Beck’s Suicide Intent Scale
Assess the suicide risk of your patient by using Beck’s Suicide Intent Scale. Learn more about it through this guide.


What are suicidal ideation and suicide intent?
Before we discuss what is all about, let’s briefly discuss what suicidal ideation and suicide intent are first.
When we speak of suicidal ideation, we are referring to the emergence and presence of persistent thoughts (whether they are simply musings, fantasies, or contemplations) of suicide. These thoughts are birthed by symptoms often tied to depression, such as feelings of emptiness, intense loneliness, despair, and problematic beliefs like “there’s nothing to look forward to in this life” and “my pain will never go away.”
If these thoughts remain as they are, we can consider this as passive suicidal ideation. This means that a person simply thinks about death or suicide and/or wishes not to wake up. They will not act upon it. However, if their thoughts translate to actual plans and a genuine desire to commit self-harming acts, we refer to that as active suicidal ideation. You can also refer to it as suicide intent.
When we speak of suicide intent, we refer to a person’s level of determination or seriousness in carrying out a suicidal act. Since they are likely planning it, you can say they are committing to actualizing their thoughts of self-harm.
If you are handling a patient who has thoughts of self-harm, especially if they’ve attempted self-harm before, you can use the Beck’s Suicide Intent Scale to gauge their risk level.
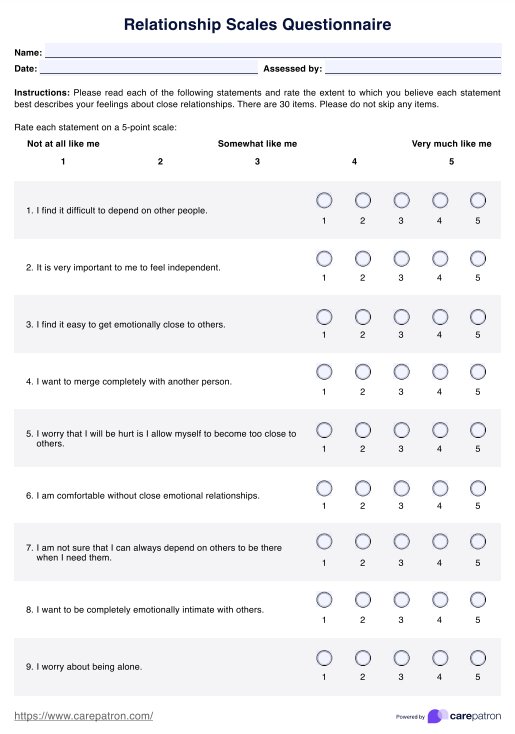
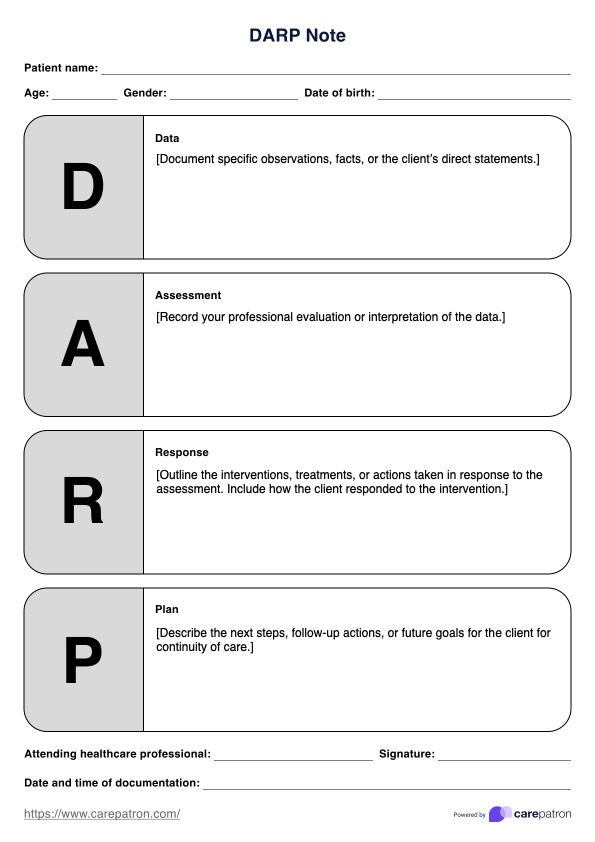
