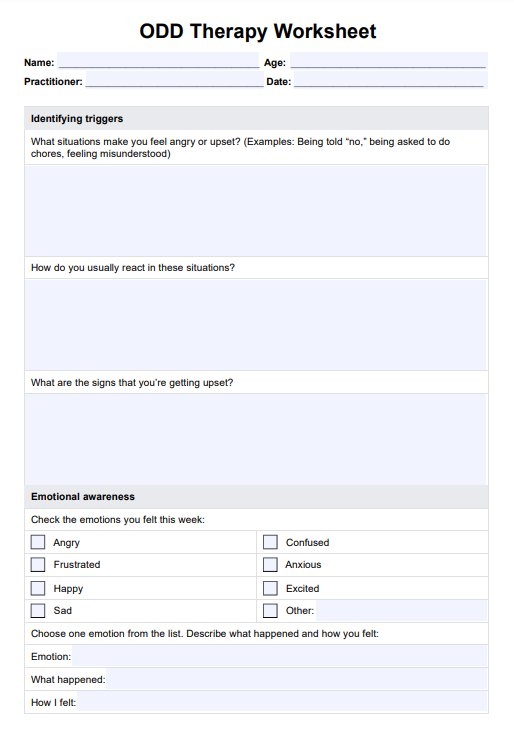
ODD Therapy Worksheets
Download this ODD Therapy Worksheet for emotional regulation and communication skills, promoting positive behavior patterns and personal growth in individuals.


What is an oppositional defiant disorder therapy worksheet?
Oppositional defiant disorder (ODD) can significantly affect a child's behavior, impulse control, and daily interactions, creating challenges for the child and those around them. For mental health professionals, understanding the emotional and behavioral patterns of a child with ODD is essential to providing effective therapeutic approaches.
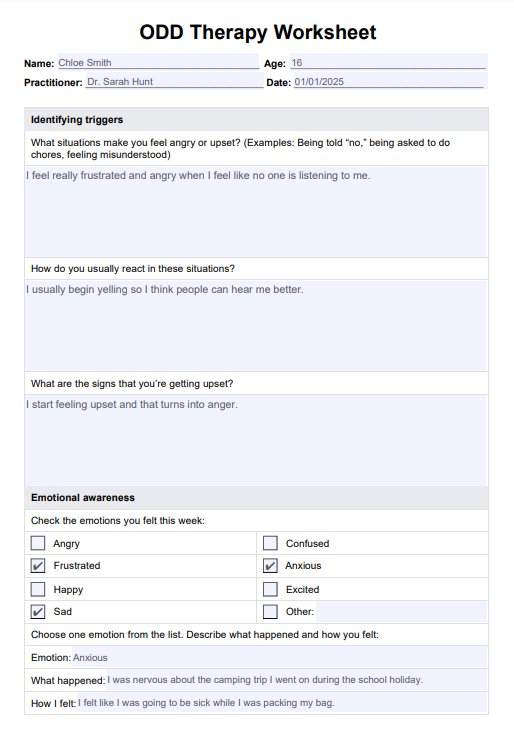
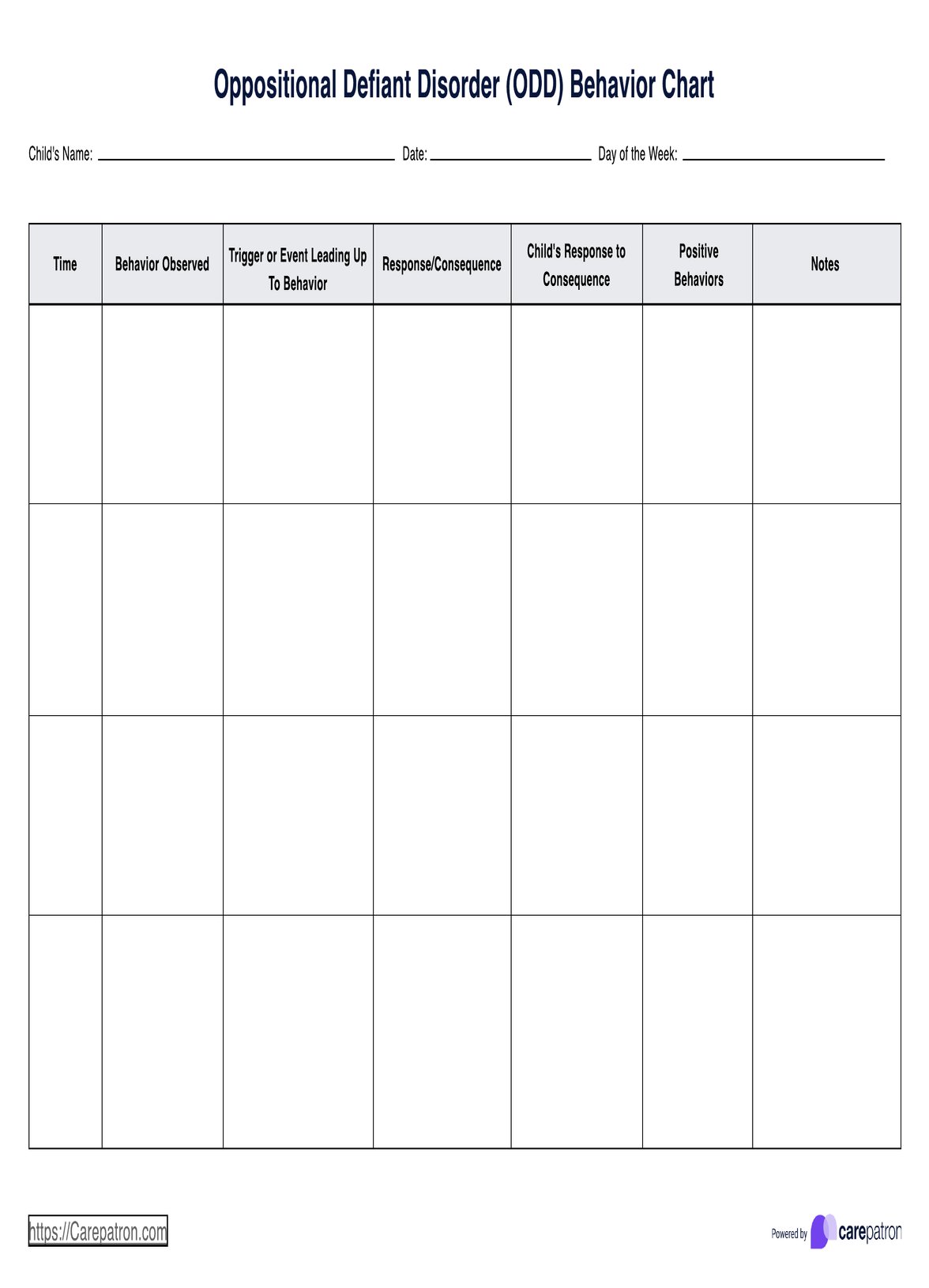
An ODD Therapy Worksheet is a specifically designed tool that helps identify problematic behaviors, explore emotional responses to stress, and develop problem-solving strategies. By fostering self-awareness and practicing constructive responses, these worksheets assist children in building healthier habits, improving their interactions, and making a positive change.
Integrated into therapy sessions, the worksheet serves as a step-by-step framework for tracking progress, celebrating successes, and addressing improvement areas.
ODD Therapy Worksheets Template
ODD Therapy Worksheets Example
How does our ODD Therapy Worksheet work?
We've created a step-by-step guide to demonstrate how this worksheet can be easily implemented into your therapy work.
Step 1: Access the Worksheet
Click the "Use Template" button to open the template via the Carepatron app. This allows you to make any modifications or customizations before sharing it with your client. For a PDF copy: Simply click "Download" to save a print-ready version.
