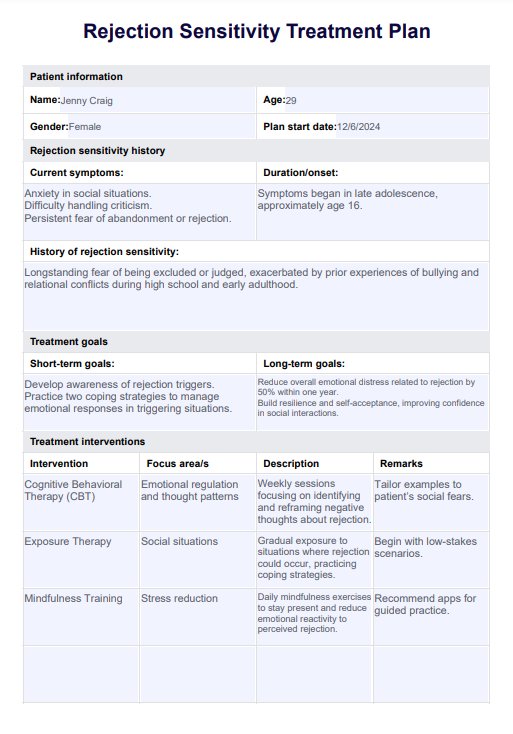
Rejection Sensitivity Treatment Plan Template
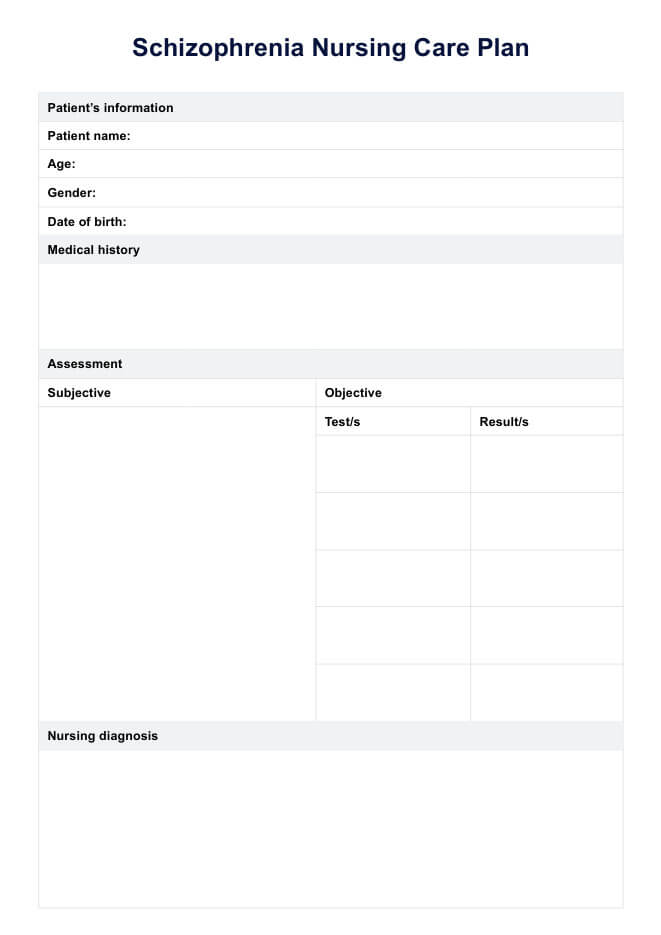
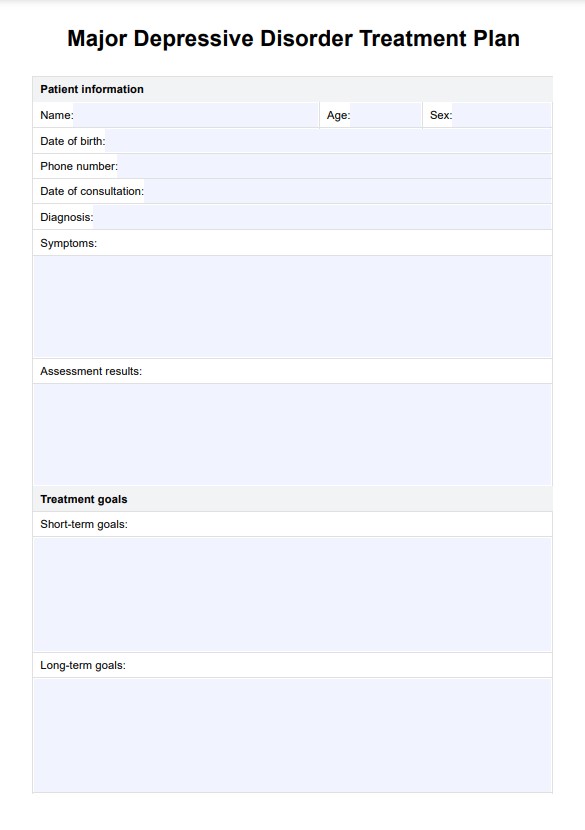
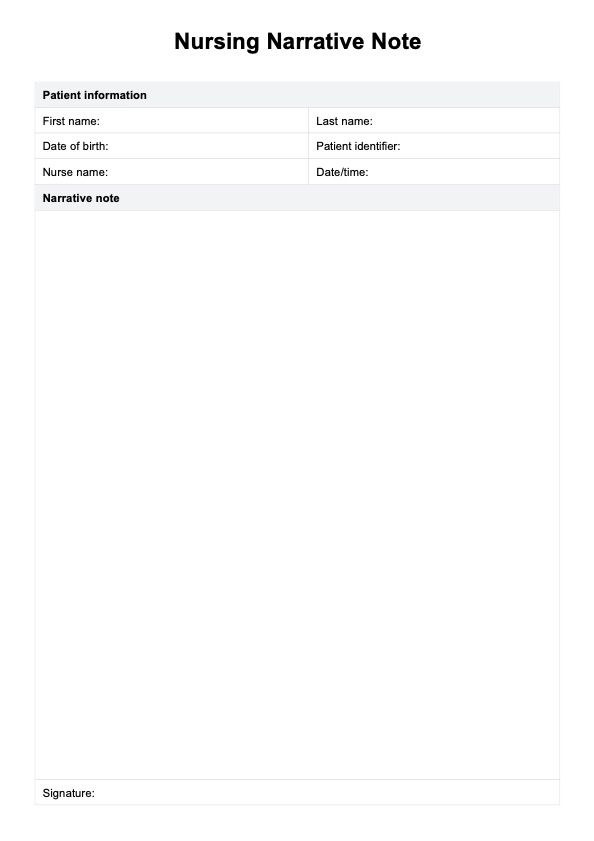
