Discharge Plan Template
Discover a comprehensive Discharge Plan Template to guide your patient's transition from the hospital. Download a free PDF example to get started.


What is hospital discharge planning?
Discharge planning is an essential aspect of patient care that aims to create a seamless transition for patients from the hospital setting to their next recovery phase. This process involves collaboration among health care professionals, hospital staff, the patient, and their family members to develop a comprehensive plan that addresses the patient's medical needs, functional abilities, and available support systems.
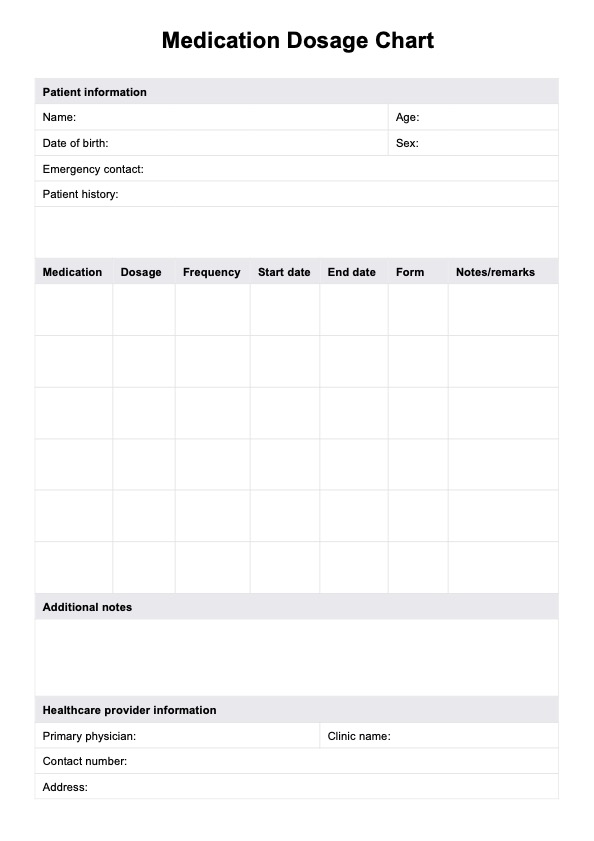
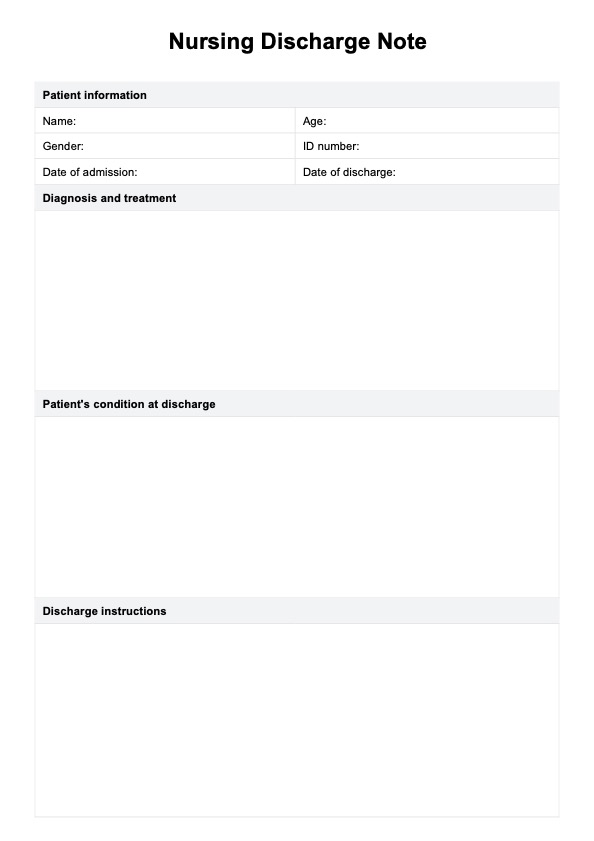
A discharge plan includes medication management, required medical equipment and supplies, home health services, follow-up appointments, and education for the patient and their caregivers. Part of discharge planning is the discharge summary, essential for communicating with other healthcare providers about what transpired during the patient's hospital stay.
Discharge planning reduces the risk of complications and hospital readmissions and helps patients receive appropriate care during their recovery. Home health agencies are crucial in coordinating necessary services post-discharge to ensure a smooth recovery process.
