Foot Posture Index (FPI-6)
Measure the pronation or supination of a patient’s foot using the Foot Posture Index (FPI-6) to gauge how it can negatively impact their movement.


What is the Foot Posture Index (FPI-6)?
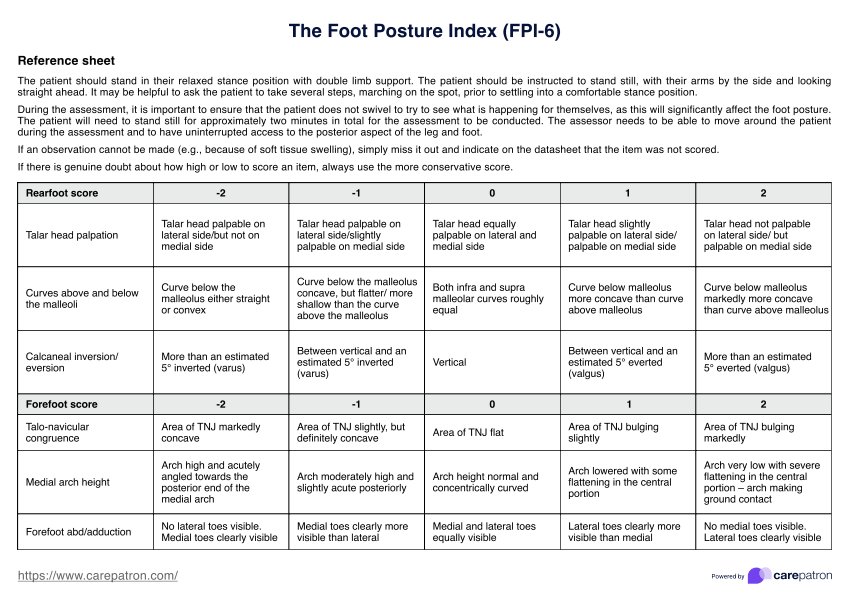
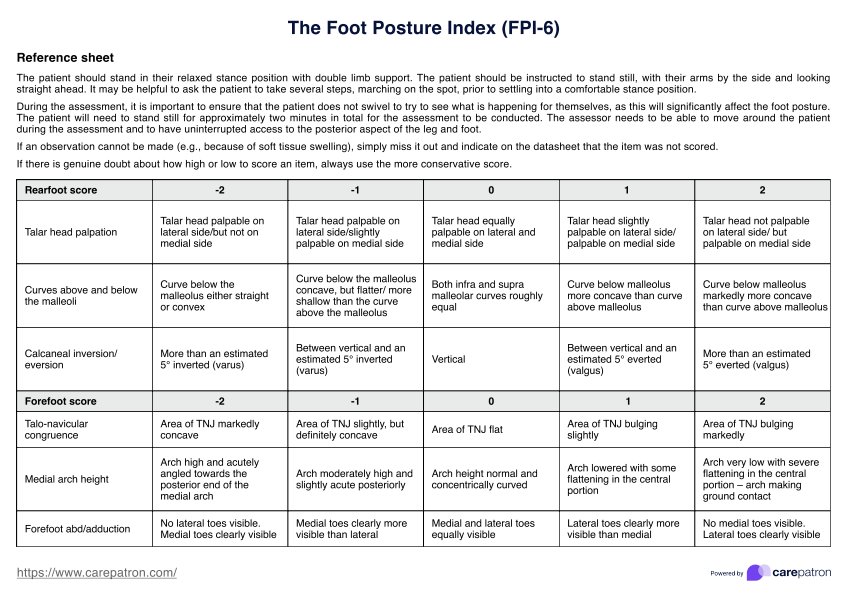
The Foot Posture Index (FPI-6) is a novel rating system tool for evaluating standing foot posture in clinical and research settings. It assesses both the rear and forefoot, comprehensively evaluating overall foot position and alignment.
Unlike traditional measures, which often require specialized equipment, the FPI-6 offers a simple, reliable method for scoring standing foot posture using visual and manual assessments. Morrison and Ferrari (2009) also found it a reliable method for assessing the foot in children and adolescents.
