Summary Discharges
Explore our guide on Summary Discharges. Understand the process, use our free template, and discover how effective discharge planning can improve patient care.


What is a Summary Discharge?
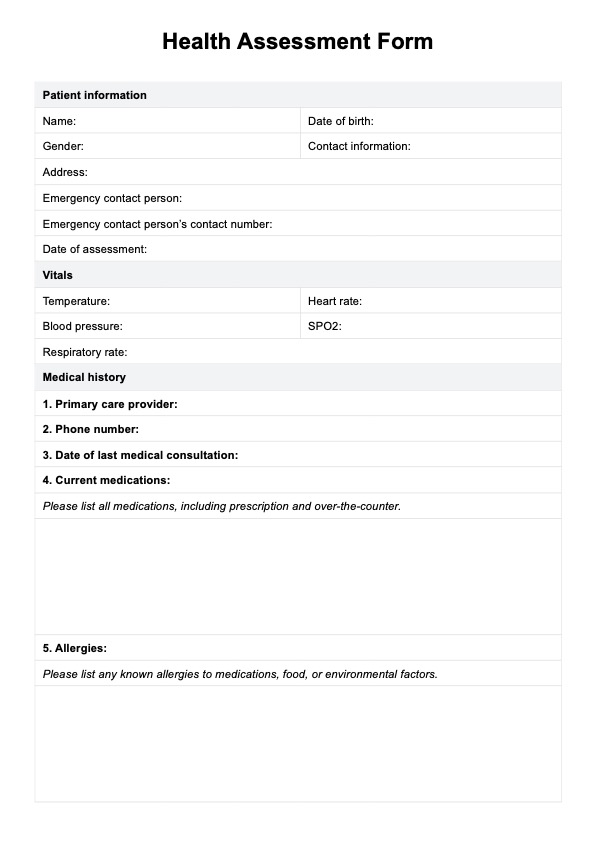
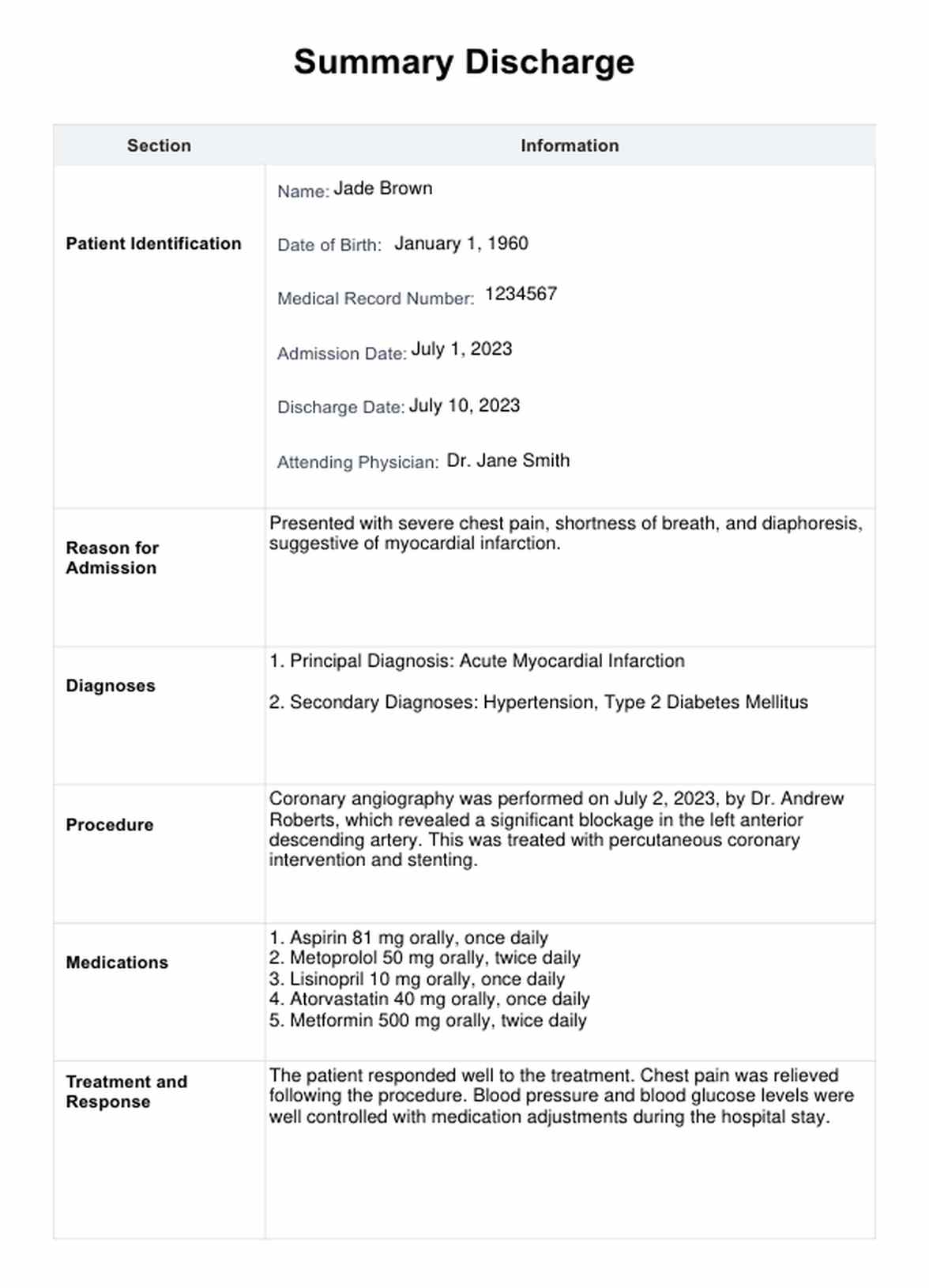
A Summary Discharge is a comprehensive clinical report prepared by a healthcare professional, typically a physician, nurse, or social worker, at the conclusion of a patient's hospital stay or a series of treatments. This document plays a critical role in the transition of care from the hospital to the home or another healthcare facility.
The Summary Discharge details essential components of the patient's healthcare journey, including their identification, reason for hospitalization, diagnoses, procedures performed, medications prescribed, and the patient's response to the treatment. It also outlines the patient's condition upon discharge and provides specific aftercare instructions.
The Summary Discharge is a communication bridge between the hospital care team and aftercare providers, ensuring continuity and care coordination. It also holds legal weight, with potential implications on patient care and outcomes if errors are made. Hence, timely and accurate completion of Summary Discharges is integral to efficient and effective healthcare delivery.