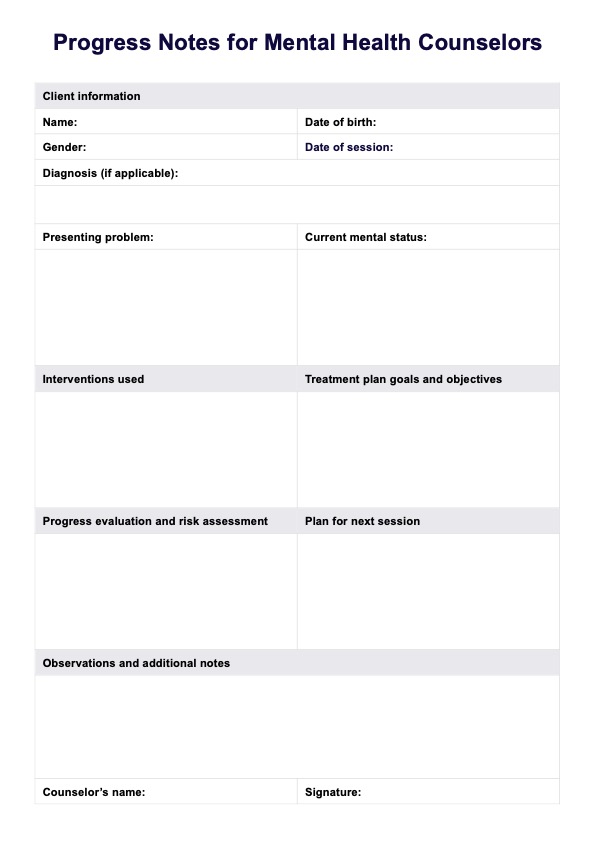
Beck’s Suicide Intent Scale Template
Beck’s Suicide Intent Scale Example
How to use Beck’s Suicide Intent Scale
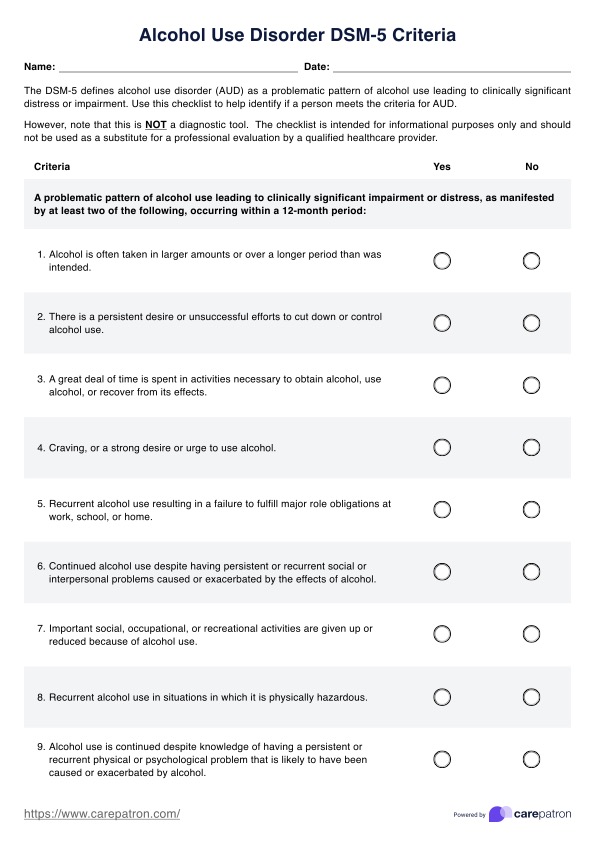
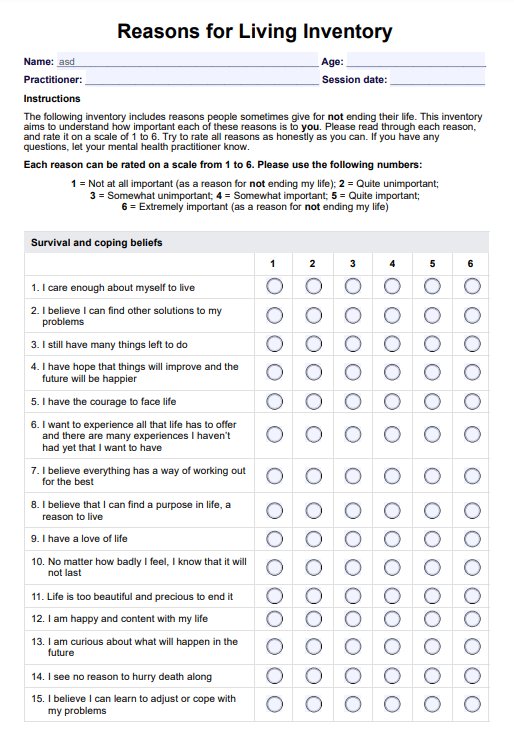
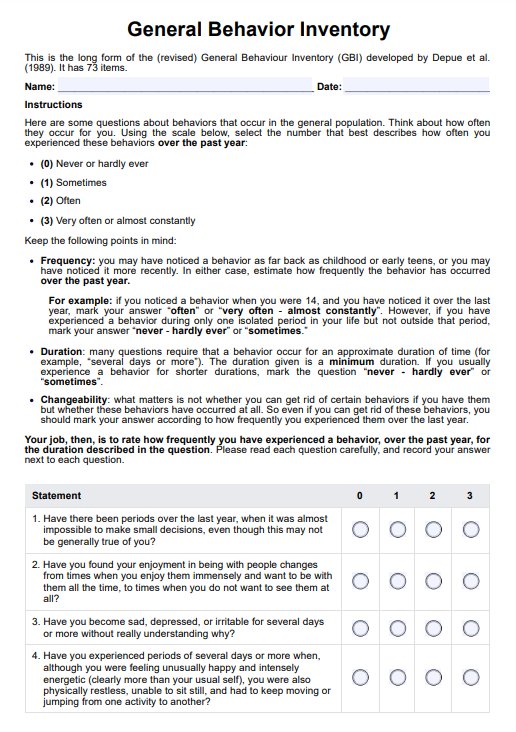
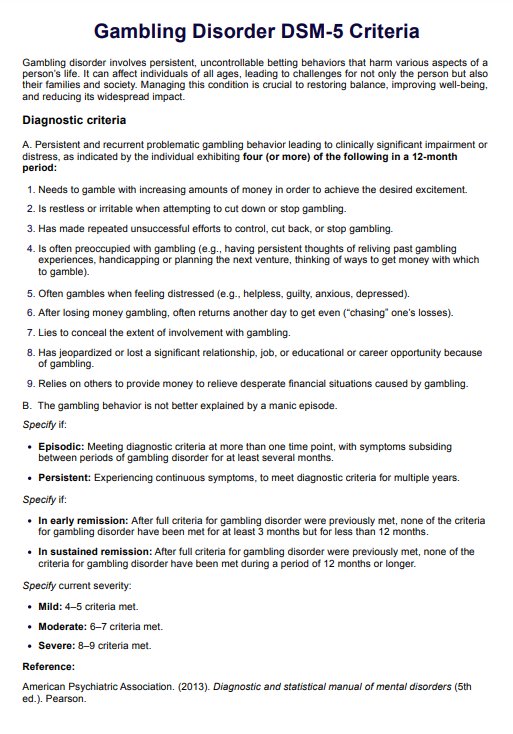
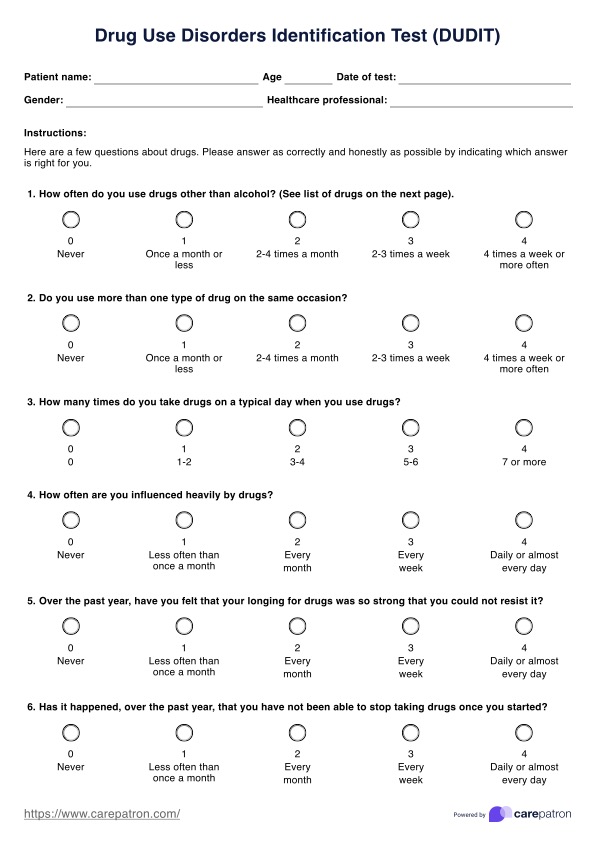
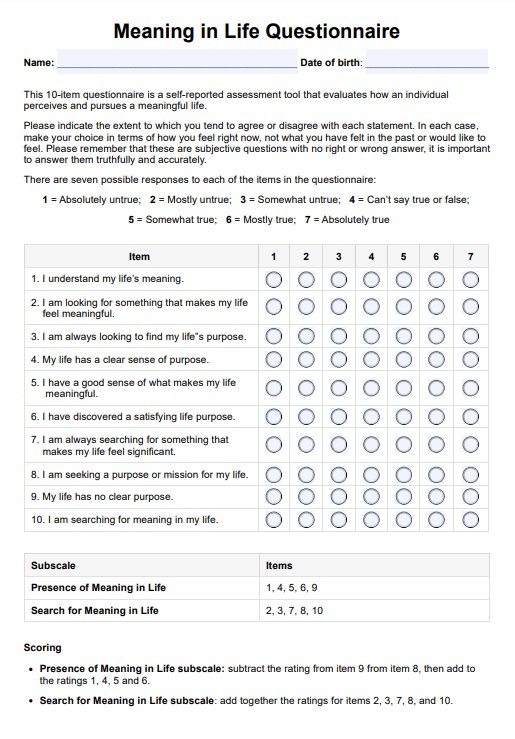
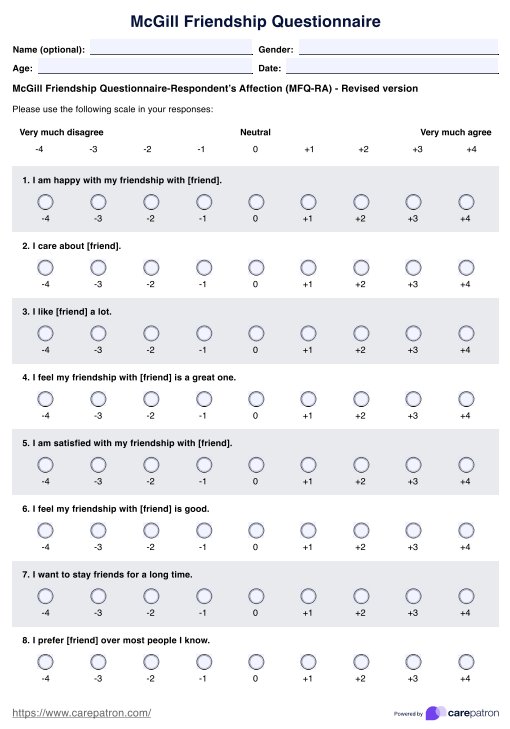
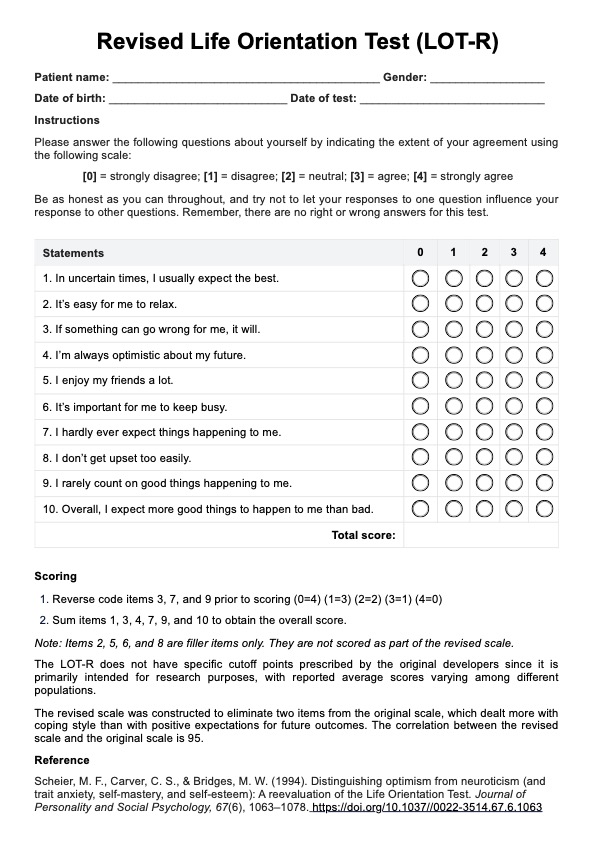
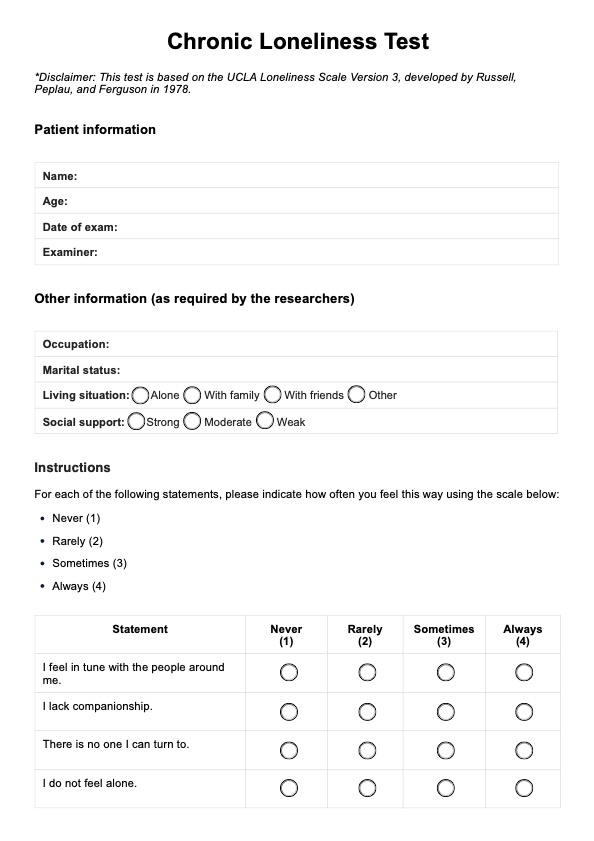
