Occupational Therapy Initial Assessment Template
Optimize patient care with our Occupational Therapy Initial Assessment Template. Streamline assessments, set goals, and track progress efficiently!


What is occupational therapy?
Occupational therapy (OT) is a healthcare profession focused on helping individuals develop, recover, or maintain the skills needed for daily living and working. Occupational therapists work with people of all ages with physical, mental, developmental, or emotional challenges. The primary goal of occupational therapy is to enable people to participate in meaningful activities or occupations despite limitations or disabilities.
Occupational therapists assess a person's abilities, environment, and goals to create customized treatment plans. These plans may include activities to improve motor skills, cognitive abilities, sensory processing, social skills, and emotional regulation. Occupational therapy interventions can involve various activities, such as exercises, adaptive equipment training, environmental modifications, and counseling.
In addition to working directly with individuals, occupational therapists collaborate with other healthcare professionals, educators, employers, and family members to support clients in achieving their goals and maximizing their independence, mobility, and quality of life.
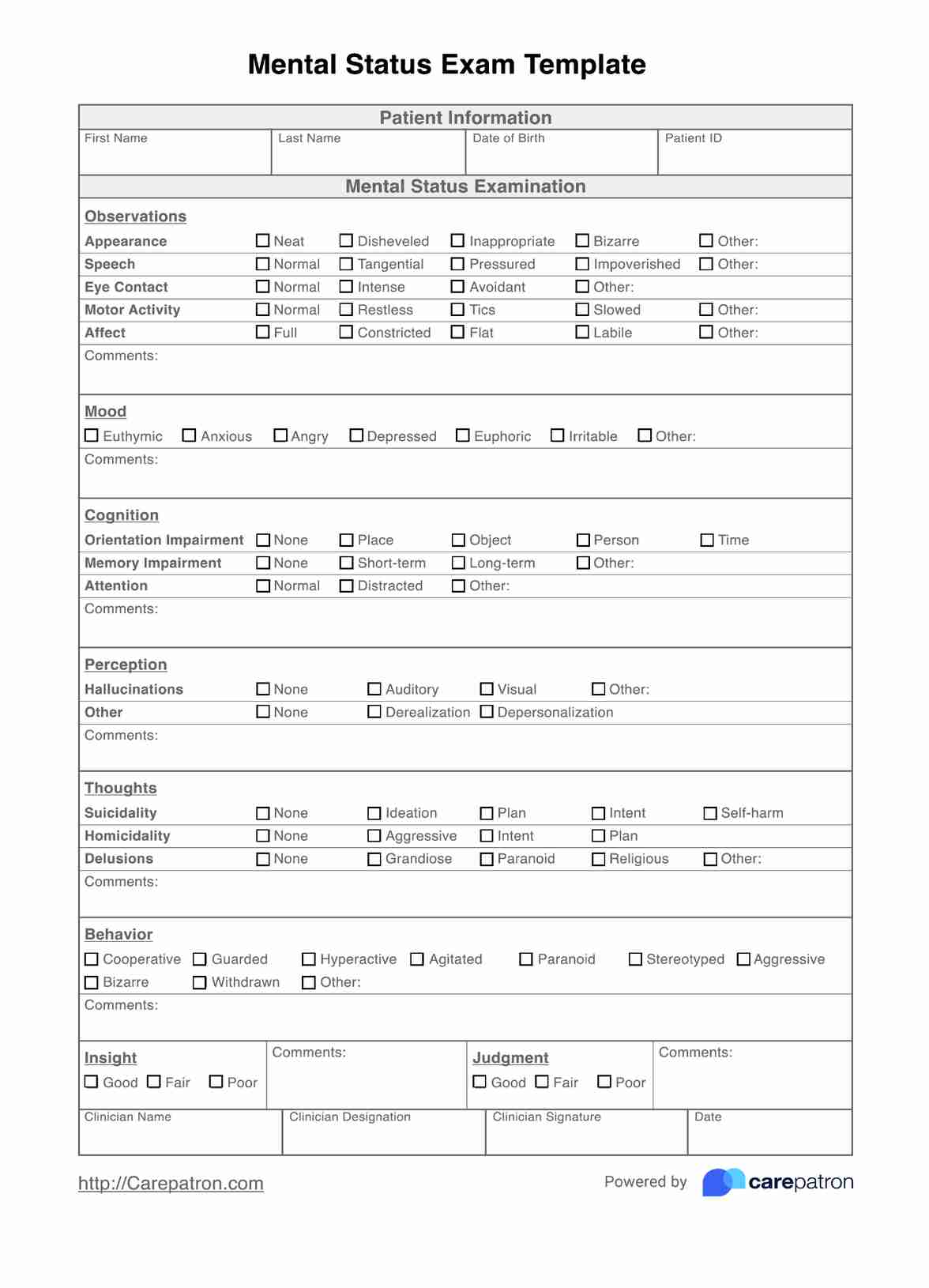
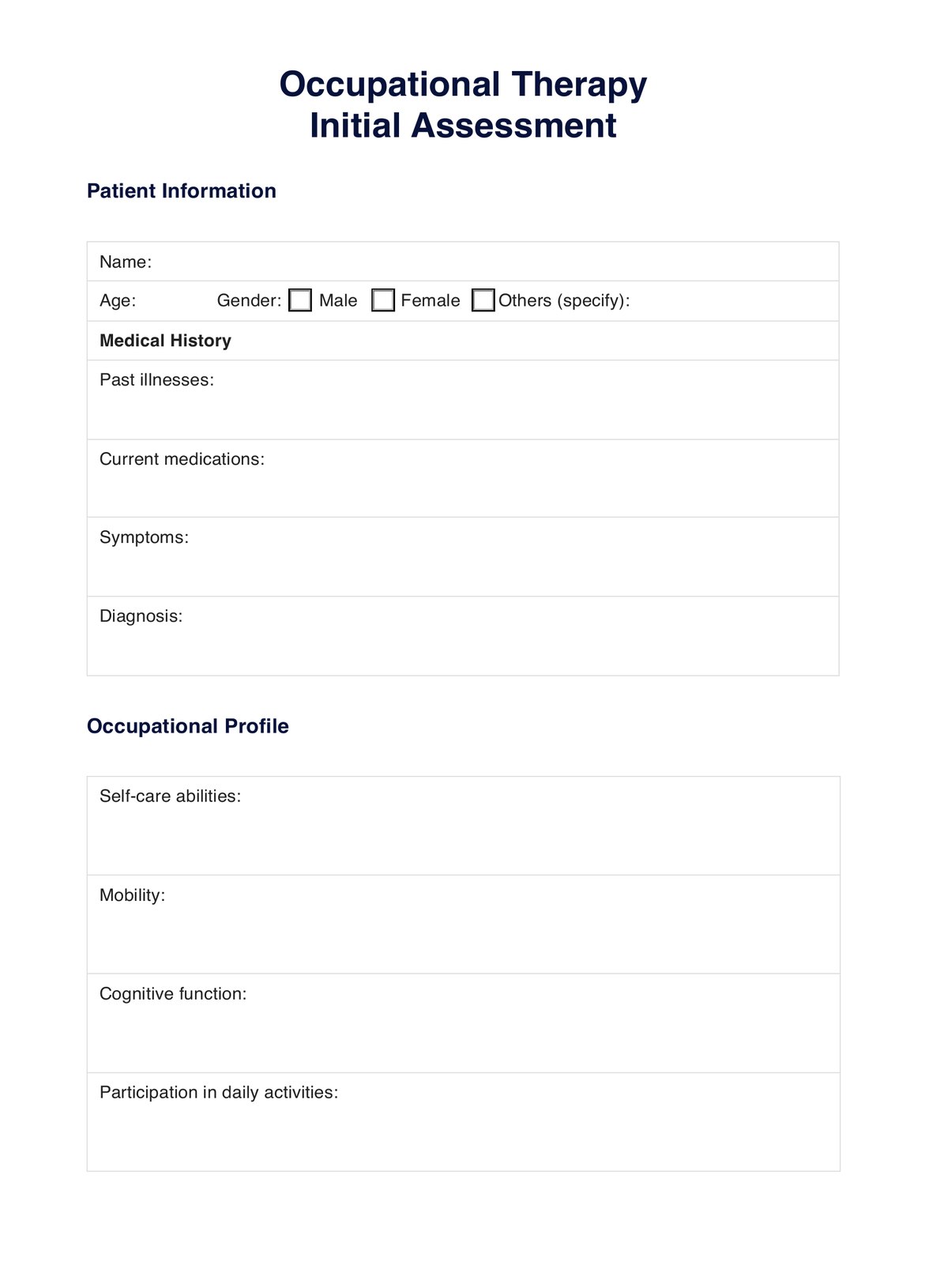
Occupational Therapy Initial Assessment Template
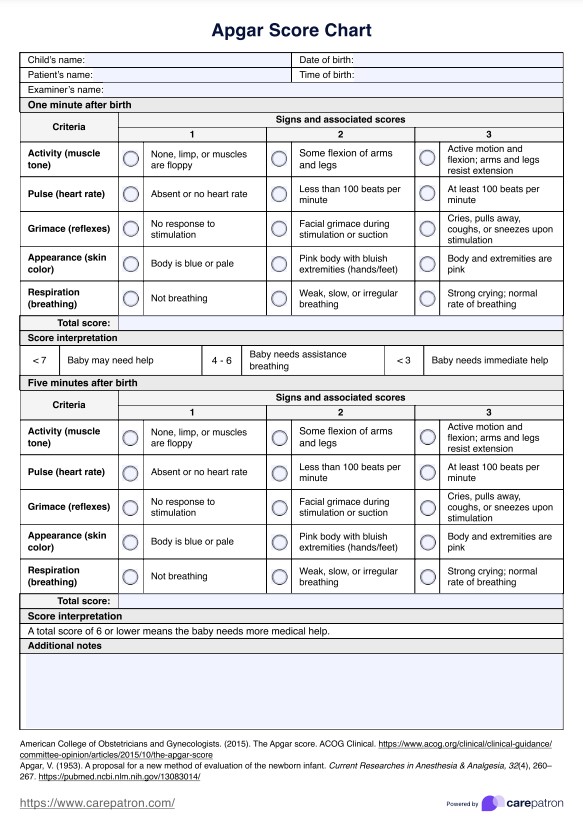
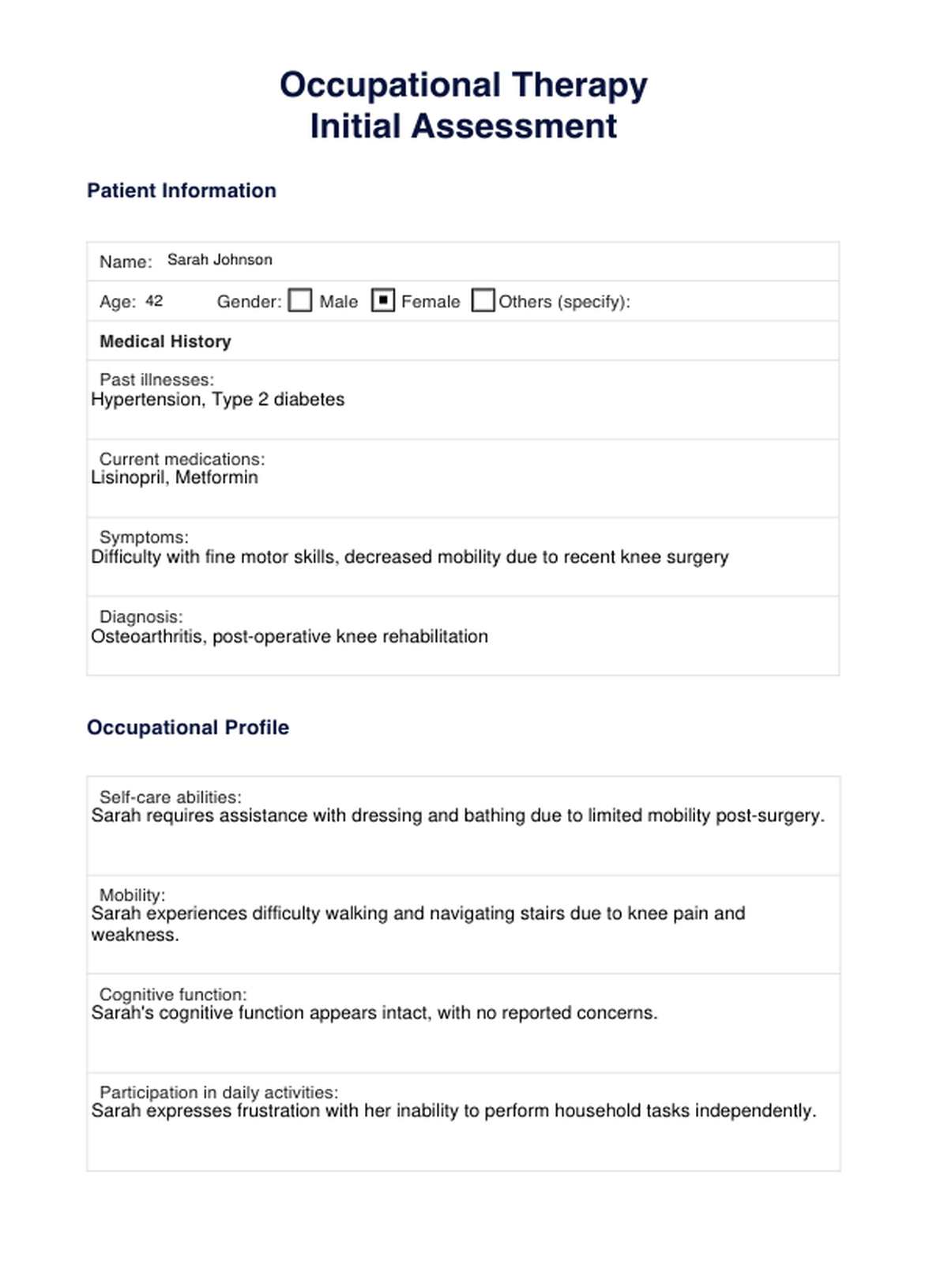
Occupational Therapy Initial Assessment Template Example
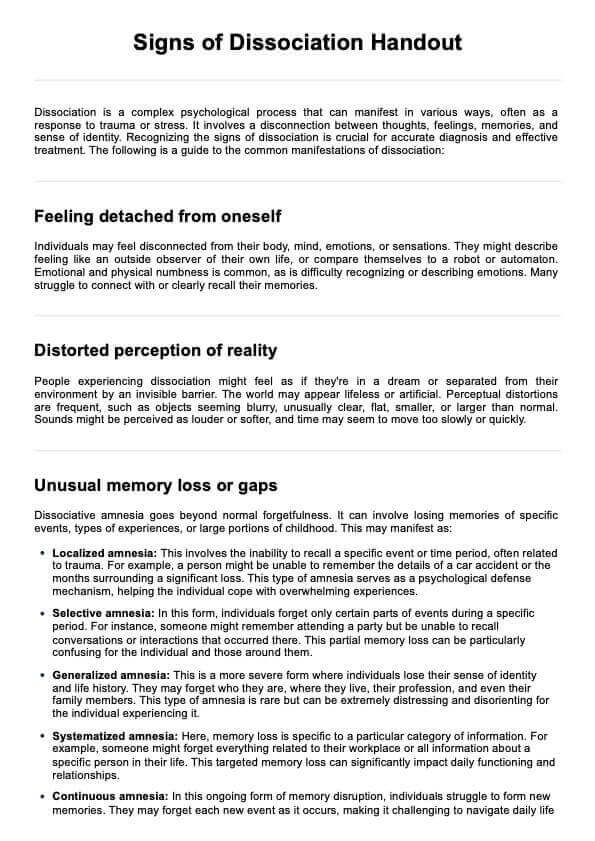
What is an occupational therapy initial assessment?
An occupational therapy initial assessment is the first step in the occupational therapy process when working with a new client. It involves gathering information about the client's medical history, current functional abilities, goals, and environmental factors that may affect their participation in daily activities.
The initial assessment typically includes several components:
- Client interview: The occupational therapist (OT) thoroughly interviews the client to understand their medical history, current concerns, and goals. This may include questions about the client's ability to perform daily activities, any pain or discomfort they experience, previous treatments or therapies, and home and work environments.
- Observation: The OT observes the client's physical, cognitive, sensory, and emotional abilities during various activities. This observation helps the therapist understand the client's strengths, limitations, and areas needing improvement.