A well-executed discharge plan also empowers patients and their caregivers with discharge instructions and resources they need to manage their recovery effectively.
In summary, good discharge planning is essential in ensuring patients receive coordinated, high-quality care as they transition from the hospital to their home or another healthcare facility.
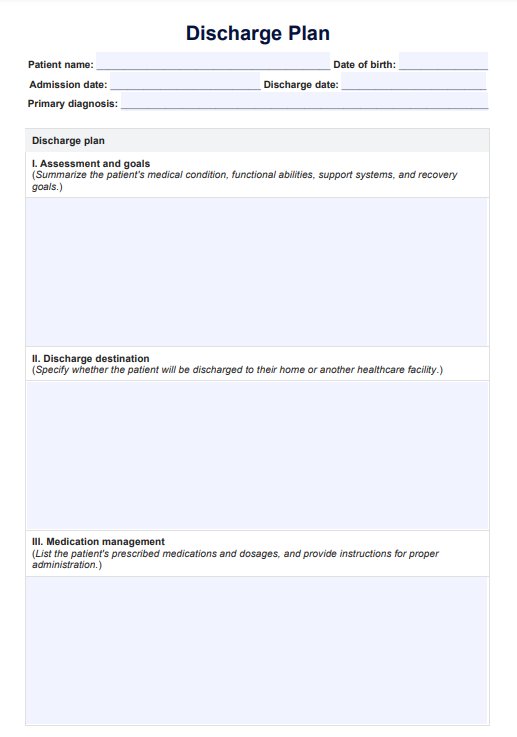
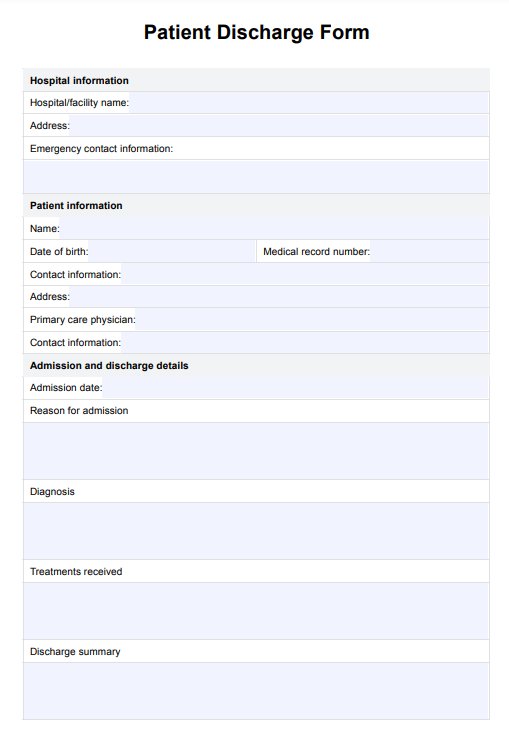
Discharge Plan Template
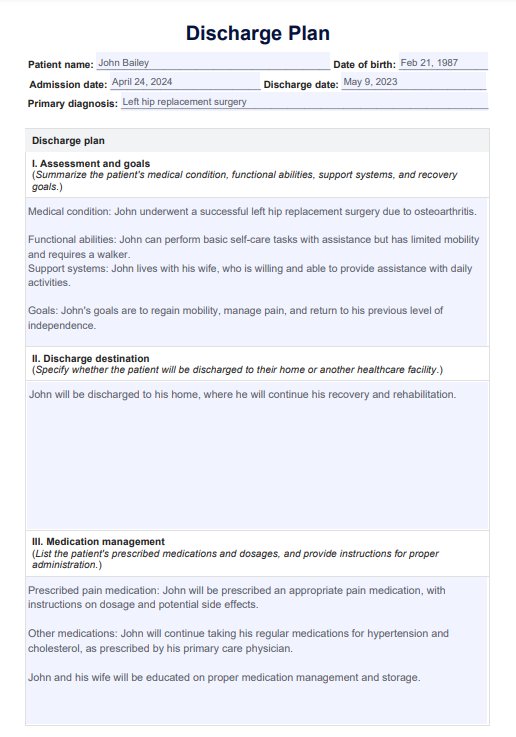
Discharge Plan Template Example
How does it work?
A discharge plan is a roadmap for a patient's transition from the hospital to their home or another healthcare facility. In this section, we will delve into the critical steps involved in creating a successful discharge plan.
