Dementia System Disorder
Download and use Carepatron's free Dementia System Disorder Template to assess dementia in patients properly.


What is dementia system disorder?
Dementia system disorder, also called major neurocognitive disorder, encompasses a range of symptoms associated with cognitive decline. This often manifests as memory loss, difficulty with problem-solving, and challenges in language comprehension (Emmady et al., 2022). These dementia symptoms are not just signs of normal aging; they represent a significant reduction in cognitive abilities, impacting daily activities and quality of life. The disorder is typically triggered by damage to brain cells and tissue, adding risk factors to communication between nerve cells and leading to behavioral symptoms like mood swings and personality changes.
Risk factors for developing dementia include age, with a higher prevalence in those 65 and older (World Health Organization, 2023), and lifestyle factors such as smoking, excessive alcohol consumption, and poor diet. Medical conditions like hypertension, diabetes, and obesity can also develop dementia. Despite these risks, dementia symptoms vary widely; some individuals experience mild cognitive impairment that may progress to more severe forms of dementia, including Alzheimer’s disease, vascular dementia, and Lewy body dementia.
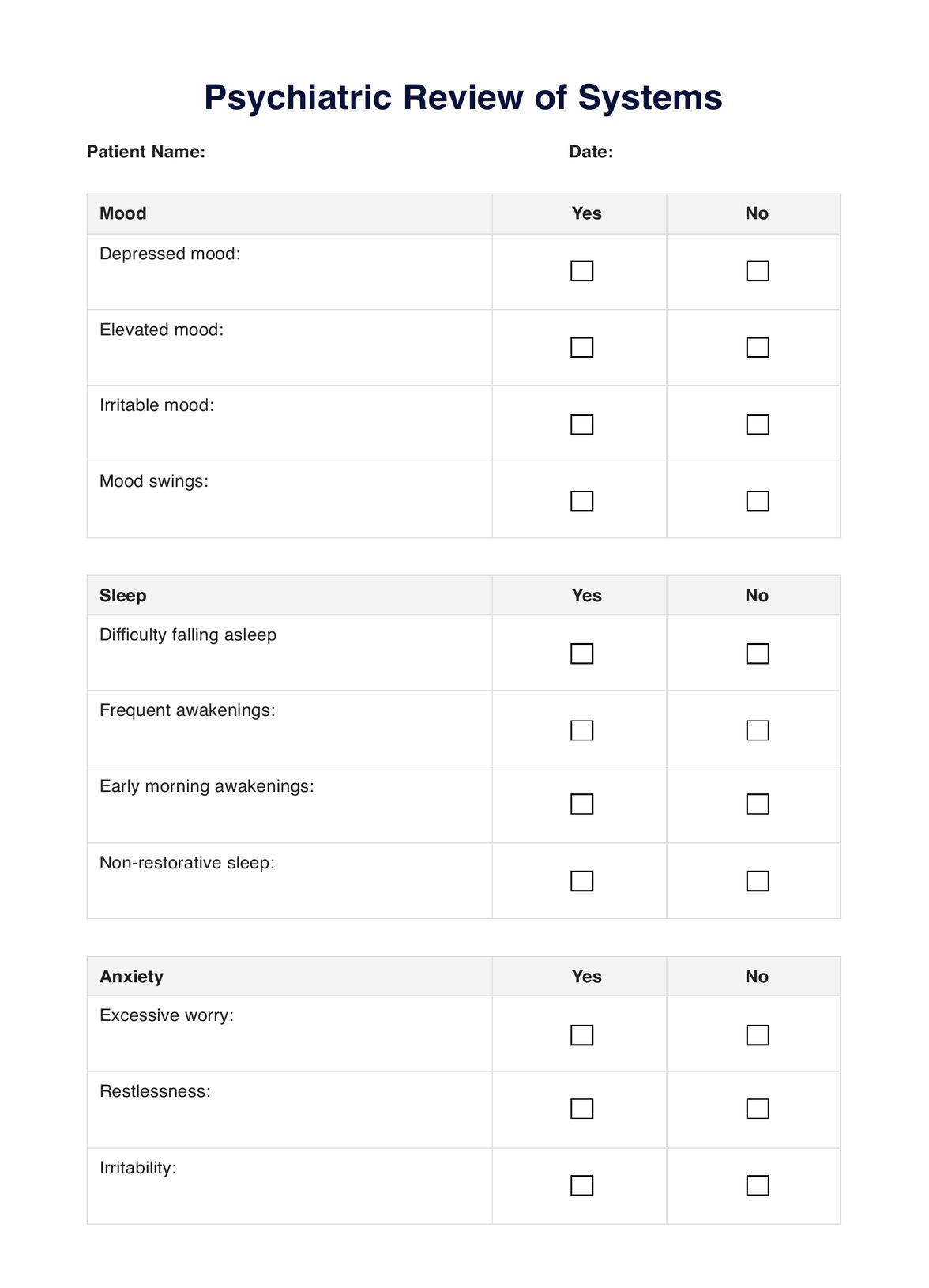
Dementia System Disorder Template
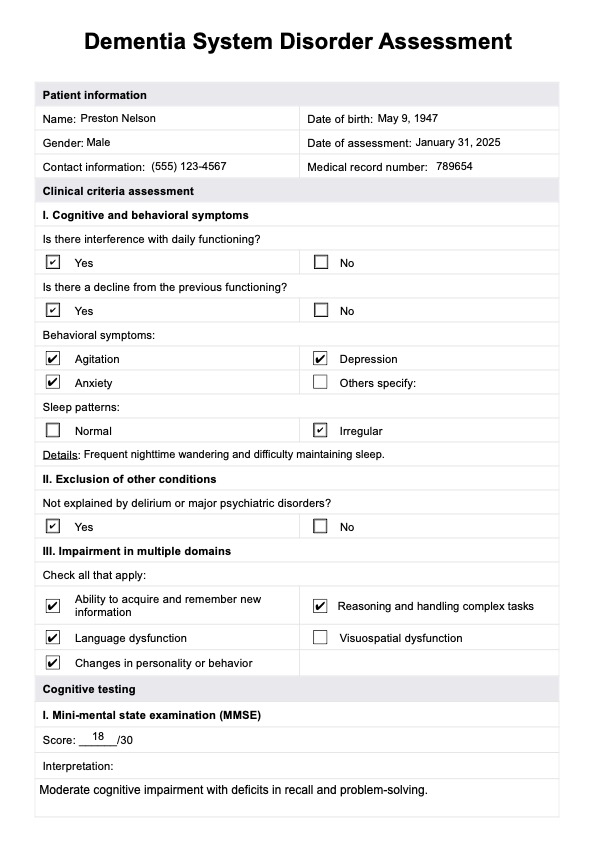
Dementia System Disorder Example
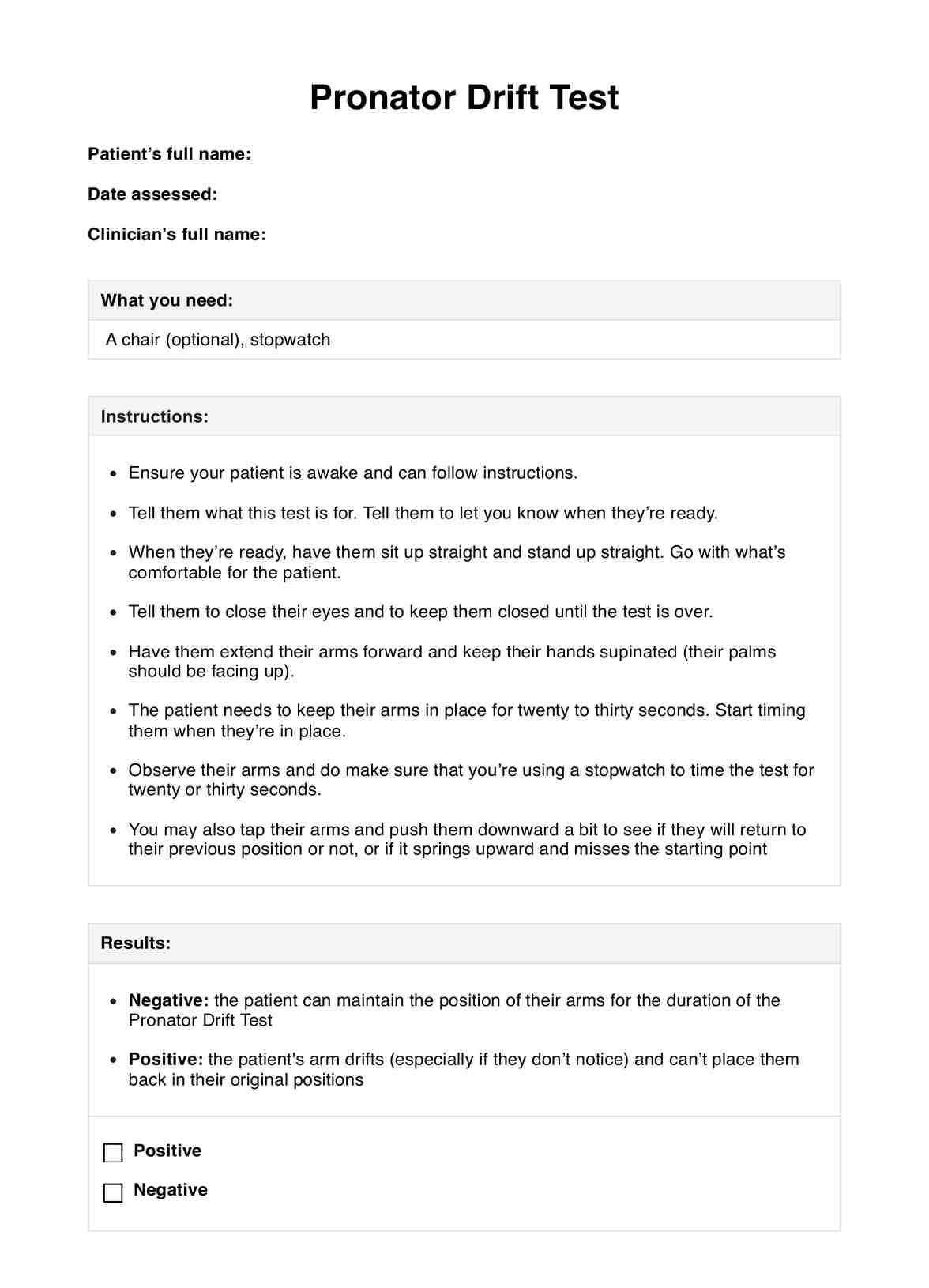
How does our Dementia System Disorder Template work?
Carepatron's Dementia System Disorder Template streamlines the assessment process, enhancing the efficiency and accuracy of dementia evaluations. Here is how medical professionals can use this template in their work process.
Step 1: Access and use the template
Click "Use template" to open and customize the Dementia System Disorder Template in the Carepatron app. The template is easy to modify, featuring fillable tables and a sample plan for everyday use, providing a practical tool for clinical assessments.
Step 2: Introduce the assessment to the patient
Explain the purpose and process of the assessment to the patient, ensuring they understand what to expect. This step helps build trust and make the patient comfortable with the procedure.
Step 3: Conduct the assessment of the patient
Carry out the detailed assessment as guided by the template. This involves observing and recording cognitive and behavioral symptoms and conducting cognitive tests provided within the template.
Step 4: Gather and interpret the results
After completing the assessment, gather all the data and analyze the results to determine the cognitive state and potential type of dementia. This analysis is critical to diagnosing dementia.
Step 5: Provide patient education and next steps
Inform the patient of the assessment results and discuss the potential next steps. Provide education on dementia management and plan further interventions or referrals as necessary, ensuring the patient feels supported throughout the process.