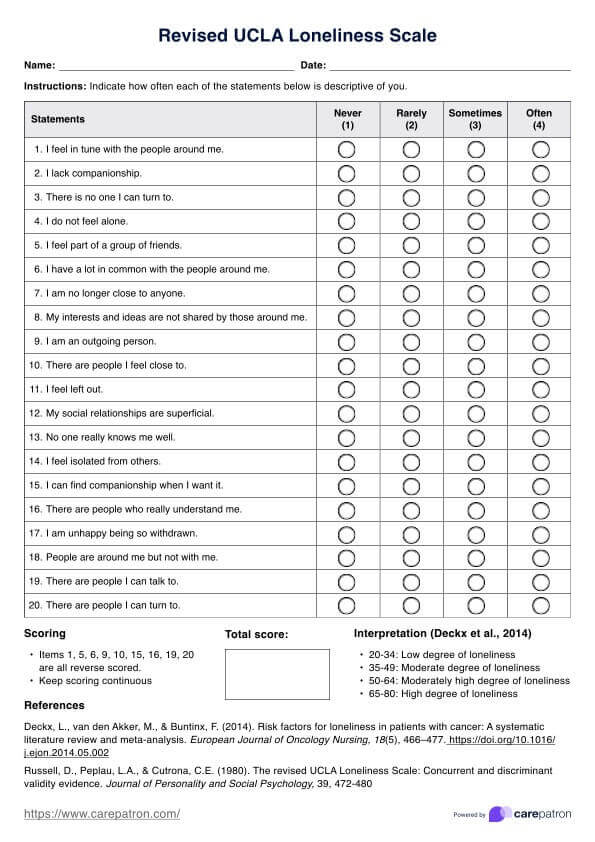
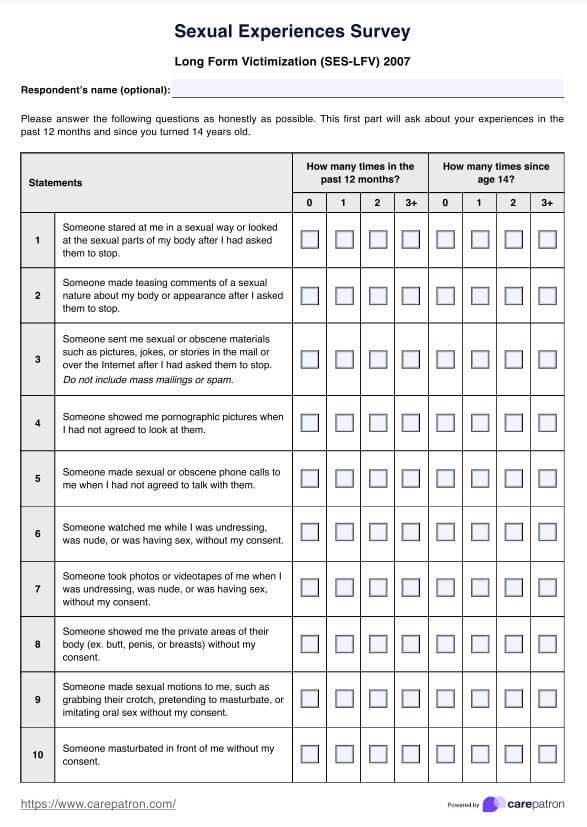
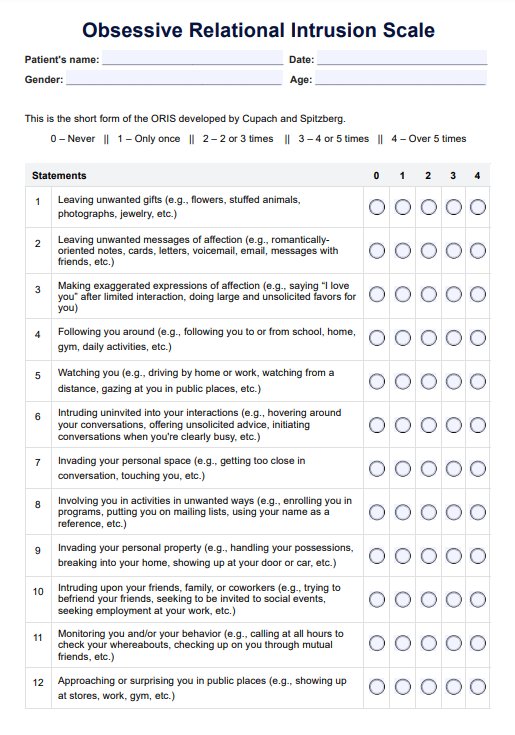
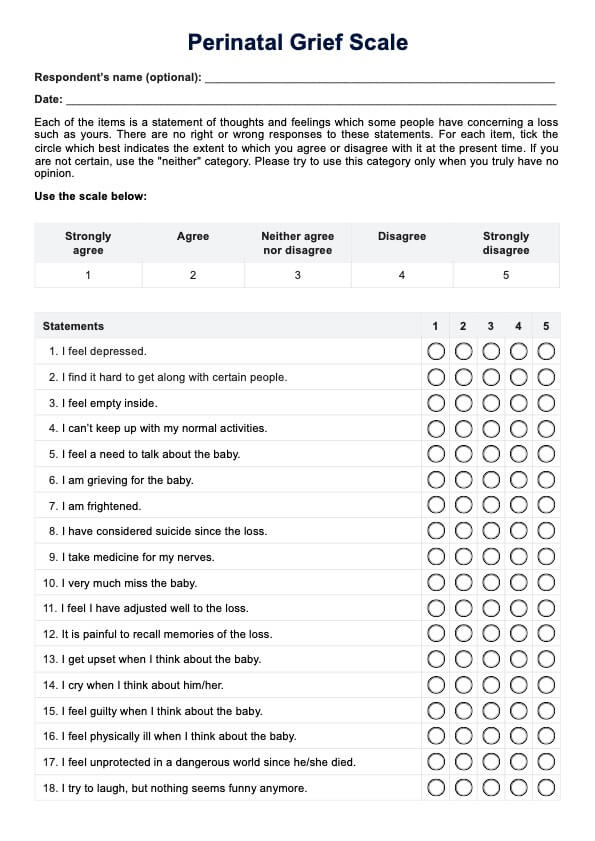
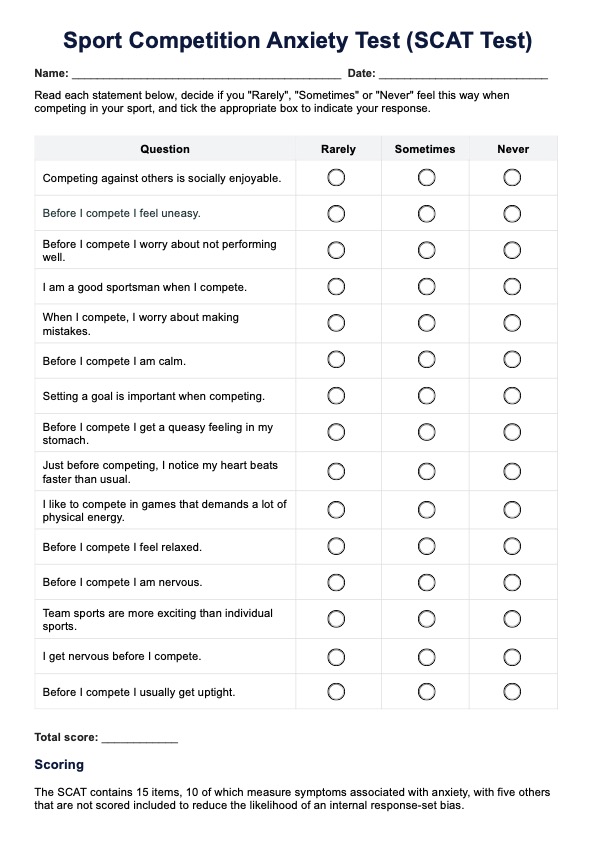
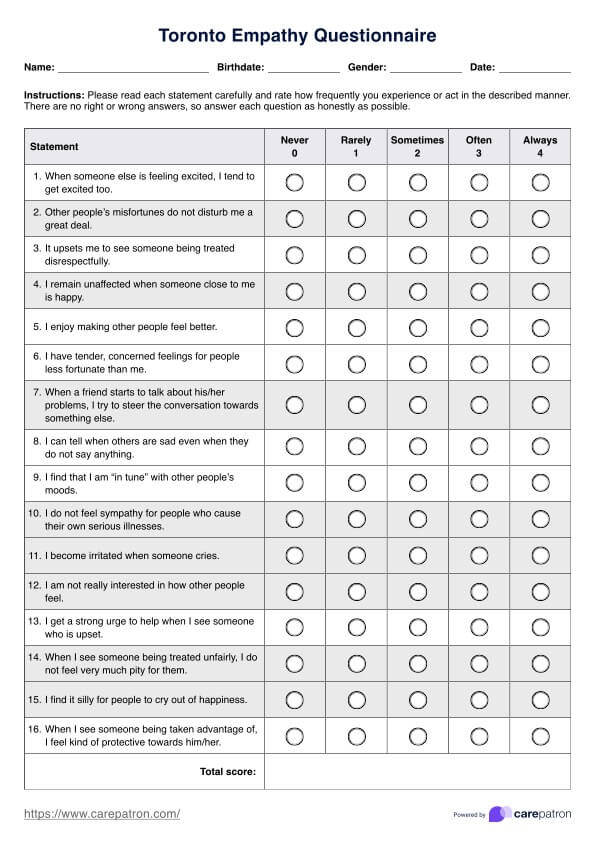