Rejection Sensitivity Treatment Plan Example
How to use our Rejection Sensitivity Treatment Plan
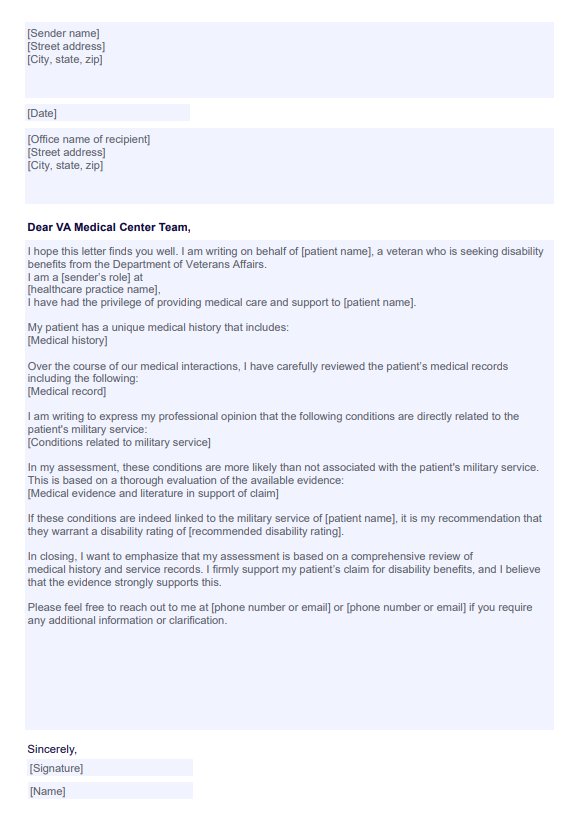
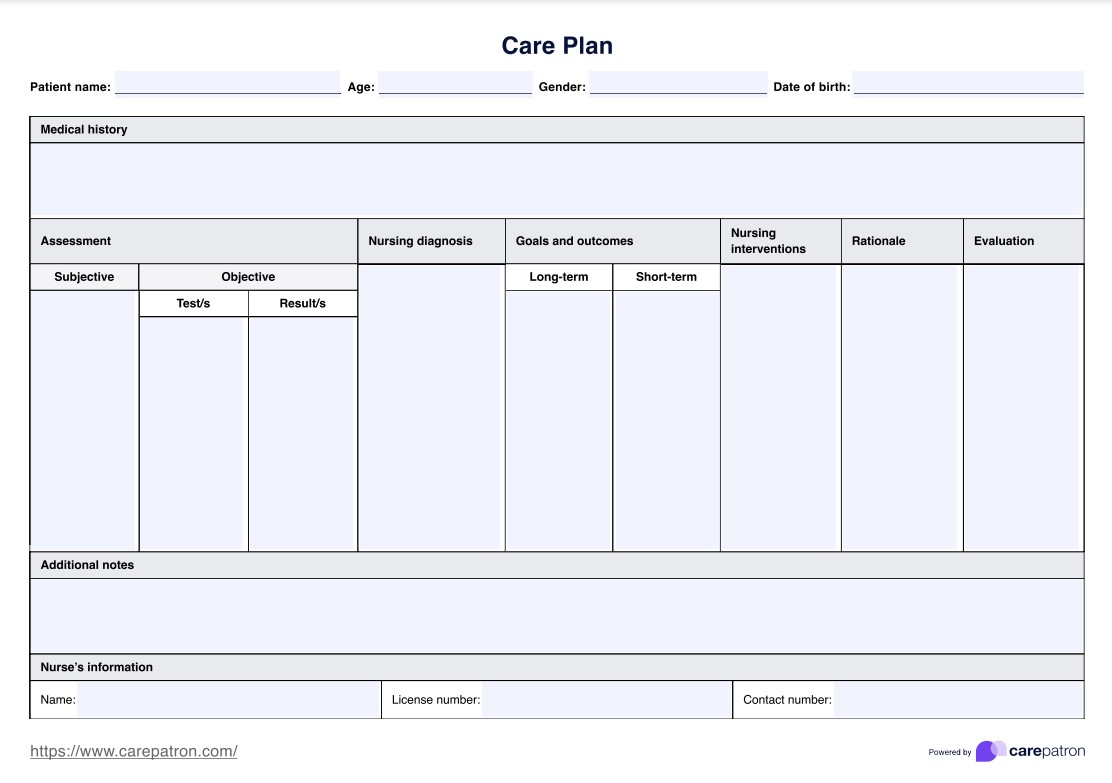
