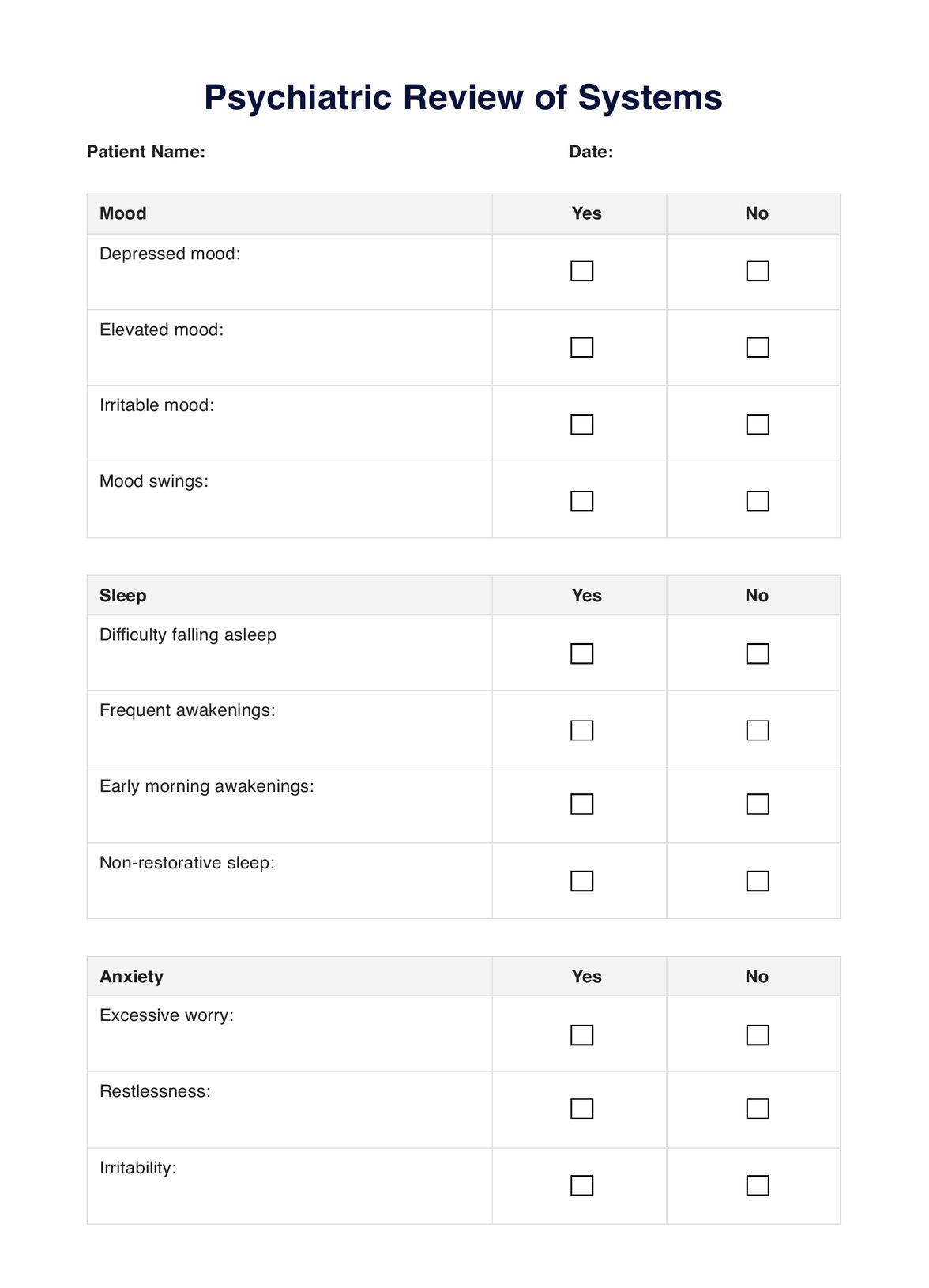
Psychiatric Review Of Systems
Streamline mental health assessments with a Psychiatric Review of Systems template, a tool for professionals to assess and document patients' mental well-being.


What is a psychiatric review of systems?
A psychiatric review of systems (PROS) is a comprehensive evaluation process used to gather essential information about a patient's mental health and overall well-being. It involves a thorough exploration of various aspects of the patient's life and medical history, including their mental status, psychiatric history, medical history, family history, and current symptoms.
The primary goal of a review of systems is to obtain a detailed understanding of the patient's mental health condition, identify potential underlying causes or contributing factors, and ultimately arrive at an accurate diagnosis. This information is crucial for developing an appropriate and personalized treatment plan that addresses the patient's specific needs and circumstances (Goldberg & Novack, 1992).