The evaluation is conducted while the patient stands comfortably, with both feet supporting their weight evenly. Patients are instructed to stand still, keep their arms at their sides, and look straight ahead to ensure an accurate assessment. This dynamic but structured evaluation helps identify foot type and determine potential risk factors associated with abnormal foot mechanics.
FPI-6 criteria for assessment
The FPI-6 consists of six observational criteria, each scored on a scale from -2 to +2, where negative values indicate a supinated foot posture, positive values indicate a pronated foot posture, and scores closer to zero represent a neutral alignment (Redmond et al., 2006):
- Talar head palpation: Assesses the prominence of the talar head. If the talar head is more palpable on the lateral side, it suggests a supinated foot posture, whereas prominence on the medial side indicates a pronated foot posture.
- Curvature above and below the malleoli: Examines the concavity of the curves above and below the lateral malleolus. A more pronounced concavity below the malleolus is associated with a pronated foot, while a straighter or convex shape suggests supination.
- Calcaneal inversion/eversion: Evaluates the alignment of the heel bone (calcaneus) relative to a vertical position. An inverted heel (tilted inward) indicates supination, while an everted (tilted outward) heel suggests pronation.
- Talo-navicular joint (TNJ) congruence: Observes the shape and contour of the TNJ area. A more concave TNJ suggests supination, whereas a bulging TNJ indicates pronation.
- Medial longitudinal arch height: Measures the height and shape of the foot’s arch. A high, sharply angled arch suggests supination, while a low, flattened arch is characteristic of pronation.
- Forefoot abduction/adduction: Assesses the visibility of the toes from a posterior view. If the medial toes (big toe side) are more visible, the foot is adducted, indicating supination. If the lateral toes (little toe side) are more prominent, the foot is abducted, indicating pronation.
As mentioned, the FPI-6 helps practitioners assess static foot posture, determine risk factors, and guide interventions for patients with gait abnormalities or lower limb discomfort.
However, modifications to the cutoff values may be necessary when screening for supinated feet, as the FPI-6 has limitations in identifying high-arched individuals (Teyhen et al., 2011). It is important for clinicians to consider this when diagnosing foot-related issues and planning treatment strategies.
Check out this video on our Foot Pain Chart to see how similar assessments are performed:
Foot Posture Index (FPI-6) Template
Foot Posture Index (FPI-6) Example
How to use our Foot Posture Index (FPI-6) template
Carepatron has created a free and easy-to-use FPI-6 template, including a reference sheet and a data sheet for easy clinical documentation. Follow these steps to get started:
Step 1: Download the form
Click the "Use template" button to access the Foot Posture Index template via the Carepatron app. For a PDF version, you can also click "Download."
Step 2: Introduce to your patient
Explain the purpose of this modified Foot Posture Index assessment to your patient, emphasizing its role in evaluating their foot posture and identifying any imbalances contributing to discomfort or musculoskeletal issues. Ensure they stand naturally and relaxed before proceeding with the assessment.
Step 3: Assess the six criteria
Using the reference sheet included in the template, systematically evaluate each of the six FPI-6 criteria while the patient is in a standing position. Assign a score to each criterion based on the observed foot posture.
Step 4: Record the scores
Enter the assigned scores into the data sheet provided in the template. The total score will help classify the patient’s foot posture.
Step 5: Interpret results and discuss with the patient
Review the final classification and discuss its implications with the patient. If necessary, provide recommendations for further evaluation, footwear modifications, or treatment plans based on the assessment.
Step 6: Save and update records
Store the completed form securely in the Carepatron app for easy reference and follow-up assessments. If needed, update the patient’s records to track changes in foot posture and treatment outcomes.
Scoring and interpretation
As mentioned, each of the six Foot Posture Index criteria is scored on a 5-point scale, ranging from -2 to +2. Negative scores indicate a more supinated foot posture, while positive scores indicate a more pronated foot posture.
The scores from all six criteria are summed to yield a composite score ranging from -12 to +12. This total score is then used to classify foot posture as follows (Terada et al., 2014):
- Normal: 0 to +5
- Pronated: +6 to +9
- Highly pronated: 10+
- Supinated: -1 to –4
- Highly supinated: –5 to -1
A more negative total score suggests a supinated foot posture, while a more positive score indicates a pronated foot posture.
What are the benefits of using the Foot Posture Index (FPI-6)?