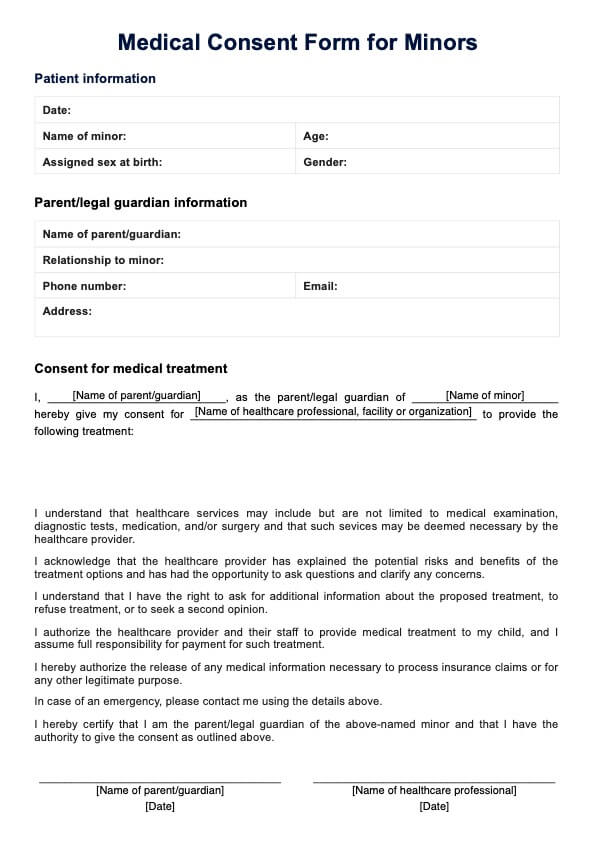
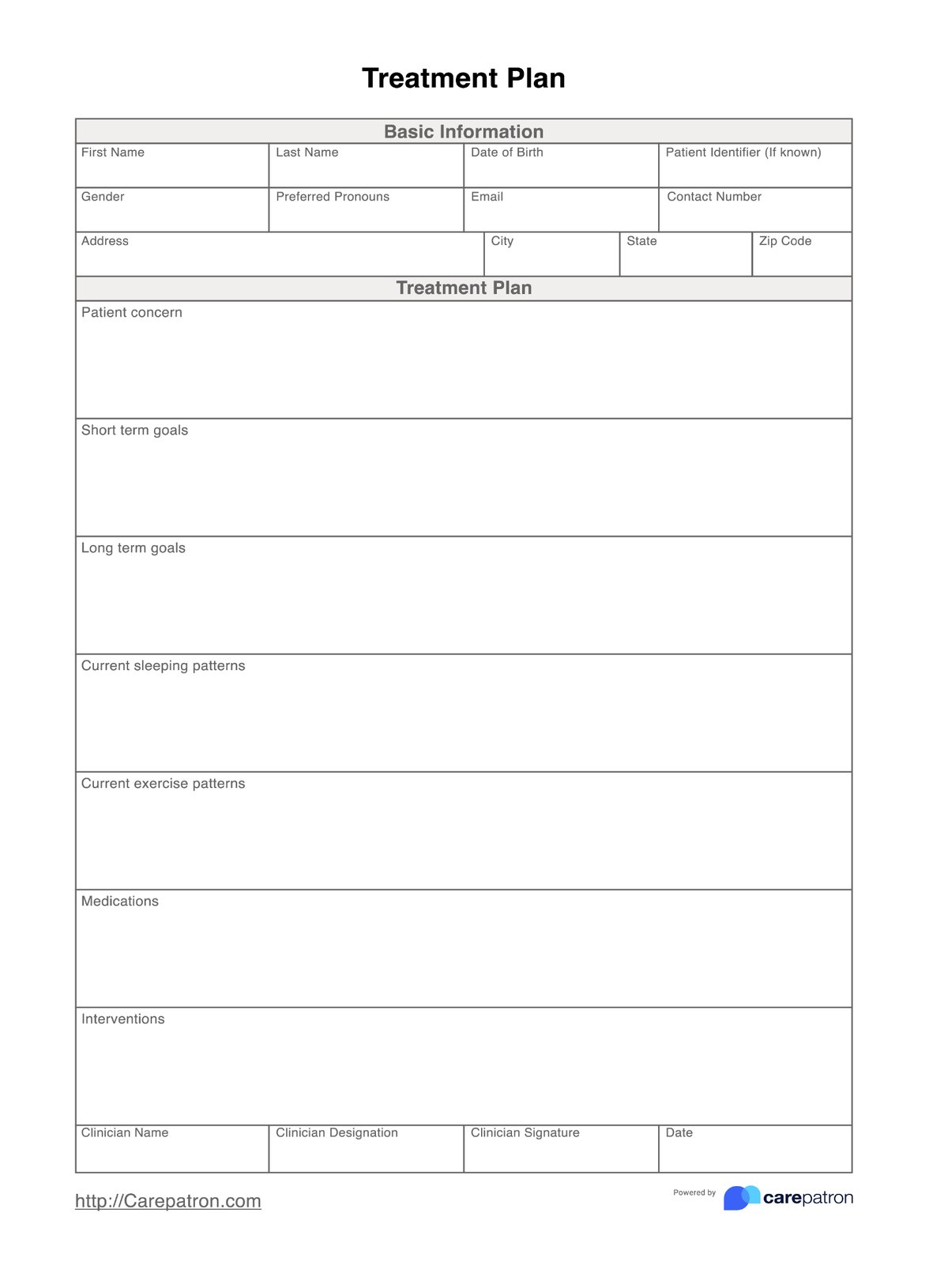
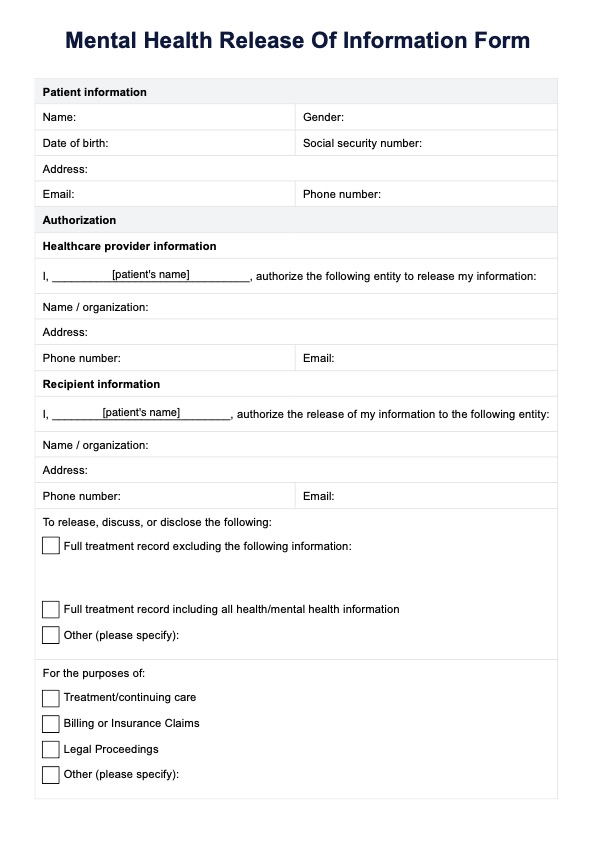
Our blank Rejection Sensitivity Treatment Plan makes it easier to identify and organize interventions, coping strategies, and medications to help your client effectively manage emotional responses to perceived rejection-sensitive dysphoria. Here's how to use it:
Step 1: Download the template
Get a copy of the Rejection Sensitivity Treatment Plan template by clicking "Use template." This lets you access the form and customize it via the Carepatron app. For a PDF version, choose "Download."