If you want access to an alternative Discharge Summary template, feel free to watch this video:
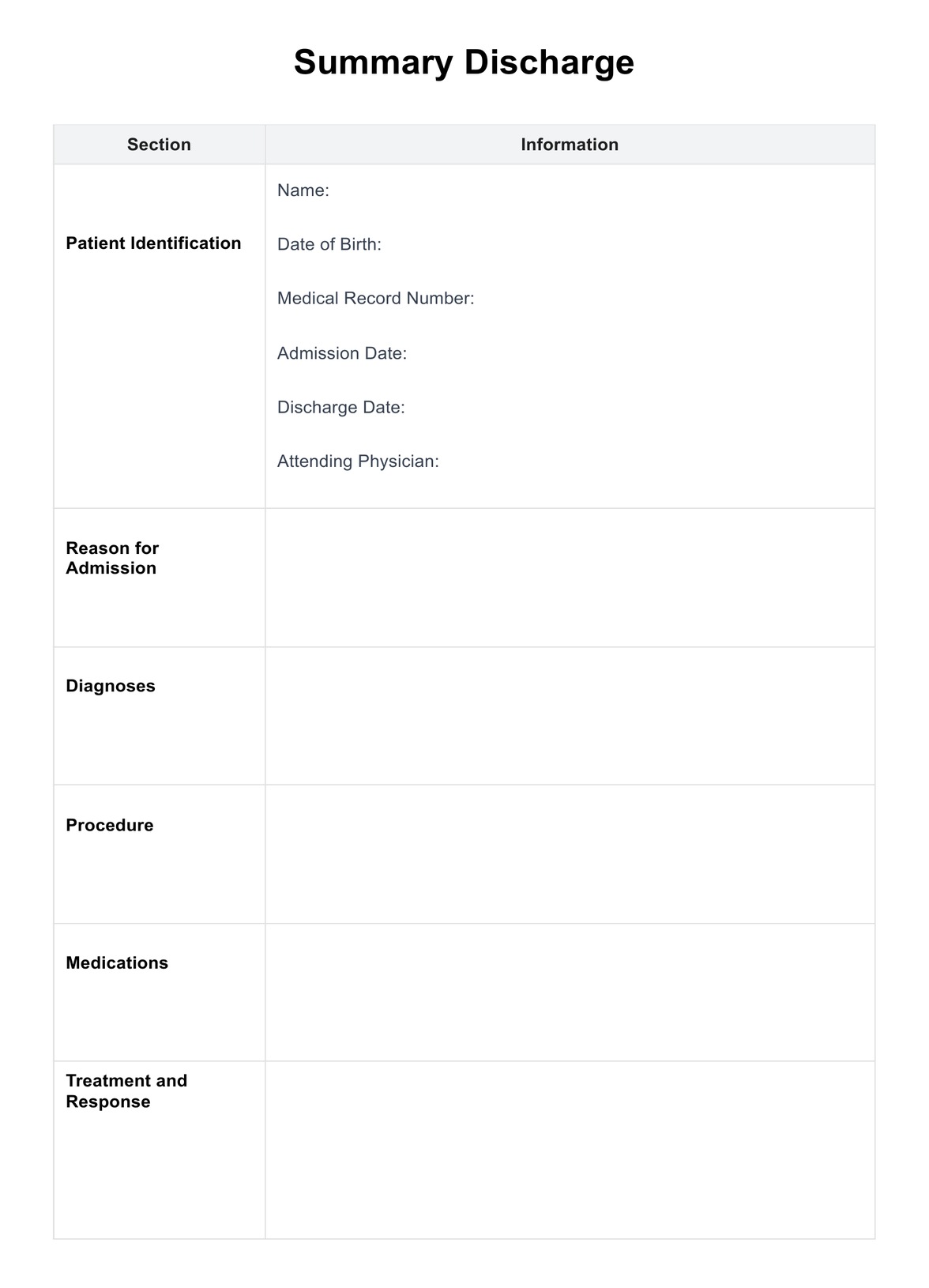
Summary Discharges Template
Summary Discharges Example
How does it work?
Creating a Summary Discharge is a structured process that requires attention to detail and a thorough understanding of the patient's healthcare journey. It involves several key steps, each contributing to the comprehensive summarization of the patient's hospital or healthcare facility stay.
Step 1: Gathering Information
The first step involves gathering all pertinent information about the patient. This includes details about their diagnoses, the procedures they underwent, the medications they received, and their response to the treatment. The patient's demographic details, dates of admission and discharge, and the attending physician's name are also collected.
Step 2: Structuring the Summary Discharge
In the second step, the information collected is arranged in a structured format. This typically includes distinct sections for patient identification, reason for admission, diagnoses, procedures, medications, treatment and response, condition at discharge, discharge instructions, and follow-up appointments.
Step 3: Writing the Summary Discharge
Once the structure is in place, the next step involves writing the Summary Discharge. The goal is to provide a clear and concise document that succinctly captures the patient's healthcare journey. Care should be taken to ensure that the information provided is accurate and that the language is understandable to all potential readers, including patients and their families.