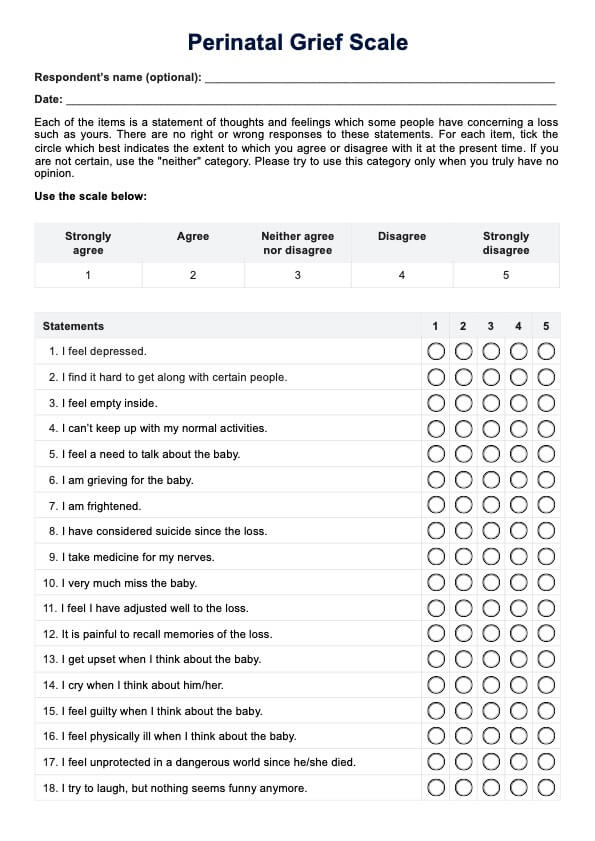
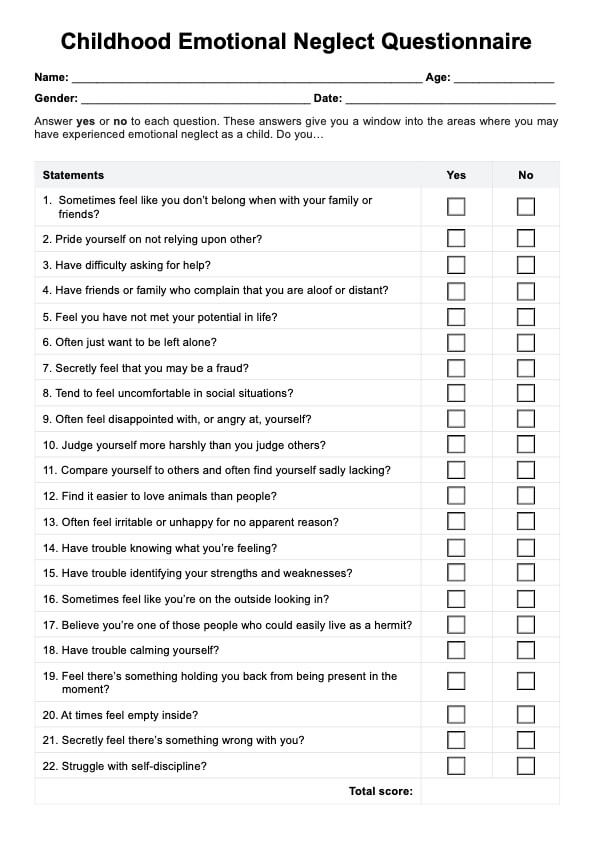
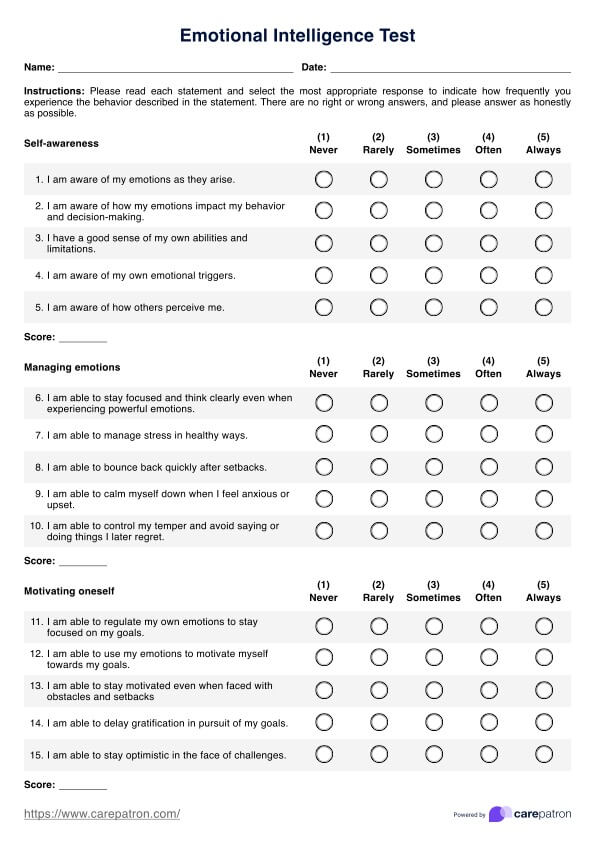
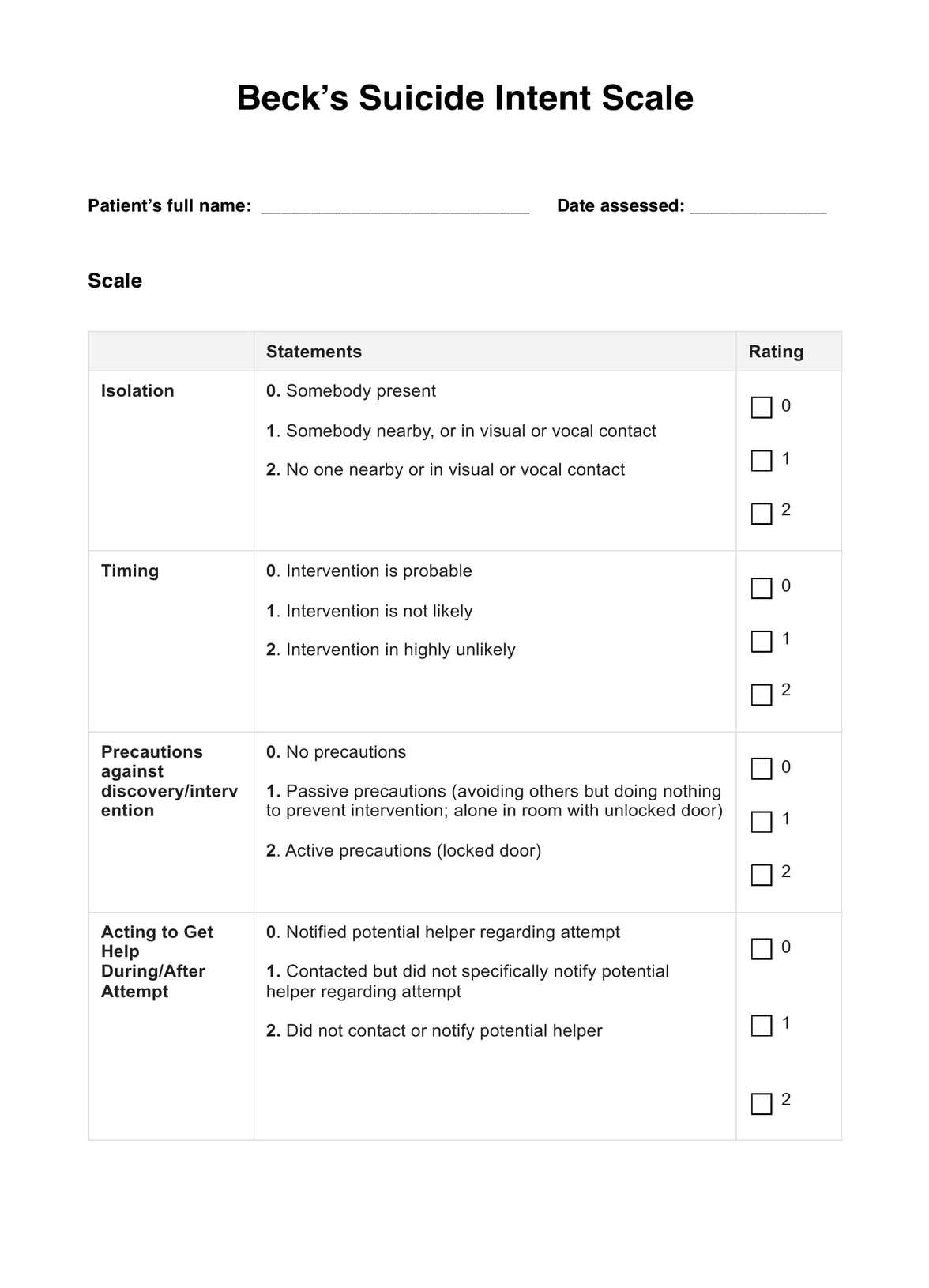
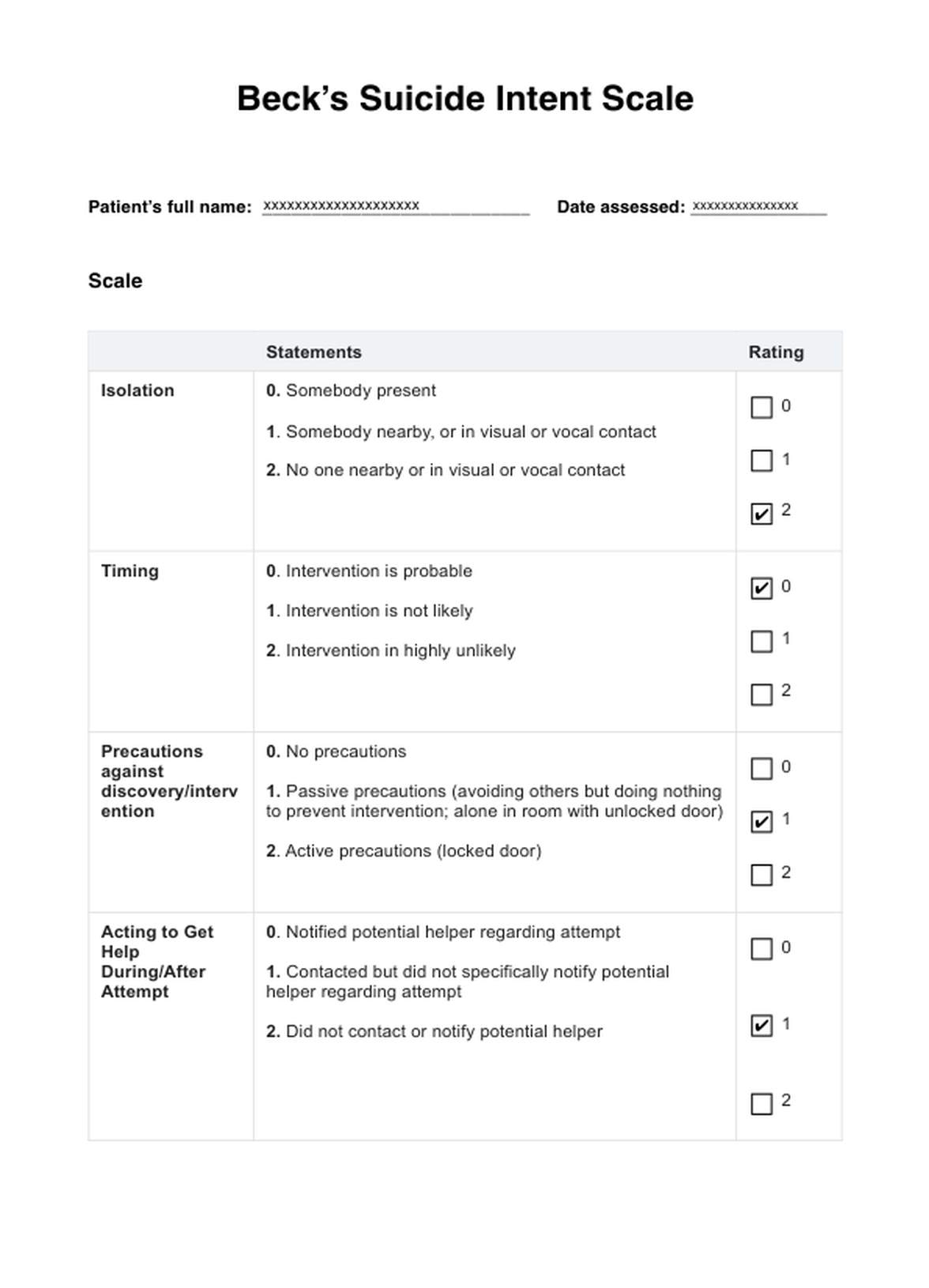
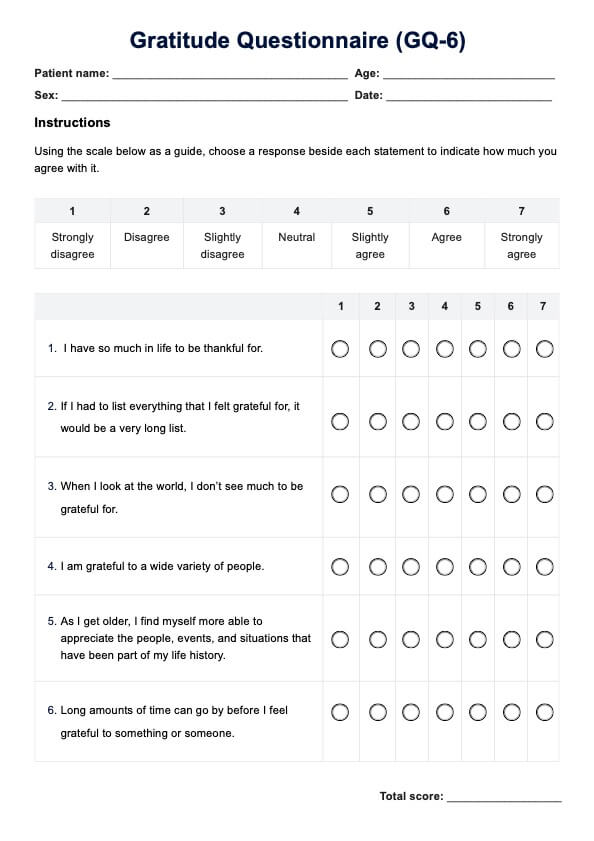
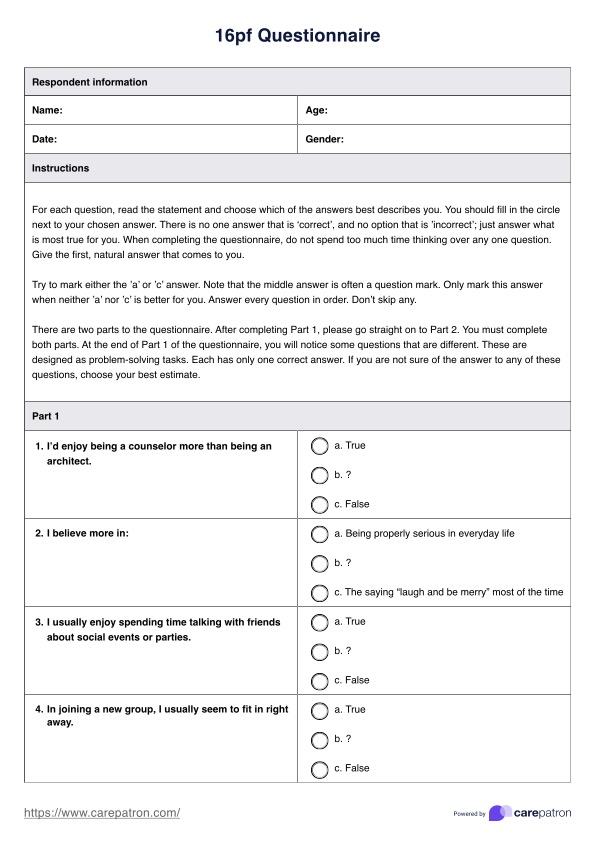
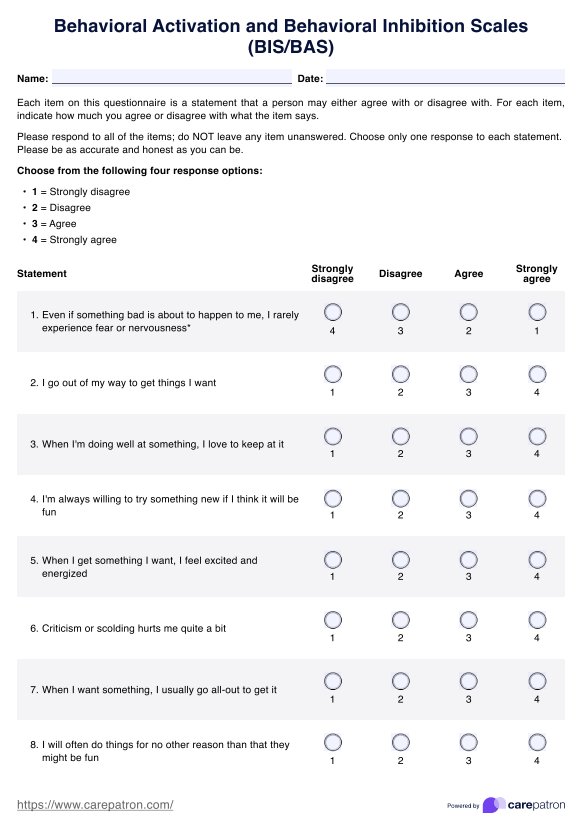
Beck’s Suicide Intent Scale comes in the form of a twenty-item assessment, fifteen of which are scored. These items all revolve around the circumstances of a self-harm/suicide attempt. These items are divided into three parts.