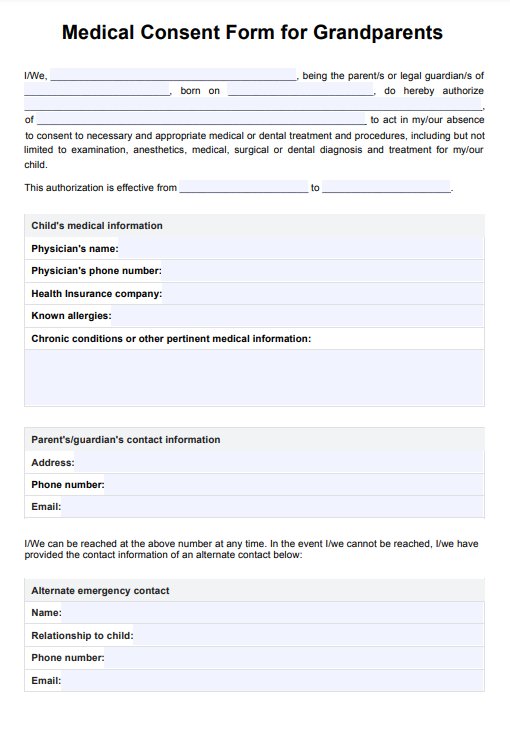
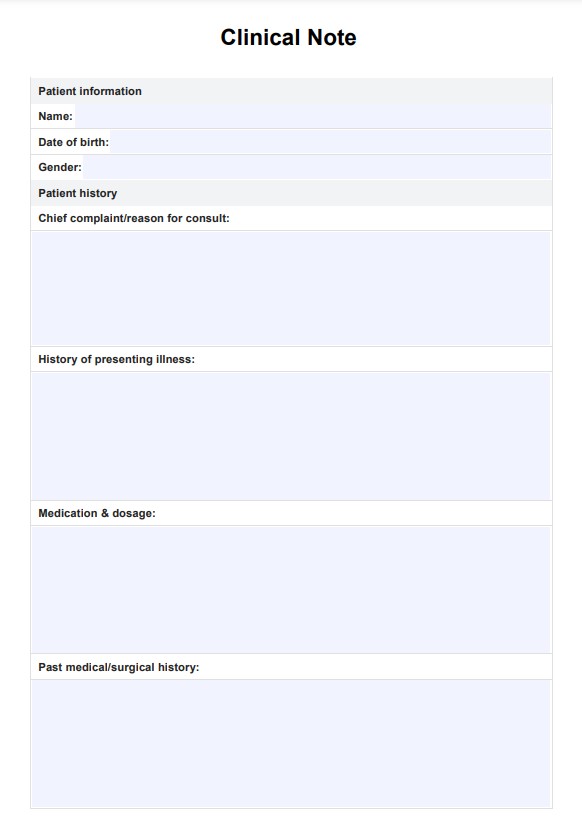
Step 2: Complete client information
Start by entering the client’s basic information at the top of the form, including their name, age, and gender. This ensures that each treatment plan is personalized and easily identifiable.
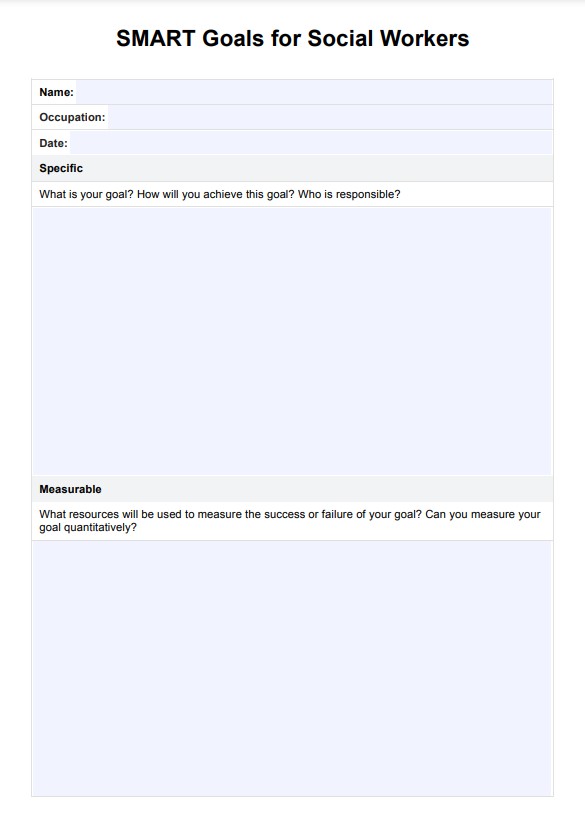
Step 3: Define treatment goals
Set clear, measurable treatment goals for both the short-term and long-term. These goals should address the client’s immediate needs, such as reducing emotional reactivity to perceived rejection, and focus on their longer-term growth, like improving overall emotional regulation or building resilience in social situations.
