Richmond Agitation Sedation Scale (RASS)
Assess the level of sedation or agitation of your hospitalized patients by using the Richmond Agitation Sedation Scale (RASS).


What is the Richmond Agitation Sedation Scale (RASS)?
Richmond Agitation Sedation Scale, the RASS sedation scale or the RASS scale for short, was developed to help critical care doctors/nurses, emergency doctors/nurses, and respiratory therapists (in the event ventilators are used) assess ICU patients and hospitalized patients with critical illnesses or injuries, but primarily for mechanically ventilated patients.
The scale assesses them in terms of how agitated or sedated they are while undergoing treatment in an emergency room or intensive care unit. Given this, the Richmond Agitation Sedation Scale has since become a cornerstone in critical care medicine, aiding in the effective and controlled sedation of patients that helps manage sedation for critically ill patients.
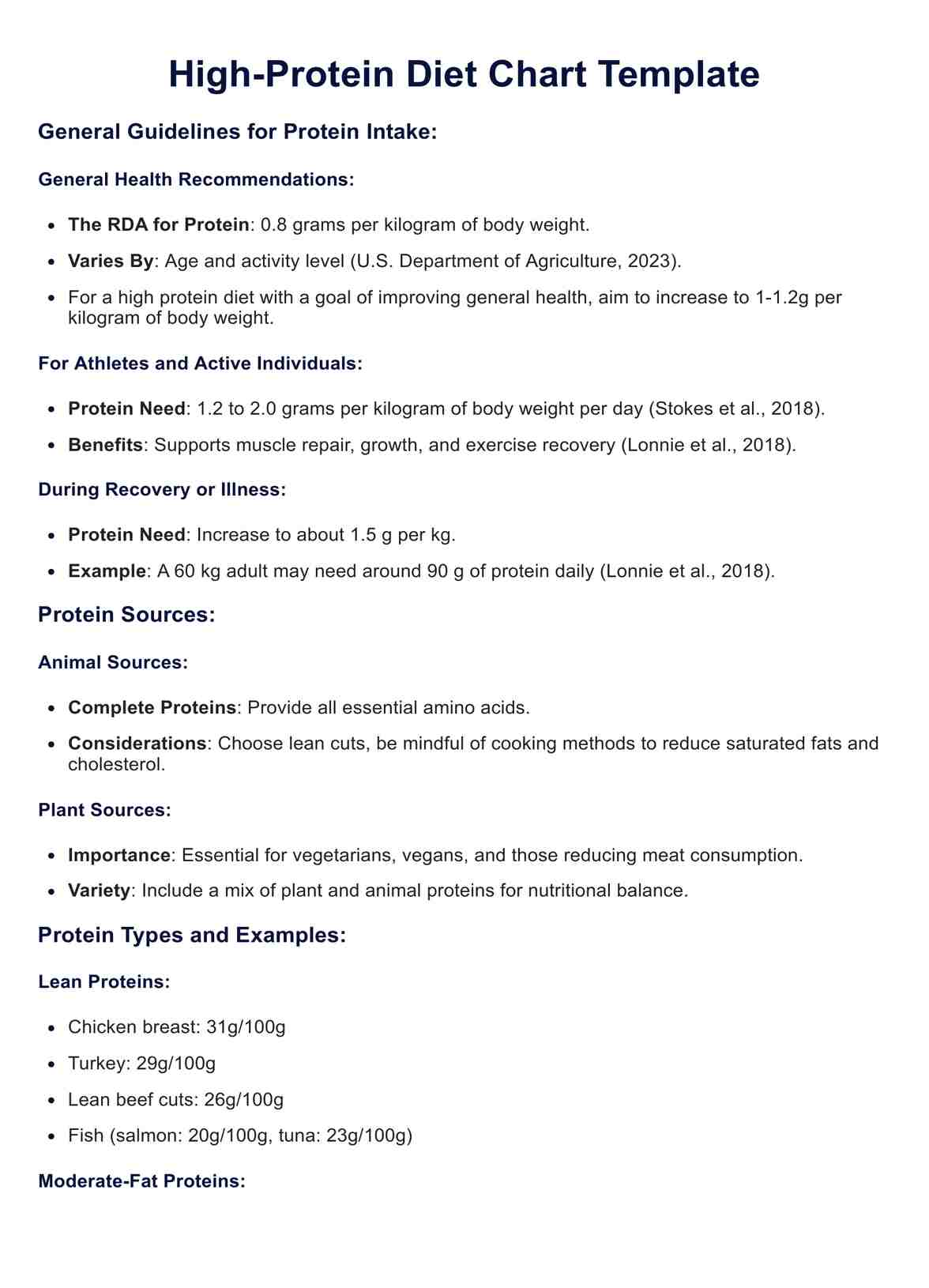
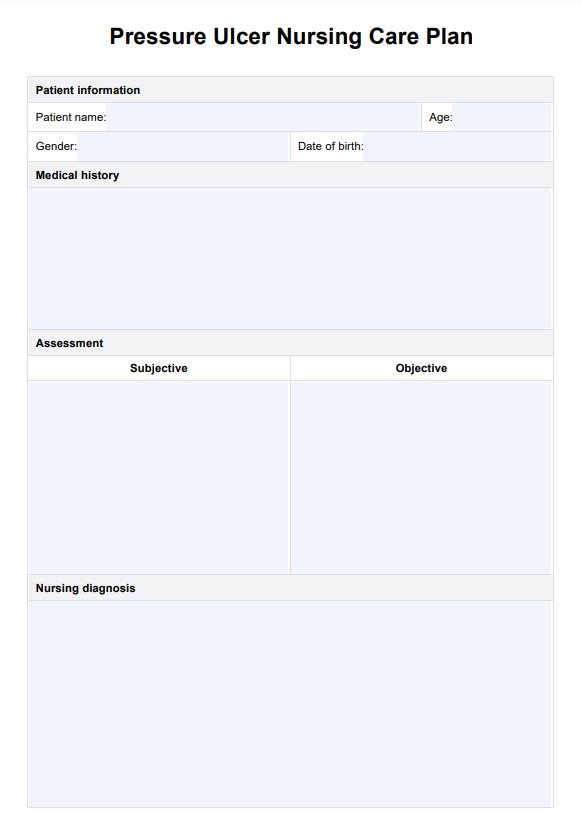
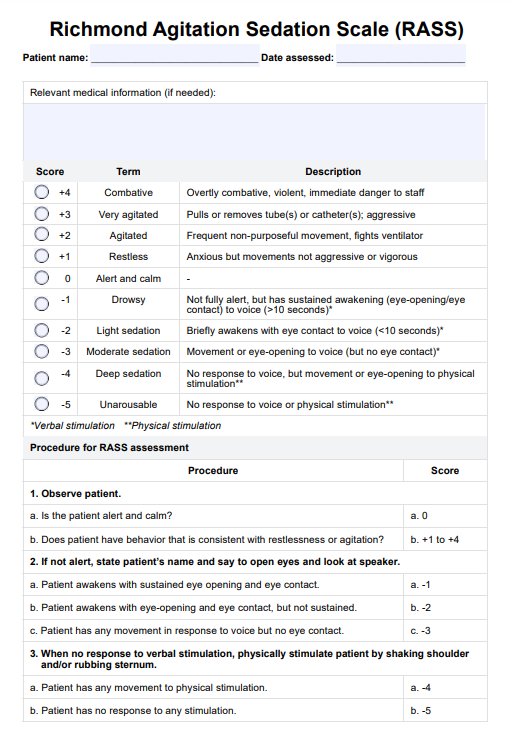
Richmond Agitation Sedation Scale (RASS) Template
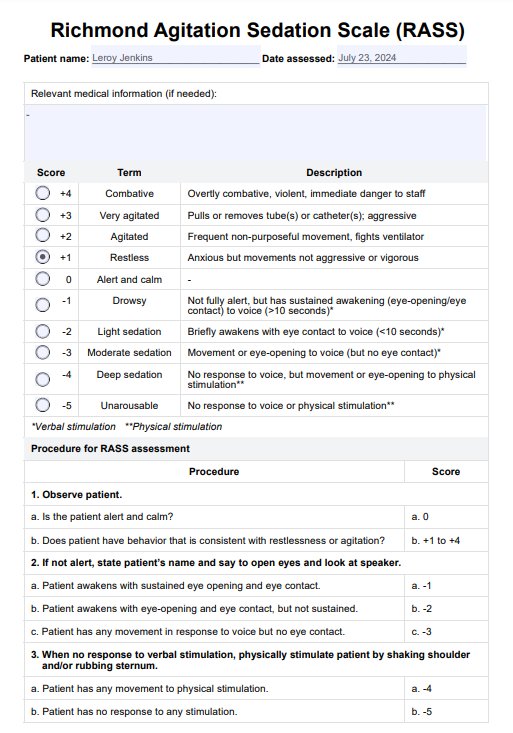
Richmond Agitation Sedation Scale (RASS) Example
How to use the Richmond Agitation Sedation Scale (RASS)?