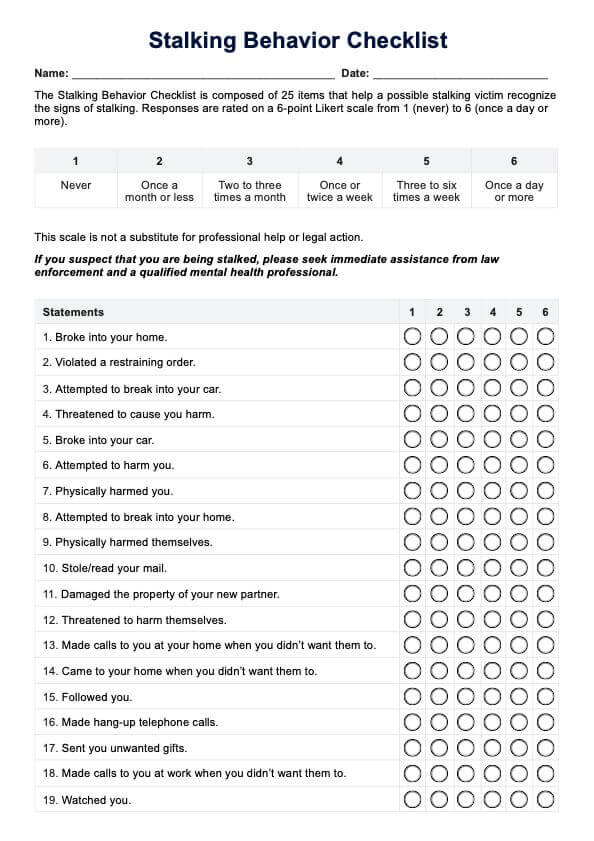
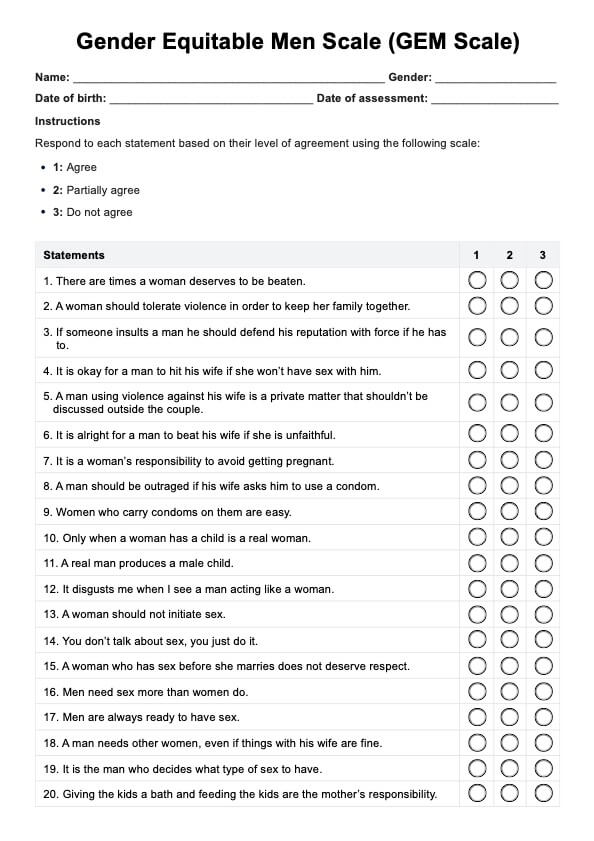
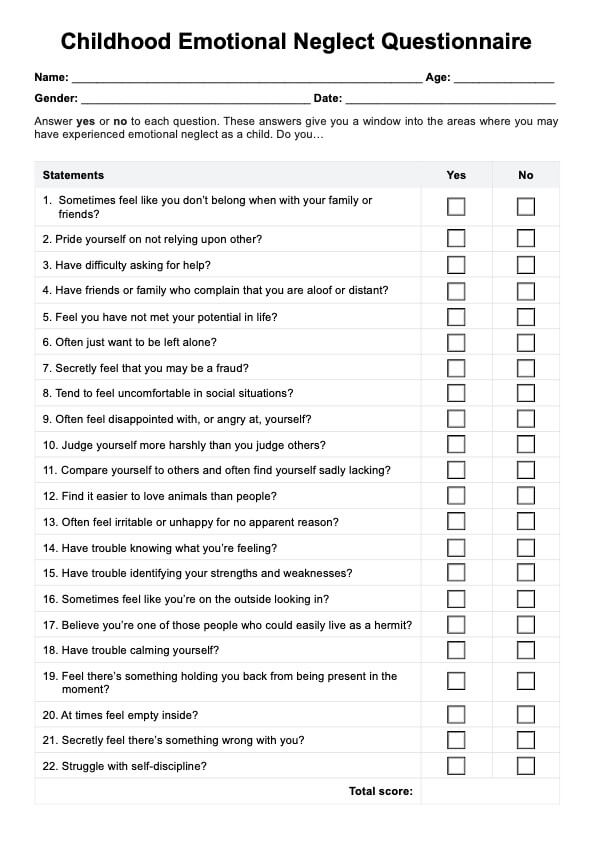
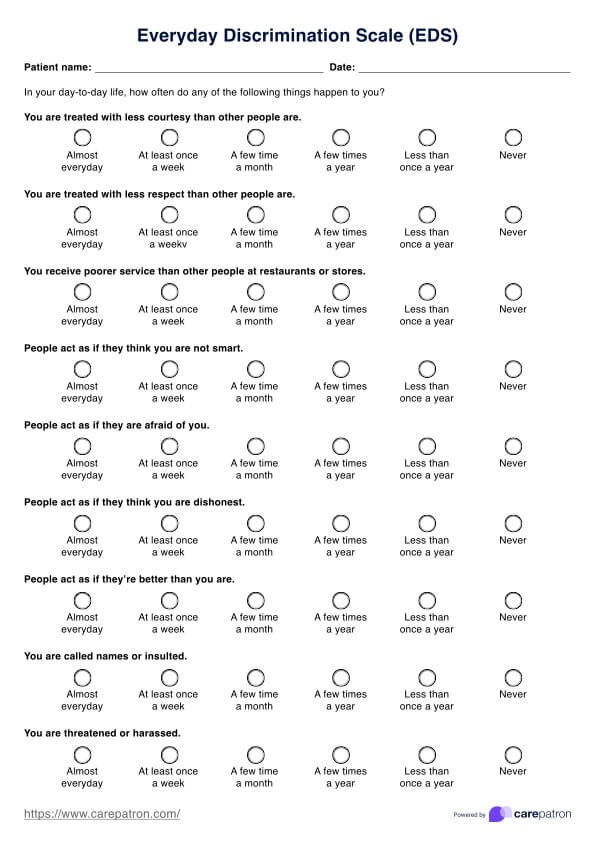
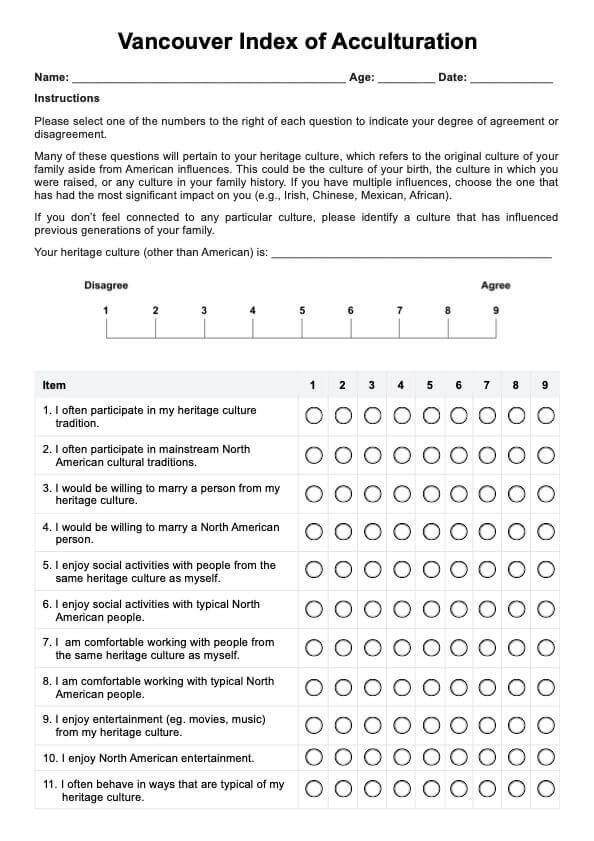
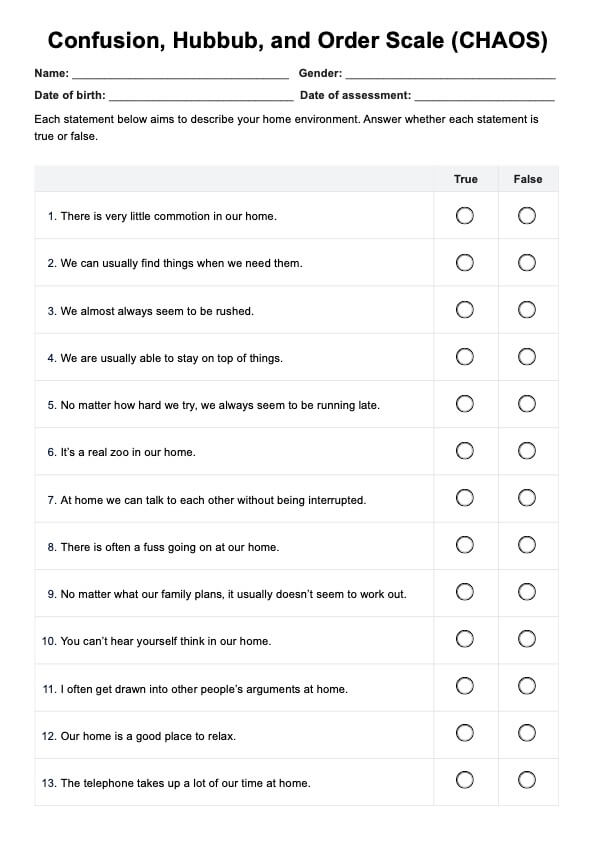