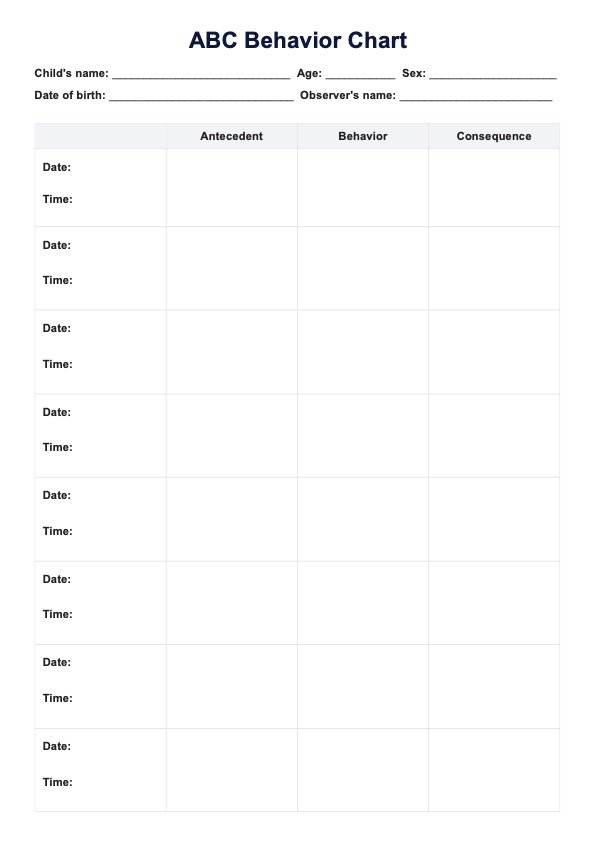
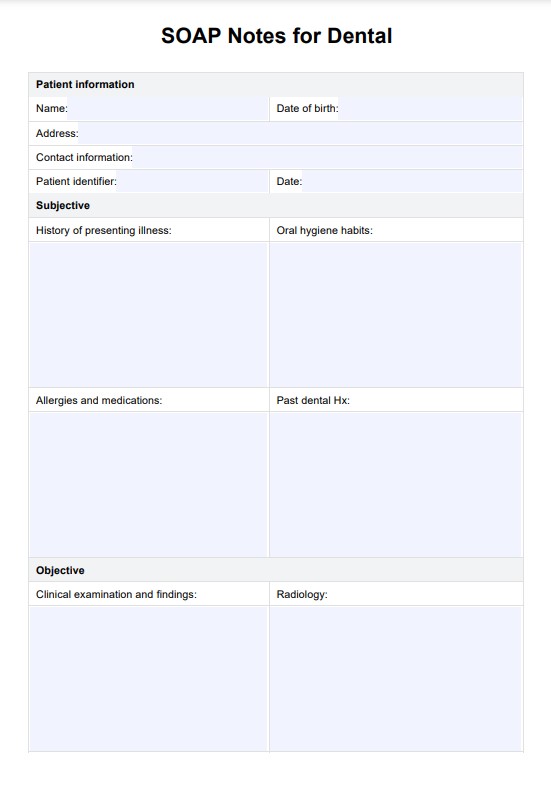
Step 6: Plan interventions
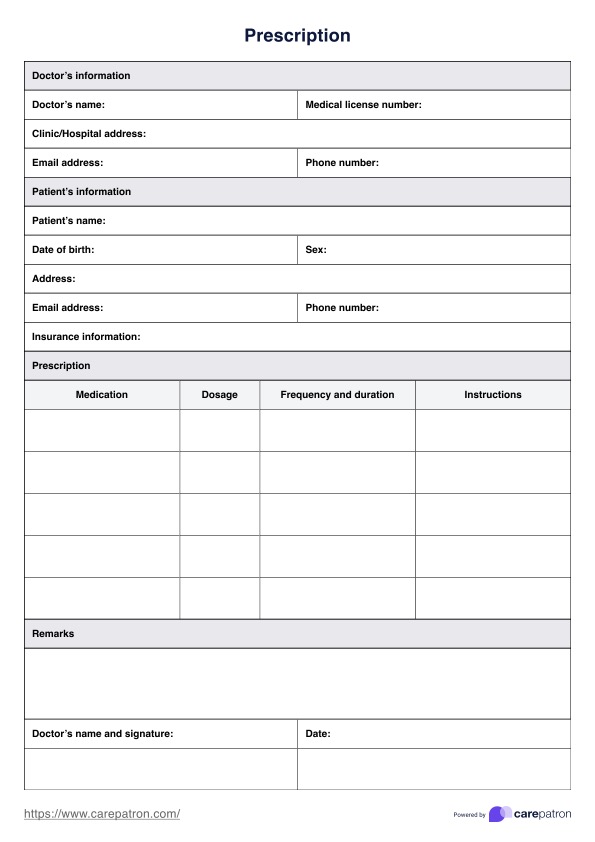
Use this section to outline the interventions you’ll be using. Depending on the client's needs, you may incorporate cognitive behavioral therapy (CBT), mindfulness-based approaches, emotion regulation techniques, or social skills training. Specify the strategies, exercises, or frequency of practice for each intervention, and, if relevant, include medication options that may support treatment.
Step 7: Identify coping strategies and medications
In this step, document the specific coping strategies taught to the client, such as relaxation techniques, grounding exercises, or journaling. Additionally, if applicable, note any medications prescribed to help manage symptoms of rejection sensitivity, such as antidepressants or mood stabilizers.
Step 8: Review and update the treatment plan regularly
The Rejection Sensitivity Treatment Plan is a dynamic document, and it should be reviewed and updated regularly based on the client’s progress. Schedule follow-up appointments to reassess treatment goals, evaluate the effectiveness of coping strategies, and discuss any challenges that may have emerged.
Rejection sensitivity treatment approaches
Treating rejection sensitivity, including RSD, focuses on reducing severe and intense emotional pain, improving emotional regulation, and addressing underlying mental health conditions such as ADHD or mood disorders. Effective approaches often combine psychotherapy, medication, and coping strategies tailored to individual needs.