The FPI-6 is a valuable tool in clinical practice for assessing foot position and classifying foot posture type. It provides an easy, inexpensive, and reliable way to evaluate standing foot posture without requiring specialized equipment. This makes it particularly useful for identifying foot type, assessing injury risk factors, and guiding treatment strategies.
Below are some key benefits of using the FPI-6 in a clinical setting.
A cost-effective and accessible assessment tool
The FPI-6 provides a simple yet effective method for evaluating static foot posture without requiring specialized equipment. You can conduct the assessment through direct observation, making it an accessible tool in various clinical settings. Despite its simplicity, the FPI-6 offers valuable insights into foot alignment and potential musculoskeletal risks.
Aids in diagnosis and treatment planning
By assessing both rearfoot and forefoot posture, the FPI-6 helps you determine whether additional evaluations, such as imaging or gait analysis, are necessary. The results serve as a foundation for developing targeted treatment strategies through manual therapy, orthotics, footwear recommendations, or rehabilitation exercises.
Supports injury prevention and rehabilitation
Identifying excessive pronation or supination early can help prevent musculoskeletal injuries, such as plantar fasciitis, Achilles tendinopathy, or shin splints. The FPI-6 also helps monitor patients undergoing rehabilitation by tracking changes in foot posture over time, allowing clinicians to adjust interventions as needed.
Enhances clinical decision-making and long-term monitoring
The structured approach of the FPI-6 allows you to make informed decisions regarding patient care, risk assessment, and treatment effectiveness. By using the tool for periodic reassessments, clinicians can objectively measure progress and refine interventions to optimize patient outcomes.
Improves patient education and engagement
The FPI-6 benefits clinicians and enhances patients' understanding of their foot posture and its impact on overall musculoskeletal health. By visually demonstrating assessment results and explaining their implications, healthcare professionals can engage patients in their treatment plans.
References
Morrison, S. C., & Ferrari, J. (2009). Inter-rater reliability of the foot posture index (FPI-6) in the assessment of the paediatric foot. Journal of Foot Ankle Res(1). https://doi.org/10.1186/1757-1146-2-26
Redmond, A. C., Crosbie, J., & Ouvrier, R. A. (2006). Development and validation of a novel rating system for scoring standing foot posture: The foot posture index. Clinical Biomechanics, 21(1), 89–98. https://doi.org/10.1016/j.clinbiomech.2005.08.002
Terada, M., Wittwer, A. M., & Gribble, P. A. (2014). Intra‐rater and inter‐rater reliability of the five image‐based criteria of the foot posture index‐6. International Journal of Sports Physical Therapy, 9(2), 187. https://pmc.ncbi.nlm.nih.gov/articles/PMC4004124/
Teyhen, D. S., Stoltenberg, B. E., Eckard, T. G., Doyle, P. M., Boland, D. M., Feldtmann, J. J., McPoil, T., Christie, D. S., Molloy, J. M., & Goffar, S. L. (2011). Static foot posture associated with dynamic plantar pressure parameters. Journal of Orthopaedic & Sports Physical Therapy, 41(2), 100–107. https://doi.org/10.2519/jospt.2011.3412
Commonly asked questions
A normal Foot Posture Index (FPI-6) score ranges from 0 to +5, indicating a balanced foot posture without excessive pronation or supination. This suggests the foot maintains a neutral alignment, distributing weight efficiently during standing and movement. Scores outside this range may indicate a need for further assessment and possible intervention.
The six criteria assessed in the Foot Posture Index (FPI-6) are talar head palpation, curvature above and below the malleoli, calcaneal inversion/eversion, talo-navicular joint (TNJ) congruence, medial longitudinal arch height, and forefoot abduction/adduction. Each criterion is scored from -2 to +2, helping to classify the foot as supinated, neutral, or pronated.
In foot and ankle research, the Foot Posture Index (FPI-6) is widely used for assessing foot posture. To use the FPI-6, a healthcare professional observes a patient’s standing foot posture while they are in a comfortable stance position. Each of the six criteria is assessed and assigned a score, which is then summed to classify the foot posture as supinated, normal, or pronated. This information helps identify foot type, assess risk factors, and guide treatment decisions in clinical settings.
















-template.jpg)