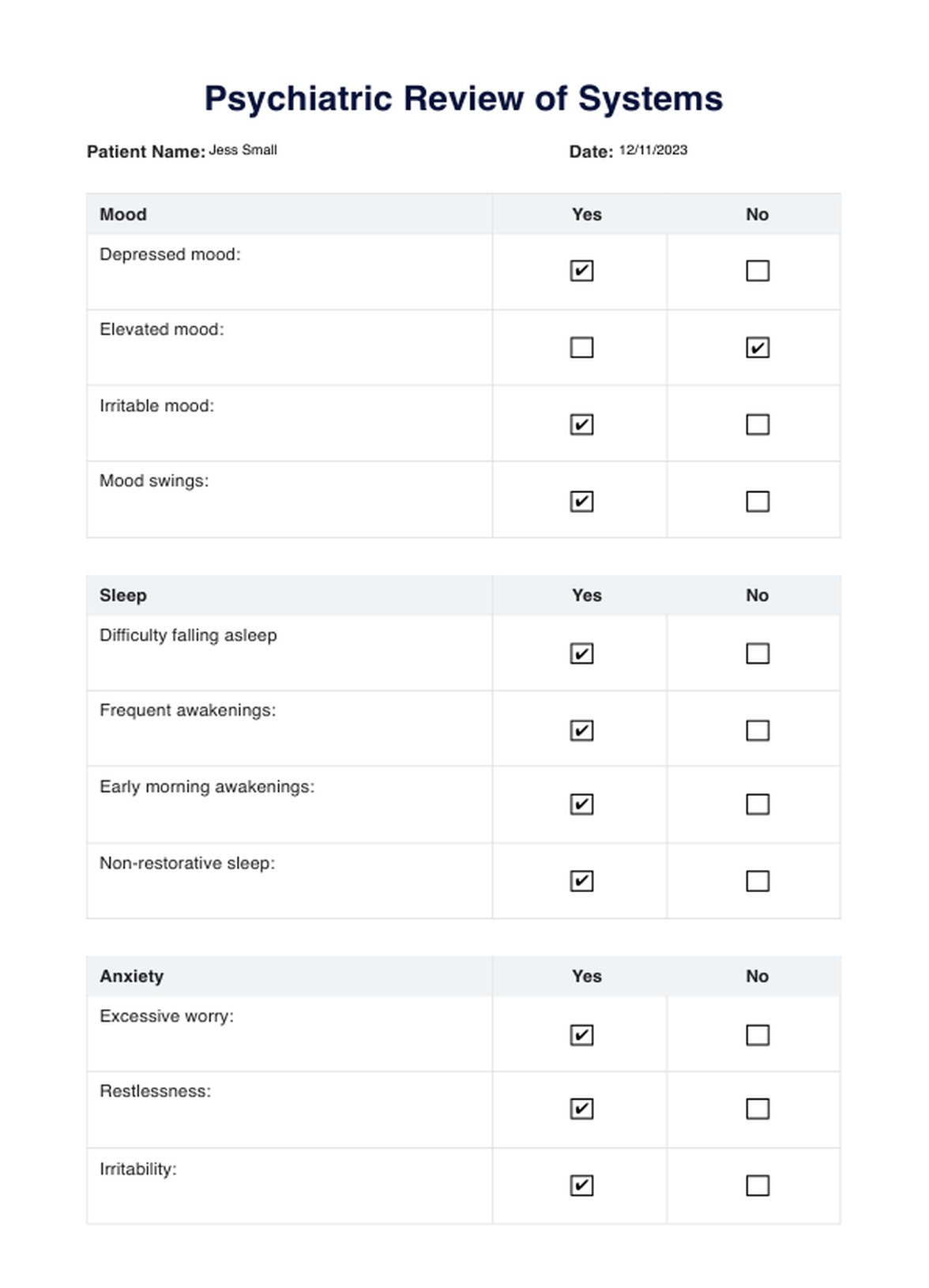
Psychiatric Review Of Systems Template
Psychiatric Review Of Systems Example
What is included in a psychiatric review of systems?
During a psychiatric review of systems, healthcare practitioners typically cover the following key areas:
Mental status examination
This involves assessing the patient's mental state, including their appearance, behavior, speech, mood, thought process, perception, cognition, insight, and judgment.
Past psychiatric history
Healthcare practitioners inquire about any previous or current psychiatric disorders, symptoms, treatments, hospitalizations, and suicide attempts the patient has experienced.
Medical history
A comprehensive medical history is obtained, including any past or current physical symptoms, past medical history, psychiatric medications and treatments, as these can influence or be influenced by the patient's mental health.
Family history
Information about the patient's family history of mental illnesses, substance abuse, or other relevant conditions is gathered, as it can provide insights into potential genetic or environmental factors contributing to the patient's condition.
Psychiatric symptoms
A detailed assessment of the patient's current psychiatric symptoms, such as depressive symptoms, anxiety, psychotic features, dissociative symptoms, obsessive-compulsive symptoms, and personality traits, is conducted. These can then be analyzed using the American Psychiatric Association's (2013) Diagnostic and Statistical Manual of Mental Disorders as a reference.
Substance use and abuse
Healthcare practitioners explore the patient's history of substance use or abuse, as it can significantly impact mental health and complicate diagnosis and treatment.