The first part comprises items revolving around objective circumstances related to suicide attempts:
- Isolation
- Timing
- Precautions against discovery/intervention
- Acting to get help during/after an attempt
- Final acts in anticipation of death (e.g., will, gifts, insurance)
- Active preparation for the attempt
- Suicide note
- Overt communication of intent before the attempt
The second part is a self-report section. This means you will either have them answer this part independently or you will ask them questions based on the following items (we recommend you ask them questions instead of handing them a copy of the scale despite the part being a self-report):
- Alleged purpose of the attempt
- Expectations of fatality
- Conception of method’s lethality
- Seriousness of attempt
- Attitude toward living/dying
- Conception of medical rescuability
- Degree of premeditation
The third and last part comprises items that are not scored and are miscellaneous aspects related to suicide attempts:
- Reaction to the attempt
- Visualization of death
- Number of previous attempts
- Relationship between alcohol intake and attempt
- Relationship between drug intake and attempt (e.g., narcotics, hallucinogens; drug is not the method used to commit suicide)
All items have three preset answers. You simply need to select the one that applies the most to the patient per item.
As for scoring, you just need to add up the scores. Each answer set will score a 0, 1, or 2. The answer choices are arranged in that order.
To interpret the scores, you may refer to the following ranges and designations:
- 0 to 10 = Low Risk (Recommended action: send home with advice to see Community Mental Health Team or GP.)
- 11 to 19 = Medium Risk (Recommended action: having them undergo an assessment by Community Mental Health Team or Psychiatrist is advisable. If they refuse treatment, a follow-up with a Community Mental Health Team should be arranged. A psychiatric admission is an option if the patient lives alone, has attempted suicide before, and/or is depressed.)
- 20 to 30 = High Risk (Recommended action: Immediate assessment by Psychiatrist or Community Mental Health Team. Psychiatric admission is also recommended. Involuntary admissions might be required, depending on how serious their intent is.)
When is it best to use Beck’s Suicide Intent Scale?
This scale is most useful when dealing with a patient who has a history of self-harm or suicide attempts and is discussing these issues with you. It's important to explain the purpose of the scale to the patient and obtain their consent before proceeding. Remember, this scale is not a questionnaire; you need to ask the patient questions related to each item and select the response that best fits their answers.
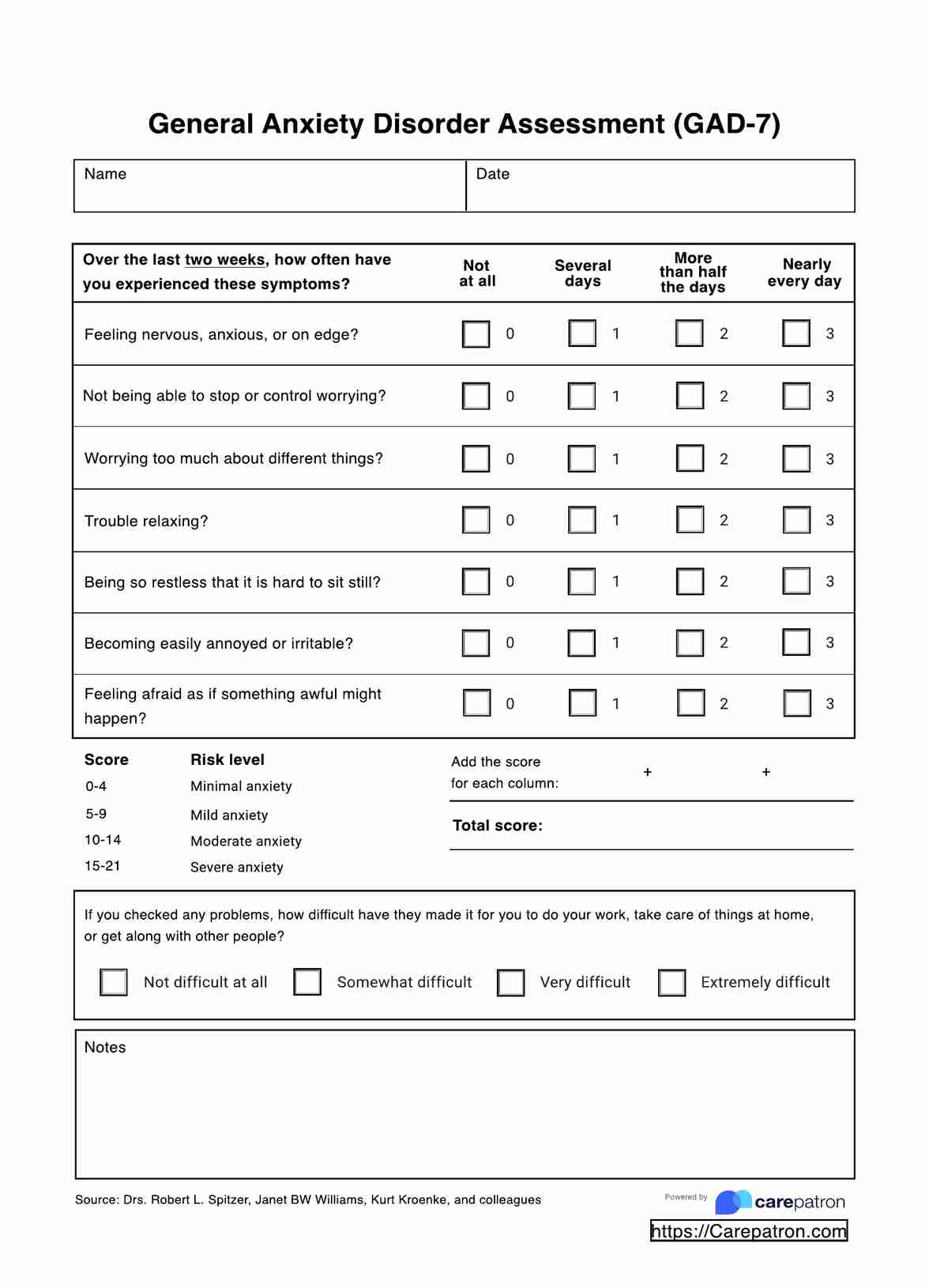
In addition to the Suicide Intent Scale, it’s crucial to use other assessments to identify symptoms of mental health issues that may be linked to suicidal ideation, such as anxiety and depression. Covering as much ground as possible helps you and other professionals provide comprehensive care.