Step 2: Introduce the worksheet
Explain its purpose to your client during the initial session or when introducing the worksheet. For younger clients: Use simple language to describe how the worksheet can help them recognize their feelings and behaviors and how they can make positive changes. For parents or caregivers: Briefly discuss how they can support the child in completing the worksheet and reinforce positive behaviors.
Step 3: Complete the worksheet together
For best results, guide your client through the worksheet during therapy, especially the first time. Walk through each section, asking clarifying questions and helping the client reflect on their experiences. Modify language and expectations based on the client’s age and developmental stage. Younger children may need shorter answers or drawings instead of written responses.
Step 4: Assign as homework
Encourage the client to use the worksheet between sessions to track their progress. At the beginning of each session, review the completed worksheet together. Praise the client for their efforts, focusing on any positive changes or successful use of strategies. Discuss any difficulties the client faced and brainstorm additional coping strategies or solutions.
Symptoms of oppositional defiant disorder
Symptoms of ODD fall into three main categories: angry and irritable mood, argumentative and defiant behavior, and vindictiveness. Children with ODD often lose their temper, are easily annoyed or touchy, and regularly feel angry or resentful (American Psychiatric Association, 2013). They may frequently argue with authority figures, actively refuse to follow rules or requests, deliberately annoy others, and blame others for their mistakes or misbehavior. Vindictive behavior, such as acting spitefully at least twice in the past six months, is another hallmark of the disorder.
The severity and frequency of these behaviors distinguish ODD from typical childhood misbehavior. These behaviors usually occur most days over six months for children under five years old, whereas for children aged five and older, they occur at least once a week during the same time frame. The behaviors must also be more frequent and intense than developmentally normal for the child’s age, gender, and cultural background.
ODD is further categorized by severity. Mild cases involve symptoms in only one setting, such as at home or school. Moderate cases involve symptoms in at least two settings, and severe cases occur in three or more settings. These behaviors often cause significant distress to the child or those around them and can interfere with their ability to function in everyday life.
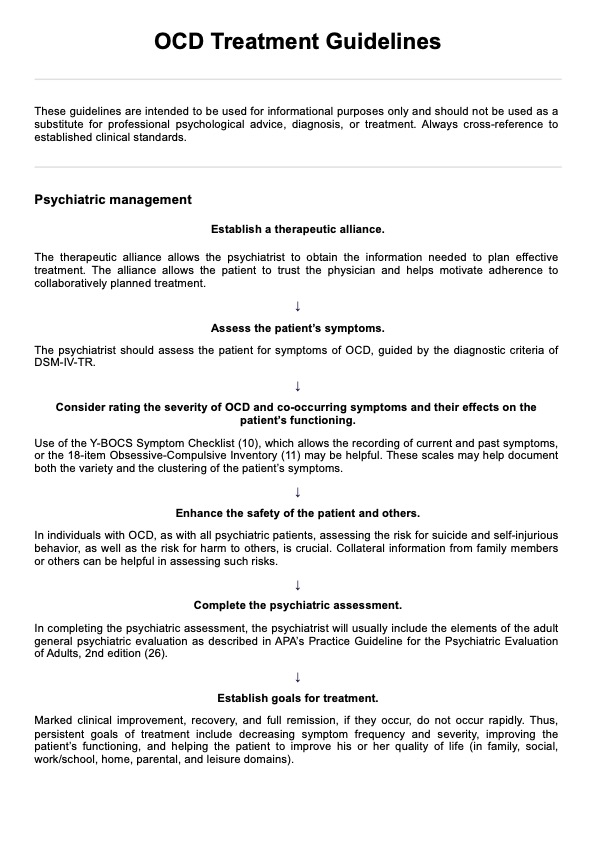
Treatment and management of ODD
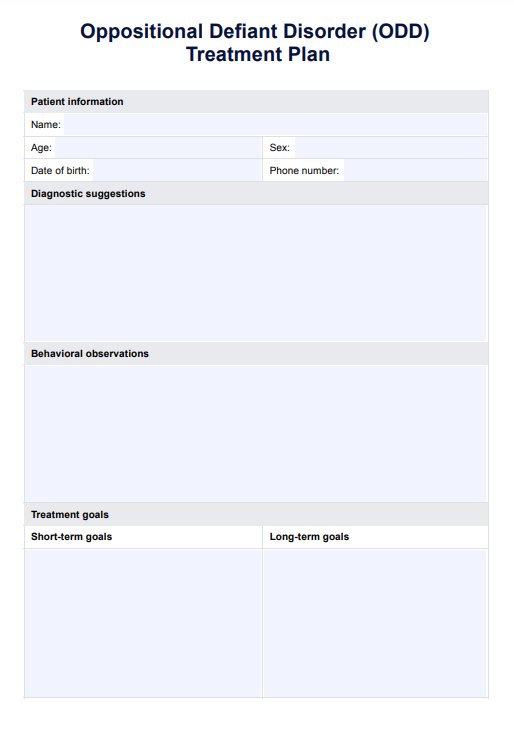
Effective treatment plans often involve a combination of therapies and strategies that target specific aspects of the disorder, aiming to improve behavior, communication, and overall functioning. Below are some key therapeutic approaches used to manage ODD.