Psychosocial stressors
Factors such as trauma, stressful life events, or social circumstances are evaluated, as they can contribute to the development or exacerbation of mental health conditions.
How does it work?
When conducting a psychiatric review of systems, healthcare practitioners can follow these five steps to ensure a comprehensive evaluation:
Step 1: Assess mood and sleep
Begin by inquiring about the patient's mood patterns, including depressed mood, elevated mood, irritability, and mood swings. Additionally, explore any sleep disturbances, such as difficulty falling or staying asleep, early morning awakenings, and non-restorative sleep.
Step 2: Evaluate anxiety, psychosis, and obsessive-compulsive symptoms
Next, assess the presence and severity of anxiety symptoms, including excessive worry, restlessness, irritability, concentration difficulties, and physical symptoms like racing heart or sweating. Inquire about any psychotic symptoms, such as hallucinations, delusions, or disorganized thinking. Also, explore the presence of obsessive thoughts and compulsive behaviors.
Step 3: Identify dissociative symptoms and trauma history
Explore any dissociative symptoms the patient may be experiencing, such as detachment, numbness, out-of-body experiences, or memory loss. Additionally, inquire about any exposure to traumatic events and related symptoms like flashbacks or nightmares, which may indicate post-traumatic stress disorder (PTSD).
Step 4: Assess body image disturbances and substance abuse
Evaluate the patient's body image and any preoccupation with appearance, dissatisfaction with body image, or engagement in weight control behaviors like excessive dieting or purging. Also, gather information about substance use, including alcohol, tobacco, and illicit drugs.
Step 5: Identify cognitive symptoms and suicidal ideation
Assess the patient's cognitive functioning, including memory problems, concentration difficulties, and decision-making challenges. Finally, inquire about the presence of suicidal ideation, including thoughts of suicide or any specific plans.
Throughout the review, healthcare practitioners should document any additional relevant notes or observations, and use clinical judgment to aid in the diagnostic process and treatment planning.
When would you use this template?
Psychiatric Review of Systems Template can be used in the following situations:
- Initial psychiatric assessment: When a patient first seeks mental health care, a PROS template is typically used to gather a comprehensive overview of their mental and emotional health. This initial assessment helps clinicians identify potential psychiatric disorders, understand the severity of symptoms, and make informed decisions about the next steps in treatment.
- Differential diagnosis: When a patient presents with a complex set of symptoms or overlapping symptoms from multiple disorders, a PROS template can aid in differential diagnosis of a mental illness. The systematic evaluation of various psychiatric domains helps clinicians narrow down the possible diagnoses and make a more accurate diagnosis.
- Pre-operative assessment: Before undergoing surgery or other medical procedures, patients may undergo a psychiatric evaluation to assess their mental health and determine their readiness for the procedure. A PROS template can help identify any potential mental health concerns that may require additional attention or interventions.
Interpreting the results
Key aspects of interpreting the results from a psychiatric ROS include:
- Identification of potential psychiatric disorders: The PROS template systematically evaluates various psychiatric domains, such as mood, anxiety, psychosis, and substance abuse. By identifying symptoms and patterns, clinicians can form hypotheses about potential psychiatric disorders.
- Severity assessment: The PROS template prompts clinicians to assess the severity of each symptom, providing valuable information about the impact of the patient's mental health condition on their daily functioning and overall well-being.
- Differential diagnosis: The PROS template can aid in differential diagnosis, especially when patients present with complex or overlapping symptoms from multiple disorders, for instance bipolar disorder with other mood disorders. By systematically evaluating various psychiatric domains, clinicians can narrow down the possible diagnoses and make a more accurate diagnosis.
- Treatment planning: The gathered information from the PROS template guides clinicians in making informed decisions about the patient's treatment plan. The identified symptoms, their severity, and any underlying psychiatric disorders inform the selection of appropriate treatment modalities, medications, and interventions.
References
Carlat, D. J. (1998). The psychiatric review of symptoms: a screening tool for family physicians. American Family Physician, 58(7), 1617–1624. https://pubmed.ncbi.nlm.nih.gov/9824959/
Goldberg, R. J., & Novack, D. H. (1992). The psychosocial review of systems. Social Science & Medicine, 35(3), 261–269. https://doi.org/10.1016/0277-9536(92)90022-i
Commonly asked questions
A psychiatric review is a comprehensive assessment of a patient's mental health and psychological well-being. It involves a thorough evaluation of the patient's symptoms, medical history, and psychological functioning to identify potential mental health issues.
A psychiatric review of systems typically includes a detailed inquiry into the patient's mental status, including their mood, thought patterns, and behavior. It also assesses their cognitive function, memory, and emotional regulation.
During a full psych evaluation, a trained mental health professional will conduct a series of tests and interviews to gather information about the patient's mental health history, symptoms, and current functioning. This may include standardized assessments, such as the Mini-Mental State Examination (MMSE), and behavioral observations to identify any signs of mental health disorders or cognitive impairment.



















-template.jpg)