Cognitive behavior therapy (CBT), specifically exposure and response prevention (ERP), along with SSRIs, are considered first-line treatments for OCD.
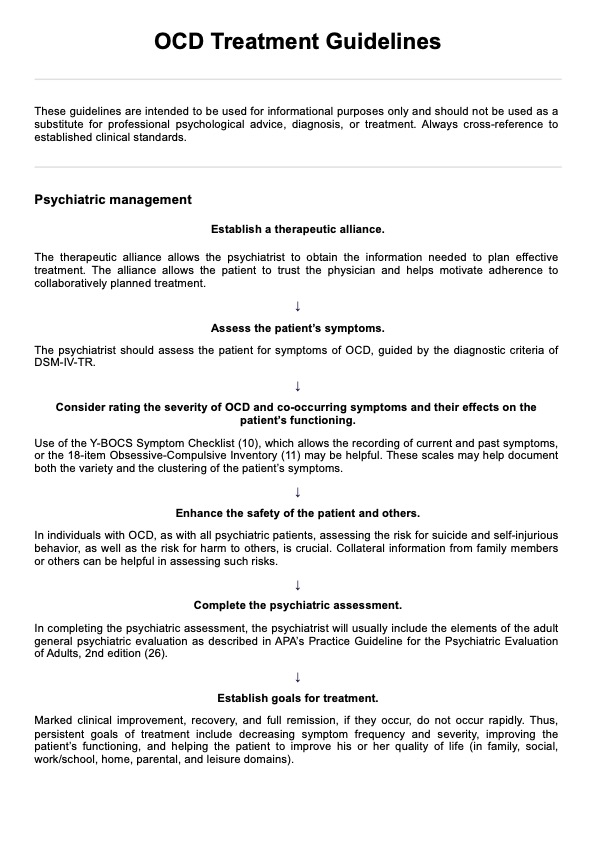
OCD Treatment Guidelines
Utilize quality evidence-based strategies and treatment guidelines for effective navigation of the complexities of OCD to better support your patients.
Use Template
OCD Treatment Guidelines Template
Commonly asked questions
The American Psychiatric Association (APA) recommends CBT and SSRIs as primary treatments for OCD, highlighting the importance of evidence-based practices for psychiatric disorders.
CBT, particularly ERP, is widely regarded as the most effective therapy for OCD, helping individuals confront their fears without engaging in obsessive-compulsive symptoms and behaviors.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