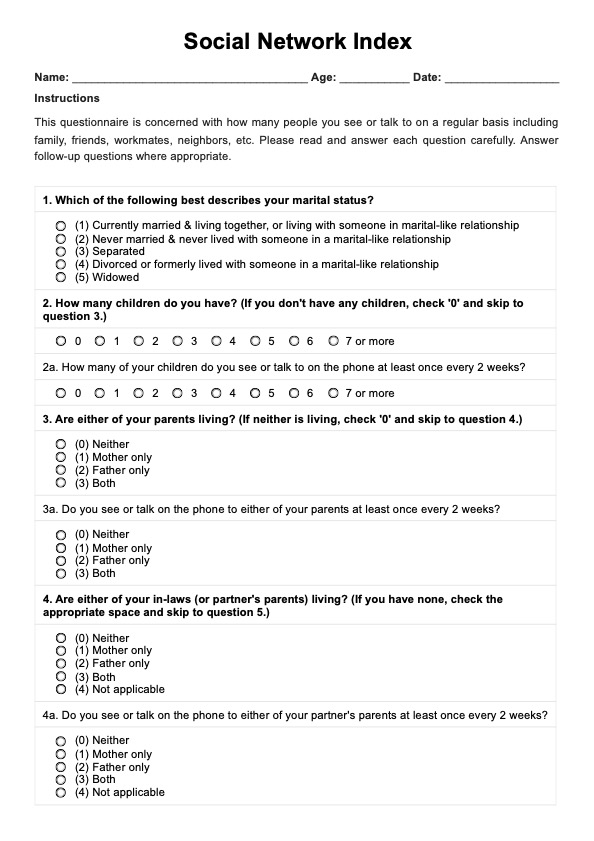
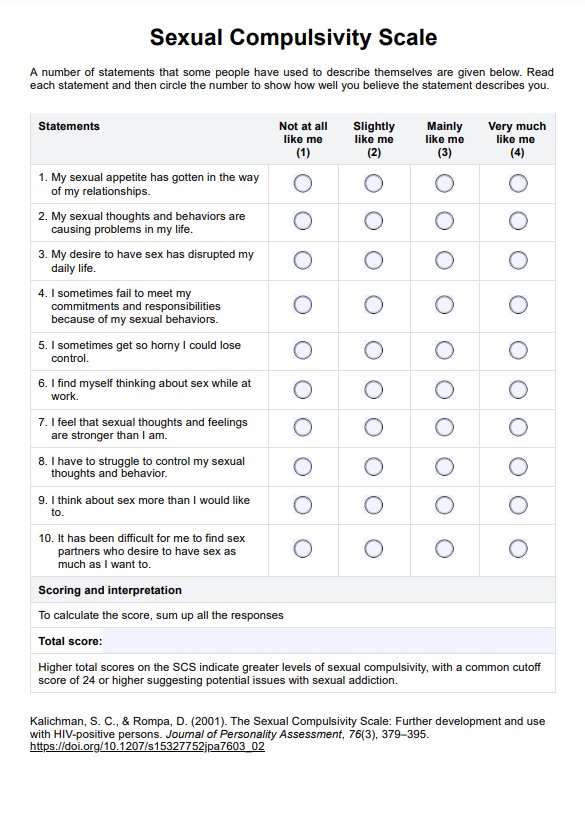
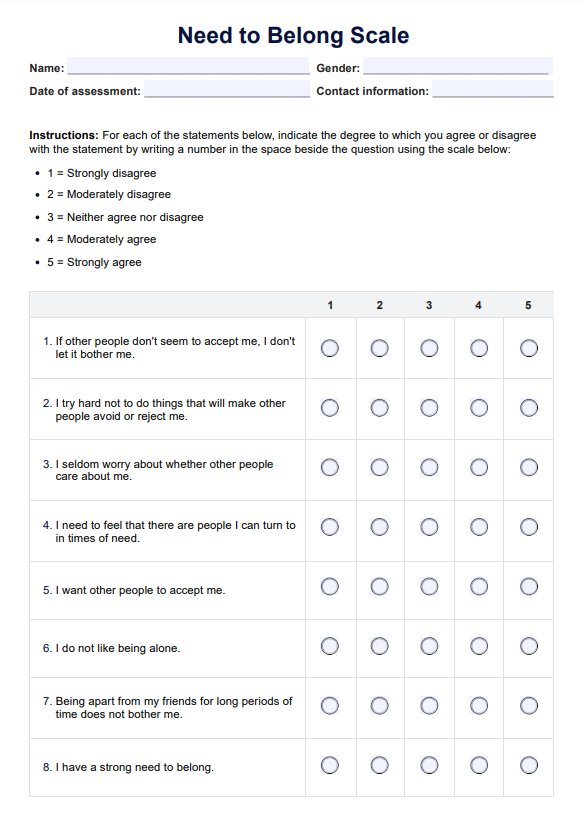
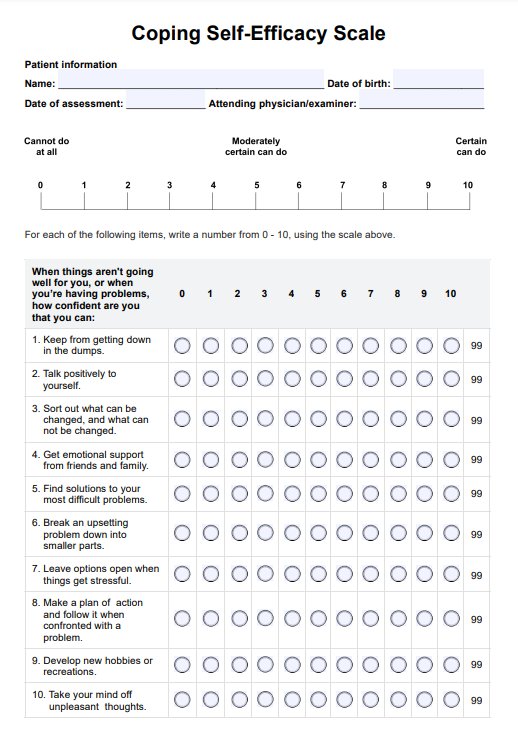
- Assessment tools: Occupational therapists may use standardized assessment tools to evaluate specific skills or areas of function. These tools can assess motor skills, sensory processing, cognitive abilities, activities of daily living (ADLs), instrumental activities of daily living (IADLs), and more.