Step 4: Reviewing and Finalizing
The final step is to review the document for completeness and accuracy. Any errors or omissions can impact patient care, making this a critical step. Once the document has been reviewed and all necessary edits are made, it is finalized and ready for distribution.
Our Printable Summary Discharges template simplifies these steps and ensures a standardized and thorough approach to creating Summary Discharges.
When would you use this Template?
A Summary Discharge template becomes indispensable in various clinical settings whenever a patient transitions from one level of care to another. Here are specific scenarios where this template would be handy:
Hospital Discharge
This is the most common scenario for utilizing a Summary Discharge document. A comprehensive discharge summary becomes necessary when a patient's hospital stay concludes, whether due to improvement, transfer to another facility, or a shift to home care. This summary records the course of treatment during the hospital stay, from diagnosis to therapy, and helps in the transition of care.
Outpatient Procedure or Surgery
After outpatient procedures or surgeries, a patient might not need an extended hospital stay. However, providing a detailed summary of what was done, any medications prescribed, and follow-up instructions are still crucial.
End of a Treatment Course
A Summary Discharge document is helpful in scenarios such as the conclusion of a series of physiotherapy sessions or the completion of a chemotherapy cycle. It can summarize the treatment provided, the patient's response, and any future care instructions.
Transfer to a Different Level of Care
When patients transition from acute care to subacute or long-term care facilities, a detailed Summary Discharge document ensures that the receiving facility has comprehensive information about the patient’s healthcare journey. This also applies to transitions between other care levels, from intensive care units to general wards.
Home Healthcare
If a patient receives home healthcare, the conclusion of the service period necessitates a Summary Discharge. This provides a detailed record of the services, the patient's response, and future recommendations.
The aim is to ensure a smooth transition of care, improve patient outcomes, and reduce readmission rates. This is why a Summary Discharge template is invaluable in any healthcare setting. It promotes consistency, ensures that all crucial information is included, and improves care continuity.
Benefits
Effective patient discharge is a crucial aspect of healthcare that directly impacts patient outcomes. Utilizing a well-designed Summary Discharge template can bring numerous benefits that elevate the standard of care, ensuring patient well-being while improving healthcare processes.
1. Streamlining the Discharge Process
The template helps standardize and streamline the discharge process. It ensures that all necessary information is collected and presented systematically, preventing omissions and miscommunications.
2. Facilitating Effective Communication
As a comprehensive document detailing a patient's journey through the hospital stay or treatment, the summary discharge serves as a valuable tool for communication between different healthcare providers, including the primary care doctor, specialists, and any post-acute care providers.
3. Improving Continuity of Care
The summary discharge provides critical information required for follow-up care, supporting continuity of care. Providing a detailed account of the hospital course, diagnoses, treatment, and follow-up instructions enables other healthcare providers to understand the patient's health status and provide appropriate care.
4. Reducing Readmissions
Research has shown that timely and accurate discharge summaries can reduce readmission rates. Patients and caregivers can manage health conditions more effectively at home by clearly outlining post-discharge care instructions and warning signs to watch out for.
5. Serving as a Legal Document
Besides its clinical importance, the summary discharge also serves as a legal document, providing a formal record of the patient's hospital stay and treatment. It can be an essential piece of evidence in any legal or compliance matters.
6. Free and Customizable
Our free Summary Discharge template is easy to use and highly customizable to suit the specific needs of various healthcare scenarios, offering flexibility and adaptability.
Commonly asked questions
Healthcare professionals use Summary Discharge, particularly those involved in a patient's discharge process.
Summary Discharge is used when a patient transitions from a healthcare facility to a home or another care setting.
Summary Discharge is a communication tool to summarize a patient's hospital stay, including diagnoses, treatment, and aftercare instructions. It facilitates continuity of care and reduces readmission risks.




















-template.jpg)