Step 1: Download the template
Download the Discharge Plan Template, fill out patient details, assess the patient's medical condition, functional abilities, and support systems, and establish recovery goals. We've also included a discharge plan example for your reference.
Step 2: Fill out the discharge plan
Start by determining if the patient will be discharged to their home or another healthcare facility. List all medications, dosages, and administration instructions while educating the patient and caregivers about proper medication management. Next, identify and provide the necessary medical equipment, assistive devices, and supplies required for recovery.
Outline the types and frequency of home health services needed, such as nursing care and physical therapy. Schedule follow-up appointments with health care providers and establish clear communication protocols among all healthcare professionals involved.
Step 3: Educate the patient and store the plan
Finally, the patient and caregivers should receive comprehensive education on proper care for a successful recovery. Organize and securely keep all documentation related to the patient's care. This ensures easy access for future reference.
When would you use this template?
A Discharge Plan Template is an indispensable tool for healthcare practitioners like nurses, doctors, case managers, and social workers who are critical in managing a patient's transition from the hospital to their home or another healthcare facility. Utilizing a Discharge Plan Template becomes especially crucial in the following situations:
Patients with complex medical conditions
For patients with multiple comorbidities, chronic diseases, or those recovering from major surgeries, a well-structured discharge plan is essential to address the various aspects of their care and support during recovery.
Elderly or frail patients
Older adults or patients with frailty may require additional support and assistance in managing their daily activities and medical care. A comprehensive discharge plan ensures their unique needs are met during the transition.
Patients with limited support systems
For patients with limited or no support from family or friends, a discharge plan can help coordinate the necessary services and resources, such as home health care or community-based support programs, to ensure their well-being and safety after hospitalization.
Transitions to other healthcare facilities
A detailed discharge plan outlines the needed services when patients require ongoing care at a rehabilitation center, skilled nursing facility, or long-term care facility. It ensures continuity of care during the transfer.
Patients with mental health conditions
Discharge planning for mental health conditions involves coordinating care with mental health professionals and ensuring appropriate support for the patient and their caregivers.
Healthcare practitioners can effectively document and communicate all necessary information about a patient's care and recovery using a Discharge Plan Template. This ensures a smooth transition from the hospital to the next phase of their recovery, reduces the risk of complications, and improves patient outcomes.
Benefits of this discharge plan
Using a Discharge Plan Template is vital in transitioning patients from the hospital to their home or another healthcare facility. A well-structured template not only ensures that all necessary information is documented and easily accessible but also provides a framework for a seamless patient experience.
This section will explore the various benefits of using a Discharge Plan Template and highlight its importance in improving patient care and outcomes.
Streamlines the discharge planning process
A template simplifies creating a comprehensive discharge plan, ensuring all essential elements are considered and documented efficiently.
Reduces the risk of complications and hospital readmissions
By providing a clear outline of the patient's care needs, a Discharge Plan Template helps reduce the likelihood of complications and hospital readmissions, ultimately improving patient outcomes.
Ensures proper communication and collaboration among the care team
A Discharge Plan Template facilitates effective communication and collaboration among healthcare providers, patients, and their families, ensuring everyone is on the same page regarding the patient's care.
Provides clear guidance for patient and caregiver education
With a well-designed template, healthcare providers can easily educate patients and their caregivers on managing medical conditions, medications, and follow-up care, empowering them to participate actively in their recovery.
Facilitates continuity of care during the transition from hospital to home or another healthcare facility
A Discharge Plan Template helps patients receive appropriate care and support during their transition, enhancing their overall well-being and recovery.
It's customizable and easy to use
Discharge Plan Templates can be tailored to suit individual patient requirements, allowing healthcare providers to create personalized plans catering to each patient's needs and recovery goals.
Commonly asked questions
Discharge plans are typically used by healthcare professionals, such as nurses, doctors, case managers, and social workers, to facilitate a patient's transition from the hospital to their home or another healthcare facility.
A Discharge Plan Template is used when creating a comprehensive discharge plan for patients, particularly those with complex medical conditions or requiring additional care and support after leaving the hospital.
The frequency of updating a discharge plan form depends on the patient's medical condition, progress, and any changes in their care needs. Reviewing and updating the discharge plan is essential to ensuring appropriate care and support are provided during the patient's recovery.






















-template.jpg)