Types of dementia
Dementia encompasses a range of conditions characterized by the deterioration of brain function, manifesting in cognitive decline and impacting daily life. These conditions are typically progressive and affect memory, behavior, and cognitive abilities.
Alzheimer's disease
Alzheimer's disease is marked by progressive memory loss and cognitive decline due to amyloid plaques and tau tangles in the brain (Kumar et al., 2024). It is the most common form of dementia, causing significant changes in brain tissue and function.
Vascular dementia
As a result of decreased blood flow to the brain, vascular dementia can follow a stroke or other vascular incidents (Vijayan & Reddy, 2016). This form often correlates with other health issues like hypertension, and its symptoms vary depending on the affected brain areas.
Lewy Body dementia
This type involves deposits of Lewy bodies in the brain, affecting brain and nervous system functions (National Institute on Aging, 2021). Patients may experience visual hallucinations, cognitive fluctuations, and motor dementia-like symptoms similar to Parkinson’s disease.
Frontotemporal dementia
Frontotemporal dementia primarily impacts the frontal and temporal lobes, affecting personality, behavior, and language (National Institute on Aging, 2021). It often develops in younger patients and progresses differently than other dementias.
Younger onset dementia
Dementia diagnosed before the age of 65 is classified as younger-onset dementia (Loi et al., 2021). It includes any dementia, presenting unique challenges due to its early occurrence.
Alcohol-related dementia
Often reversible with alcohol abstinence, alcohol-related dementia stems from chronic excessive alcohol use, leading to cognitive impairments that may stabilize or improve over time (Alzheimer's Society, 2023).
HIV-associated dementia
In those with HIV, the virus can cause dementia by damaging brain cells, leading to symptoms like memory loss and confusion, impacting overall brain function (Alzheimer's Society, n.d).
Chronic traumatic encephalopathy (CTE)
CTE is linked to repeated head traumas, commonly seen in contact sports athletes (NHS, 2019). It manifests as cognitive decline, mood disturbances, and behavioral changes over time.
Posterior cortical atrophy (PCA)
PCA affects the brain's back part, leading to trouble with visual processing and spatial reasoning, making it difficult for patients to recognize faces or navigate spaces (Alzheimer's Association, 2015).
Mixed dementia
Mixed dementia occurs when symptoms of more than one type of dementia (Custodia et al., 2017), such as Alzheimer's and vascular dementia, appear simultaneously, complicating diagnosis and management.
Ways to assess dementia system disorder
Assessing dementia system disorder requires a multifaceted approach to diagnose and understand the extent of cognitive impairment accurately. This process typically includes cognitive testing, imaging studies, and laboratory tests, each providing crucial insights into the patient's condition and helping to differentiate dementia from other neurocognitive disorders.
Cognitive testing
Cognitive testing evaluates functions such as memory, language skills, and problem-solving abilities. Tests like the Mini-Mental State Examination(MMSE) (Kurlowicz & Wallace, 1999) and the Clock Drawing Test (Rogers & Panegyres, 2007) are quick yet effective tools for initial screening. Neuropsychological testing delves deeper, assessing specific cognitive domains and identifying early symptoms of dementia. These assessments are vital for diagnosing conditions such as Alzheimer's disease and other major neurocognitive disorders.
Imaging studies
Imaging studies like MRI and CT scans are instrumental in visualizing brain structure and identifying anomalies that may contribute to cognitive decline, such as strokes or tumors. PET scans go further by detecting amyloid plaques, a hallmark of Alzheimer's disease. These studies are essential for ruling out other causes of dementia symptoms and confirming diagnoses like normal pressure hydrocephalus or Parkinson's disease dementia.
Laboratory tests
Laboratory tests help exclude other conditions that mimic dementia symptoms, such as vitamin deficiencies or thyroid disorders. Standard tests include checking Vitamin B12 levels and thyroid function tests, which can impact cognitive function if not within normal ranges. Cerebrospinal fluid analysis is also used to detect specific biomarkers for Alzheimer's disease, aiding in early diagnosis and management.