Talk therapy, such as dialectical behavior therapy (DBT), helps manage intense emotional responses, negative thought patterns, and overwhelming feelings. It equips individuals with skills to reduce intense emotional response and distress, improve impulse control, and handle perceived criticism or rejection in social settings.
Medication, such as stimulant medications for ADHD or monoamine oxidase inhibitors (MAOIs), may alleviate symptoms by targeting brain structures involved in emotional intensity and stress response.
Developing coping strategies, including relaxation techniques, self-compassion practices, and emotional armor, can help individuals manage RSD symptoms, reduce sudden outbursts, maintain emotional control, and navigate social interactions. Treating rejection sensitivity enhances emotional well-being, promotes resilience, and supports healthier relationships in young adults and others with heightened sensitivity.
常見問題
To treat rejection-sensitive dysphoria (RSD), therapy like cognitive behavioral therapy (CBT) or dialectical behavior therapy (DBT) helps improve emotional regulation, medication addresses underlying ADHD or RSD symptoms, and coping strategies such as self-compassion and stress management build resilience.
Triggers include intense emotions or feelings of perceived or actual rejection, criticism, negative feedback, or social interactions that lead to overwhelming emotional reactions and evoke feelings of inadequacy or low self-esteem.
No, rejection-sensitive dysphoria (RSD) is not just trauma. While past trauma can contribute, RSD often stems from neurobiological factors, such as its links to attention deficit hyperactivity disorder (ADHD), emotional dysregulation, and heightened sensitivity.













-template.jpg)