- Functional assessment: The OT assesses the client's ability to perform various daily activities, such as dressing, bathing, cooking, and managing household tasks. This assessment may include observing the client performing these activities or asking them to demonstrate specific tasks.
- Goal setting: Based on the information gathered during the assessment, the OT collaborates with the client to establish realistic and meaningful goals for therapy. These goals are tailored to the client's needs and preferences and serve as a roadmap for the treatment plan.
- Environmental assessment: The OT may assess the client's home, work, school, or community environments to identify any barriers or challenges impacting their participation in daily activities. This assessment helps the therapist make recommendations for environmental modifications or assistive devices.
How does our Occupational Therapy Initial Assessment Template work?
Our Occupational Therapy Initial Assessment Template is a comprehensive tool to gather essential information about the patient's medical history, development, current abilities, and therapy goals. It enables occupational therapists and other healthcare professionals to assess the patient's functional status and develop an individualized treatment plan to address their needs effectively.
Key components of our template include:
- Patient's medical history: Gather details about the patient's medical conditions, past illnesses, current medications, and symptoms to understand their health status comprehensively.
- Occupational profile: Document the patient's self-care abilities, mobility, cognitive function, and participation in daily activities to establish a clear understanding of their needs and priorities.
- Assessment of functional abilities: Assess the patient's motor skills, self-care abilities, and performance in domestic tasks and instrumental activities of daily living using standardized measures and evaluation forms.
- Environmental assessment: Identify any environmental barriers or challenges that may affect the patient's ability to function independently at home, work, or school.
- Goal setting: Collaborate with the patient to establish time-bound goals that improve their function, participation, and overall well-being.
- Treatment plan: Develop a detailed treatment plan outlining the interventions, resources, and equipment needed to effectively address the patient's goals.
- Documentation of progress: Document the patient's progress, including any changes in function, symptoms, or participation in therapy sessions.
- Coordination with other healthcare professionals: Facilitate integration of services by communicating with other healthcare professionals and making referrals as needed.
Why is the initial assessment portion of occupational therapy important?
The initial assessment in the form of occupational therapy is crucial for several reasons:
- Understanding the patient's needs: The initial assessment allows occupational therapists to gather comprehensive information about their medical history, current abilities, goals, and environmental factors that may impact their daily living. This understanding forms the foundation for developing a personalized treatment plan tailored to the patient's needs.
- Setting clear goals: Through the assessment process, therapists can identify specific areas where the patient may be struggling and set clear, measurable goals for therapy. These goals provide direction for treatment and serve as benchmarks for tracking progress over time.
- Identifying barriers to function: Assessing the patient's functional abilities and environmental factors helps therapists identify potential barriers to participation in daily activities. This may include physical limitations, cognitive impairments, or challenges related to the home or work environment.
- Customizing treatment plans: Based on the assessment findings, therapists can develop individualized treatment plans tailored to patients' needs, goals, and preferences. This may include therapeutic exercises, adaptive strategies, environmental modifications, and assistive devices to promote optimal outcomes.
- Enhancing collaboration: The initial assessment also allows therapists to collaborate with other healthcare professionals, such as physicians, physical therapists, and psychologists, to ensure comprehensive care. By sharing assessment findings and treatment goals, therapists can facilitate integrated care and enhance the overall effectiveness of therapy.
What are the benefits of using this initial assessment template?
Using the Occupational Therapy Initial Assessment Template offers access to this data with several benefits for medical professionals:
- Structured approach: The template provides a structured framework for conducting initial assessments, ensuring that all relevant aspects of the patient's medical history, functional abilities, goals, and environmental factors are thoroughly addressed.
- Comprehensive documentation: By following the template, healthcare professionals can document assessment findings, treatment goals, interventions, and progress notes in a thorough and organized manner, facilitating clear communication and continuity of care.
- Efficiency: The template streamlines the assessment process, saving time and effort for medical professionals. It helps prioritize assessment components and guides practitioners through each step, reducing the likelihood of overlooking important information.
- Customization: While the template offers a standardized format, it also allows for customization to meet the unique needs of individual patients. Medical professionals can adapt the template to incorporate specific assessment tools, treatment modalities, and patient preferences.
- Quality assurance: Consistent template use promotes adherence to best practices in occupational therapy assessment and documentation. It helps ensure that evaluations are conducted systematically and thoroughly, enhancing the quality and effectiveness of patient care.
- Facilitation of communication and collaboration: The template facilitates communication and cooperation among healthcare team members by providing a standardized format for documenting assessment findings and treatment plans. It helps promote interdisciplinary collaboration and ensures that all relevant information is readily accessible to other providers involved in the patient's care.
Commonly asked questions
The initial assessment for occupational therapists is the first step in evaluating a client's needs, abilities, and goals to develop and complete a personalized treatment and intervention plan.
Commonly used assessments in occupational therapy include the Functional Independence Measure (FIM), the Canadian Occupational Performance Measure (COPM), the Assessment of Motor and Process Skills (AMPS), and the Mini-Mental State Examination (MMSE).
The first step in the occupational therapy evaluation, diagnosis, and referral process is typically conducting an initial interview with the client to gather information about their medical history, current concerns, and goals.











-template.jpg)