References
Alzheimer's Association. (2015). Posterior cortical atrophy. Alzheimer’s Disease and Dementia. https://www.alz.org/alzheimers-dementia/what-is-dementia/types-of-dementia/posterior-cortical-atrophy
Alzheimer's Society. (2023). Alcohol-related “dementia”. Alzheimer’s Society. https://www.alzheimers.org.uk/about-dementia/types-dementia/alcohol-related-dementia
Alzheimer's Society. (n.d.). HIV-associated neurocognitive disorder (HAND). Alzheimer’s Society. https://www.alzheimers.org.uk/about-dementia/types-dementia/hiv-cognitive-impairment
Custodio, N., Montesinos, R., Lira, D., Herrera-Pérez, E., Bardales, Y., & Valeriano-Lorenzo, L. (2017). Mixed dementia: A review of the evidence. Dementia & Neuropsychologia, 11(4), 364–370. https://doi.org/10.1590/1980-57642016dn11-040003
Emmady, P. D., Schoo, C., & Tadi, P. (2022). Major neurocognitive disorder (dementia). StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK557444/
Kumar, A., Tsao, J. W., Sidhu, J., & Goyal, A. (2024). Alzheimer disease. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK499922/
Kurlowicz, L., & Wallace, M. (1999). The Mini-Mental State Examination (MMSE). Journal of Gerontological Nursing, 25(5), 8–9. https://doi.org/10.3928/0098-9134-19990501-08
Loi, S. M., Cations, M., & Velakoulis, D. (2023). Young‐onset dementia diagnosis, management and care: A narrative review. The Medical Journal of Australia, 218(4), 182–189. https://doi.org/10.5694/mja2.51849
National Institute on Aging. (2021). What are frontotemporal disorders? Causes, symptoms, and treatment. https://www.nia.nih.gov/health/frontotemporal-disorders/what-are-frontotemporal-disorders-causes-symptoms-and-treatment
National Institute on Aging. (2021). What is Lewy body dementia? Causes, symptoms, and treatments. https://www.nia.nih.gov/health/lewy-body-dementia/what-lewy-body-dementia-causes-symptoms-and-treatments
NHS. (2019, April 17). Chronic traumatic encephalopathy. NHS. https://www.nhs.uk/conditions/chronic-traumatic-encephalopathy/
Rogers, J. M., & Panegyres, P. K. (2007). Cognitive impairment in multiple sclerosis: Evidence-based analysis and recommendations. Journal of Clinical Neuroscience, 14(10), 919–927. https://doi.org/10.1016/j.jocn.2007.02.006
Vijayan, M., & Reddy, P. H. (2016). Stroke, vascular dementia, and Alzheimer’s disease: Molecular links. Journal of Alzheimer’s Disease, 54(2), 427–443. https://doi.org/10.3233/jad-160527
World Health Organization (WHO). (2023, March 15). Dementia. https://www.who.int/news-room/fact-sheets/detail/dementia
Commonly asked questions
The life expectancy for someone with Lewy body dementia varies but typically ranges from 5 to 8 years after diagnosis. This timeframe can differ based on the individual's overall health, diagnosis age, and symptoms' severity.
Yes, dementia is considered a nervous system disorder. It primarily affects the brain and leads to significant impairment in cognitive function. It disrupts the normal functioning of the brain's neurons, impacting memory, thinking, and behavior.
Dementia profoundly impacts health and well-being by impairing cognitive functions such as memory, reasoning, and communication skills. This can complicate daily activities and diminish the quality of life. Additionally, it can lead to emotional distress and physical health decline as the condition progresses.
Dementia is related to the central nervous system and specifically impacts the brain. It leads to brain tissue degradation and brain cells malfunctioning, which are crucial for cognitive function, memory, and behavior.




















-template.jpg)