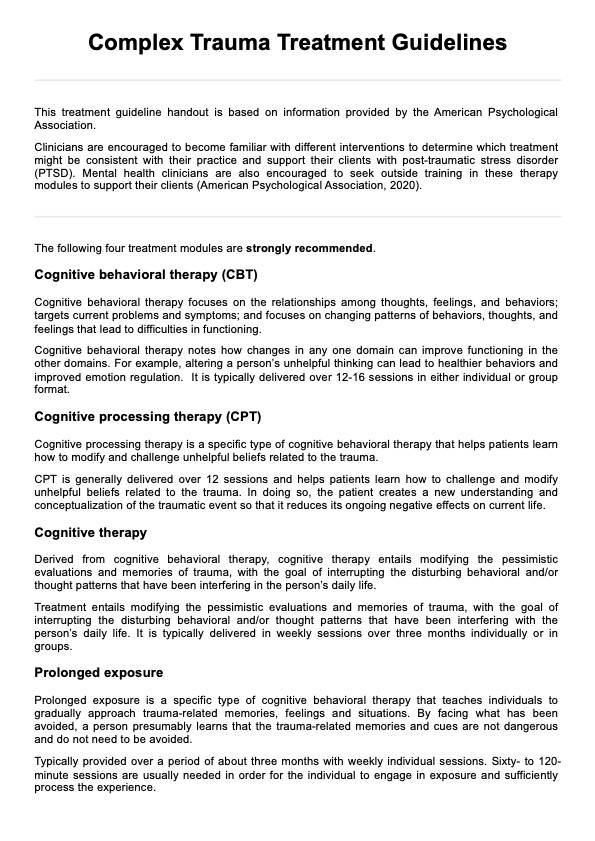
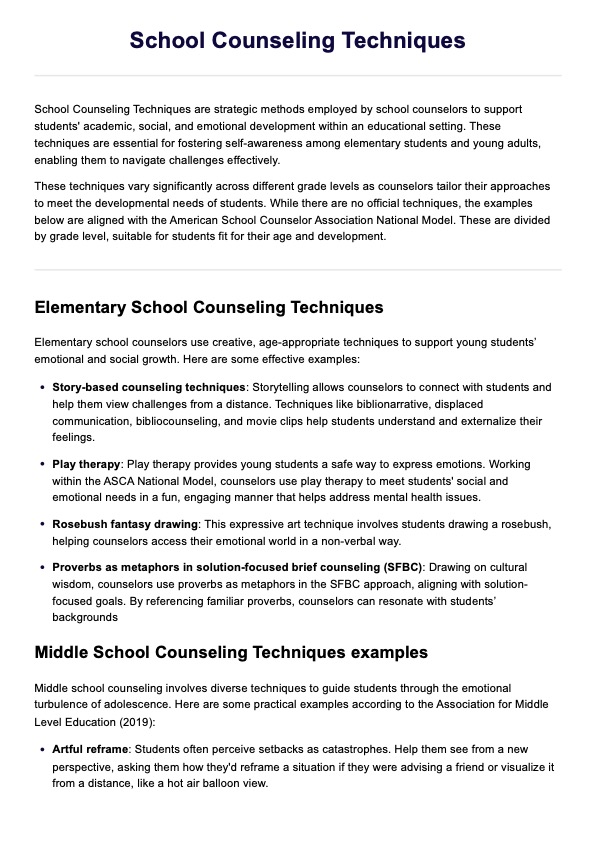
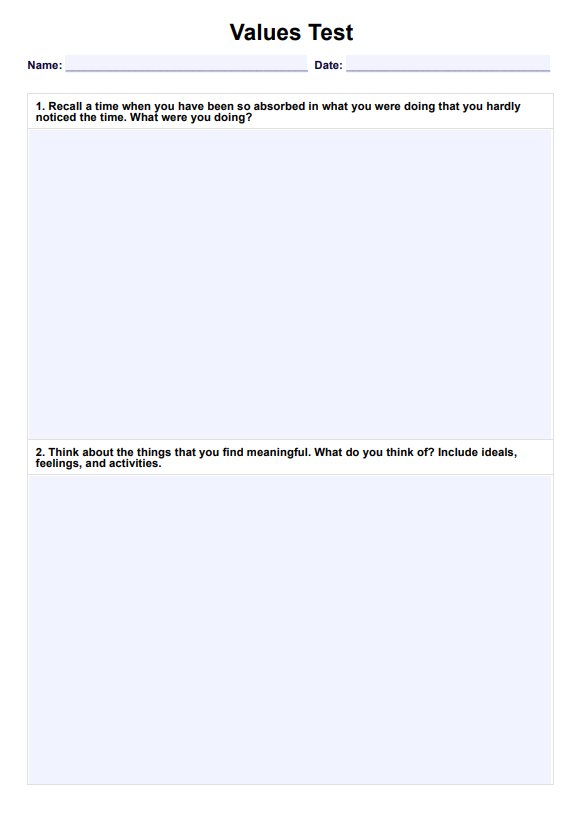
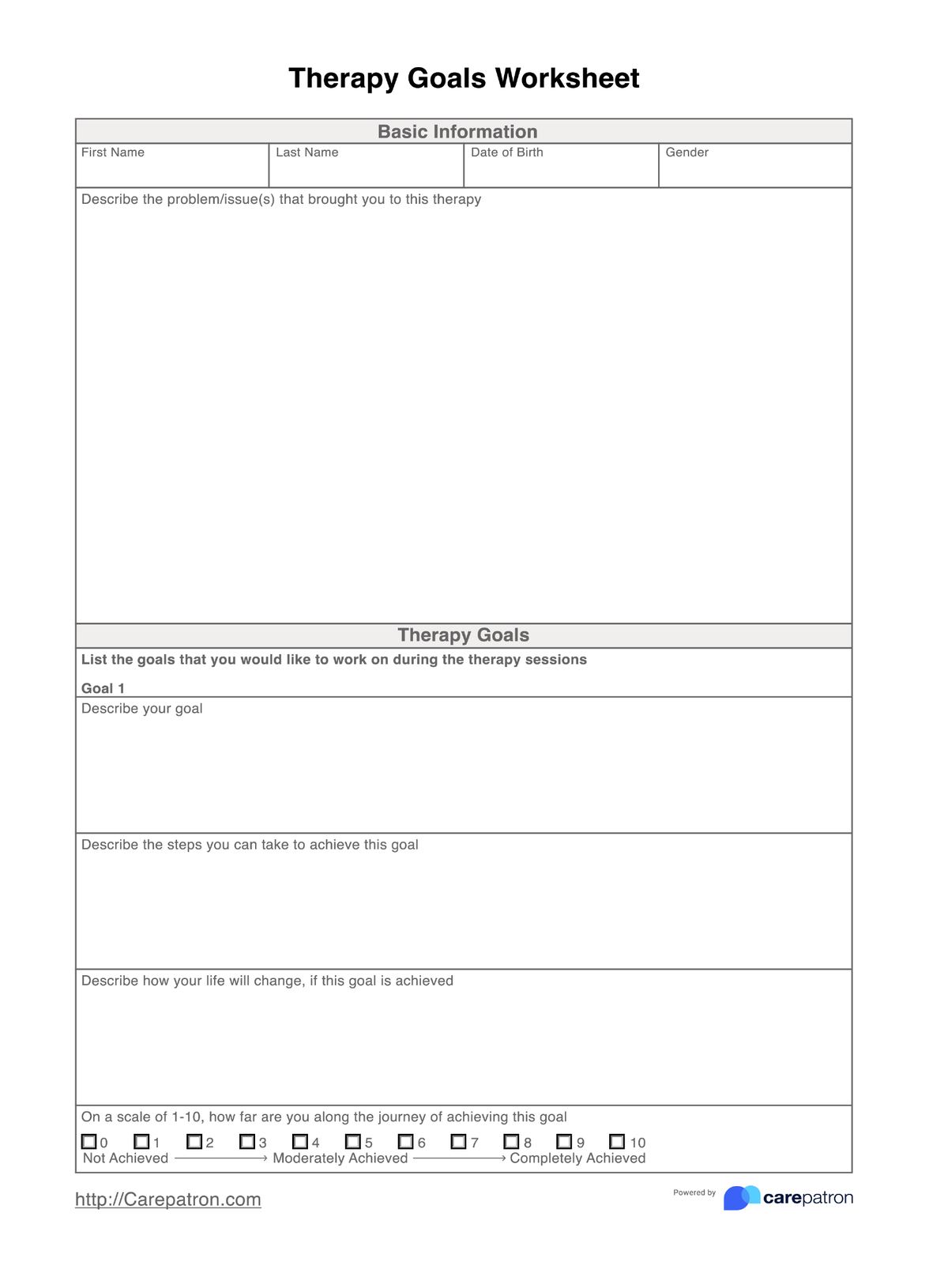
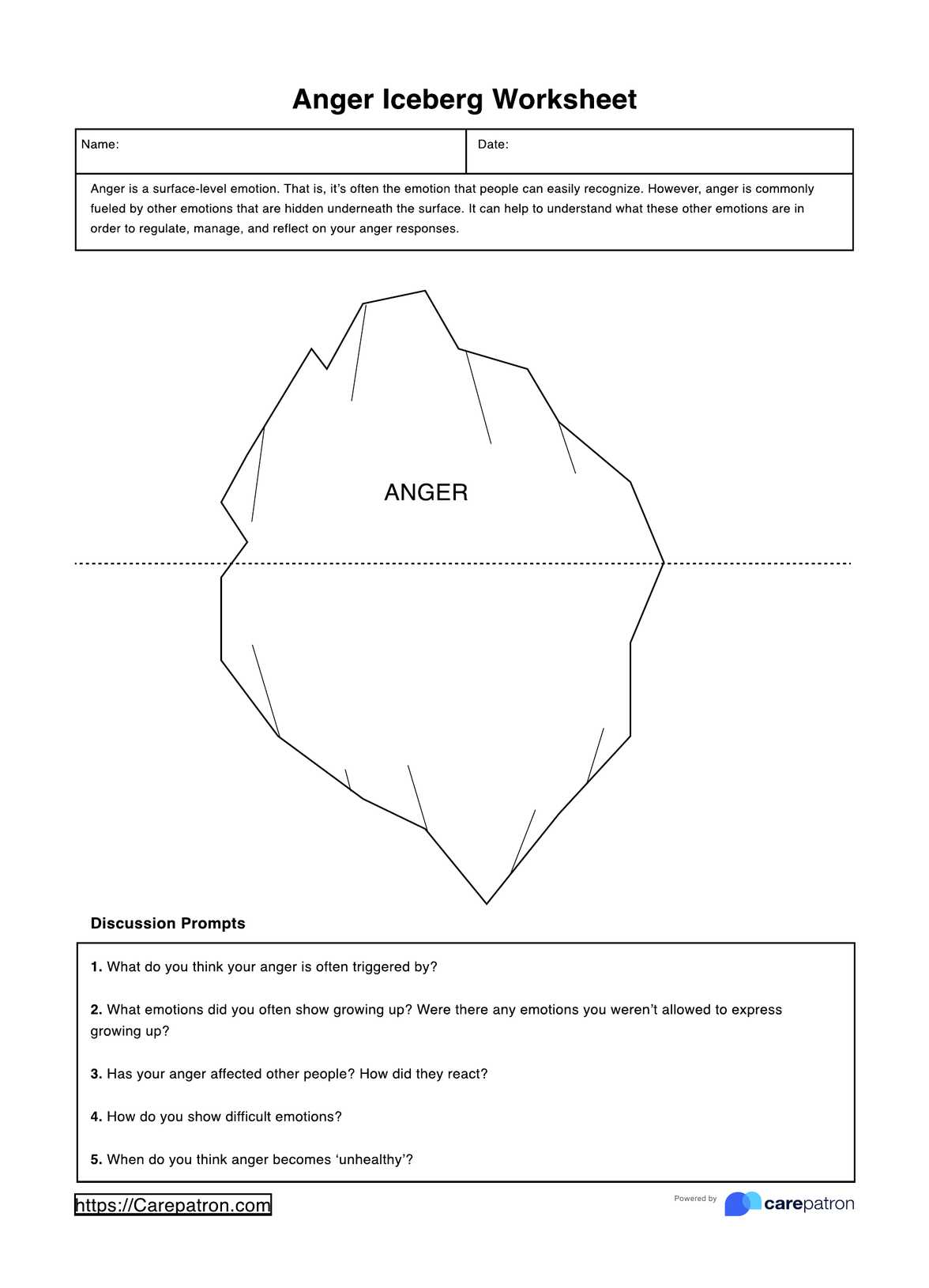
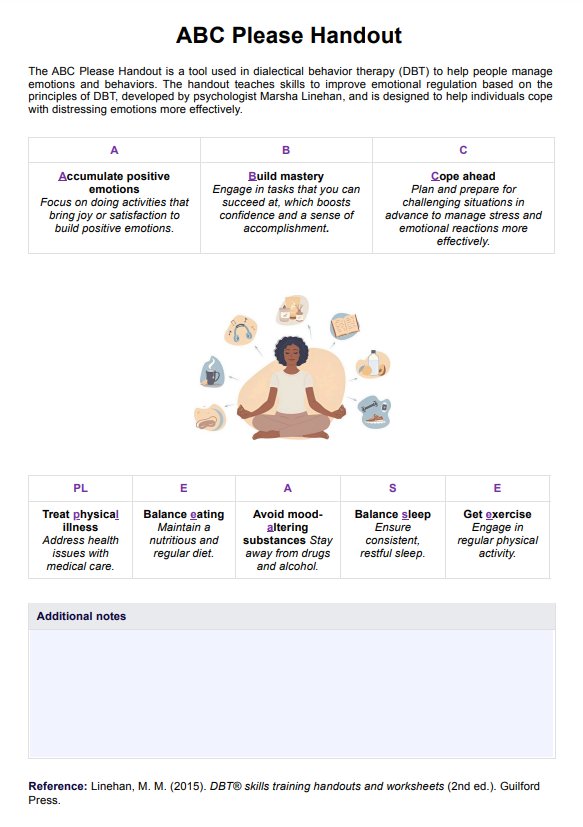
We offer numerous worksheets and tools to help you understand your patients, assist them with their problems, and apply therapeutic techniques. Our extensive resource library includes resources for cognitive behavioral therapy, dialectical behavior therapy, acceptance and commitment therapy, art therapy, and more. Additionally, we provide assessments for mental health symptoms, including the Beck's Depression Inventory and the Beck's Anxiety Inventory.
What are the benefits of using Beck’s Suicide Intent Scale?
It provides a standardized way to assess suicide intent.
The great thing about this scale is that it has a set way of assessing patients. It has established items with preset answers, and score guidelines to help healthcare professionals know the severity of the symptoms they are assessing. They don’t have to worry about dealing with guesswork and wondering, “How should I interpret this score” or “What do I do next,” to mention two questions.
It can help guide professionals with what they need to do next.
Speaking of wondering what to do next, another useful thing about this scale and our template is its recommended actions for each severity level. This should help healthcare professionals consider what to do next, Of course, they don’t necessarily have to follow the designations. They’re free to come up with what to do next based on the risk level their patient has, like administering other assessments to cover more ground.
It can be used as a monitoring tool.
Using Beck’s Suicide Intent Scale doesn’t have to be a one-time thing. Let’s say that your patient undergoes treatment to help manage their suicidal ideation and suicide intent, and they’ve been following the treatment plan you or your team has developed. You can reuse this scale during a routine check-up in case there are any changes to their answers. If their score’s getting lower, even if just a bit compared to their original score, that means they are improving. You can safely assume that your plan might be working. Give it more time and see if there are significant changes over time. If their score remains the same or is getting higher, you’ll have to find ways to manage their ideation and intent better.
Commonly asked questions
It depends on the person being assessed. This assessment tries to gauge heavy and serious topics, so don’t expect to accomplish the whole thing in just a few minutes.
It also depends on the person being assessed. Some patients might find it difficult to answer your questions because suicide ideation and intent is a touchy subject and quite difficult to talk about. So make your patient comfortable enough to answer your questions.
If you somehow managed to find this guide and you’re not a professional, you can definitely download the template and answer it for yourself, but please don’t diagnose yourself with anything. If you have thoughts about suicide, whether you plan on acting it out or not, please see a professional for help.





-template.jpg)