After obtaining a copy of the Richmond Agitation Sedation Scale PDF template, follow the steps to make the most out of the template:
Step 1: Observe patient
Observe the patient while undergoing treatment in an emergency room or intensive care unit. To properly assign specific scores to the patient, the professional using the RASS Scale needs to observe the patient answer the following questions:
- While they are being treated, is the patient alert? Are they calm? Are they exhibiting any signs of being restless or agitated? Depending on what you notice, this may score anywhere between 0 to +4
- If they are not alert, they are likely in light sedation. If that's the case, try saying your patient's name in a loud speaking voice. Prompt patient and direct patient to open their eyes and look at you. If they are still unresponsive the first time around, you may choose to repeat this once or twice. If they do respond, you may also tell them to continue looking at you as you talk to them. Depending on what you notice, this may score anywhere between -1 and -3.
- If they don't respond to your voice at all, they are likely to be deeply sedated. Physically stimulate patient by shaking their shoulder. If they don't respond to that, rub their sternum. They will either get a score of -4 or -5, signifying a deep sedation protocol, depending on if they respond to being physically nudged or if they don't respond at all.
Step 2: Assign a RASS score
As discussed above, the RASS Scale is scored between -5 and +4. The negative values measure sedation, while the positive values rate agitation. This scale is relatively easy to use because it has a set scoring system with specific designations.
What healthcare professionals need to aim for when using this scale is to get to the point where the patient will score between -2 and +1, which means they are properly sedated. However, this will depend on the sedation protocols for the kind of illness or injury they are treating. It is important to use sedative medications in conjunction with the RASS for effective patient management.
How do you score the Richmond Agitation Sedation Scale (RASS)?
The Richmond Agitation Sedation Scale is easy to score because you must select one score based on your observations. Here are the choices that you can select from:
- +4 means that they are combative, violent, and dangerous to you and the rest of the staff.
- +3 means that they are very agitated and aggressive, and they try to pull or remove tubes or catheters.
- +2 means that they are agitated. They frequently exhibit non-purposeful movement and even try to fight off a ventilator.
- +1 means that they are restless. They are anxious, but they are not aggressive.
- 0 means they are alert and calm.
- -1 means they are drowsy. They aren't fully alert, but they are awake and can open and move their eyes when talked to for 10 or more seconds.
- -2 means they are lightly sedated. They are briefly awake when nudged via speech and can make eye contact for less than 10 seconds.
- -3 means they are moderately sedated or are in moderate sedation. They exhibit movement and can open their eyes (excluding eye contact).
- -4 means they are deeply sedated. They don't respond to voices but move slightly or open their eyes when physically nudged.
- -5 means they are unarousable. They don't respond at all to voice or physical stimulation.
What are the benefits of using the Richmond Agitation Sedation Scale (RASS)?
Here are some of the benefits of utilizing the RASS:
It can help guide professionals with their treatment plans
Responses to treatments will vary from patient to patient. It also depends on the kinds of issues that they are being treated for. Using the Richmond Agitation Sedation Scale will help professionals determine what decisions they have to make while they are applying treatment.
It can help ensure the safety of the patient
The scale can help teams ensure that the patient receives the appropriate level of sedation for their particular treatment. Through careful observations based on the scale's scoring criteria, medical teams will be able to find ways to properly treat the patient and reduce their level of pain. The same goes for sedation itself. You don't want to overly sedate the patient to the point that they experience unwanted complications.
It's an inexpensive tool that is quick to accomplish
The Richmond Agitation Sedation Scale requires no special tools. Rather, it considers tools commonly used in emergency rooms and intensive care units. You don't need anything other than a printed version of this and a pen to tick which score you are giving. Engaging with the sheet shouldn't take you more than ten seconds if you already have all the information, you need based on your observations.
Commonly asked questions
Unlike other scales, which focus on just one thing, this scale assesses both sedation and agitation, giving healthcare professionals a more comprehensive range to consider as they examine and treat patients.
The RASS Scale has clear instructions and is easy to accomplish. It shouldn't take you more than ten seconds to assign a score, especially if you have gotten all the information you need based on your observations.
Besides emergency rooms and intensive care units, you can use this scale in any setting where a patient's agitation and sedation may be of concern, like operating rooms!















-template.jpg)