Behavioral therapy
One of the most effective treatments for ODD is behavioral therapy. This therapy focuses on reinforcing positive behaviors while addressing and reducing negative behaviors. Cognitive behavioral therapy (CBT) is commonly used to help children identify and manage their emotions, thoughts, and actions. By incorporating strategies to solve problems and practice impulse control, this therapy aims to reshape behavioral patterns. Therapy sessions often involve parents and caregivers to provide support, ensuring they are equipped with practical strategies to manage behaviors at home.
Parent training and support
Parent training is a critical component of managing ODD. Parents can learn strategies to improve communication, set clear and consistent rules, and implement effective discipline techniques. Training helps parents better understand ODD, manage conflicts, and reduce the power struggles that often arise. This training also contributes to professional development for those involved in the child's care, helping parents become active participants in the child’s therapeutic process.
Social skills training
Children with ODD often struggle with interpersonal interactions, which can contribute to social isolation. Social skills training aims to teach children appropriate ways to interact with peers and adults. This may include learning how to handle frustration, communicate effectively, and resolve conflicts. With improved social competence, children with ODD are more likely to experience positive interactions with others, both at school and at home.
Family therapy
Family therapy plays a key role in addressing the broader family dynamics that may contribute to or be affected by the child’s ODD. This approach focuses on improving communication, reducing tension, and fostering a supportive environment for the child. Family therapy provides a space to develop effective strategies for creating a healthier home environment that benefits everyone involved.
Medication
While there is no specific medication for ODD, some medications may be prescribed to address co-occurring conditions, such as anxiety, depression, or attention deficit hyperactivity disorder (ADHD), which are common in children with ODD. Medications like antidepressants or stimulants can help manage these conditions, ultimately improving overall behavior.
Medication should be considered as part of a comprehensive treatment plan. In some cases, adolescent psychiatry may be involved to ensure proper diagnosis and ongoing management of medications. Occupational therapy may also be recommended to address specific sensory processing or behavioral challenges, providing additional support in the treatment plan.
Reference
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596
Commonly asked questions
The most effective therapy for oppositional defiant disorder (ODD) is typically behavioral therapy, particularly cognitive behavioral therapy (CBT). This approach helps children identify and manage their emotions, thoughts, and behaviors, focusing on positive behavior reinforcement and addressing oppositional tendencies.
Disciplining a child with oppositional defiant disorder (ODD) requires clear, consistent, and structured boundaries. Using positive reinforcement for good behavior, setting logical consequences for misbehavior, and avoiding power struggles are essential strategies for managing defiant behavior.
Oppositional defiant disorder (ODD can improve as children grow, often with appropriate interventions and support. While some children may show improvement by adolescence, the severity and persistence of symptoms vary, and early intervention typically leads to better long-term outcomes.























-template.jpg)