SARC-F Questionnaire
Use the SARC-F Questionnaire for sarcopenia diagnosis. Easy to administer and helps in early identification and management.


What is sarcopenia?
Losing muscle mass is normal with age and can, in fact, start as early as the 30s. Low muscle mass can affect daily physical functions like standing, walking, and carrying items. However, some people may experience this in a rapid fashion, which is known as sarcopenia, a serious condition that significantly affects quality of life by causing involuntary loss of muscle mass and strength.
Sarcopenia symptoms
It is important to advise individuals, especially elderly patients, to watch for signs of sarcopenia, which can lead to poor functional outcomes and reduced physical performance. Symptoms include (Duque et al., 2024; Office on Women's Health, 2023):
- Falling
- Muscle weakness
- Slow walking speed
- Difficulty with daily activities (e.g., rising from a chair, opening a jar)
- Self-reported muscle wasting
Body mass index (BMI) is also used to assess individuals' nutritional condition and health status, which can be a factor in sarcopenia.
Risk factors and causes of sarcopenia
As mentioned earlier, sarcopenia comes with age-related factors. The European Working Group on Sarcopenia in Older People (EWGSOP) defined age-related sarcopenia. In 2010, it was initially recommended that the diagnosis be made by identifying both low muscle mass and poor muscle function (strength or performance). However, EWGSOP's updated consensus in 2019 emphasizes low muscle strength as a key feature of sarcopenia (Cruz-Jentoft et al., 2018; Wallengren et al., 2021).
Worldwide, 10-16% of the aging population is affected by sarcopenia, with a higher prevalence in certain patient groups. In diabetic patients, it ranges from 18% to 66% in those with advanced esophageal cancer (Yuan & Larsson, 2023). Causes and risks of sarcopenia can be classified into three: age-related factors, lifestyle factors, and chronic diseases.
Age-related changes include lower hormone levels and a reduced ability to convert protein into muscle. Concurrently, lifestyle factors such as inactivity, lack of exercise, loss of mobility, and dental and oral problems can further exacerbate health issues. Additionally, chronic conditions like bone and joint diseases, endocrine diseases, cancer, and cardiovascular disease also serve as risk factors for sarcopenia (Aging in Motion, n.d.).
Problems sarcopenia may lead to due to muscle mass loss
Sarcopenia can lead to several adverse outcomes. It often causes weakness and frailty, which can make everyday tasks like climbing stairs difficult. This loss of muscle strength increases the risk of falls and fractures, which can greatly influence an individual's mobility and independence. Additionally, sarcopenia can contribute to poor posture and balance issues, further complicating physical activity and overall quality of life. Addressing sarcopenia is crucial, as it affects not only physical function but also has significant implications for overall health and longevity.
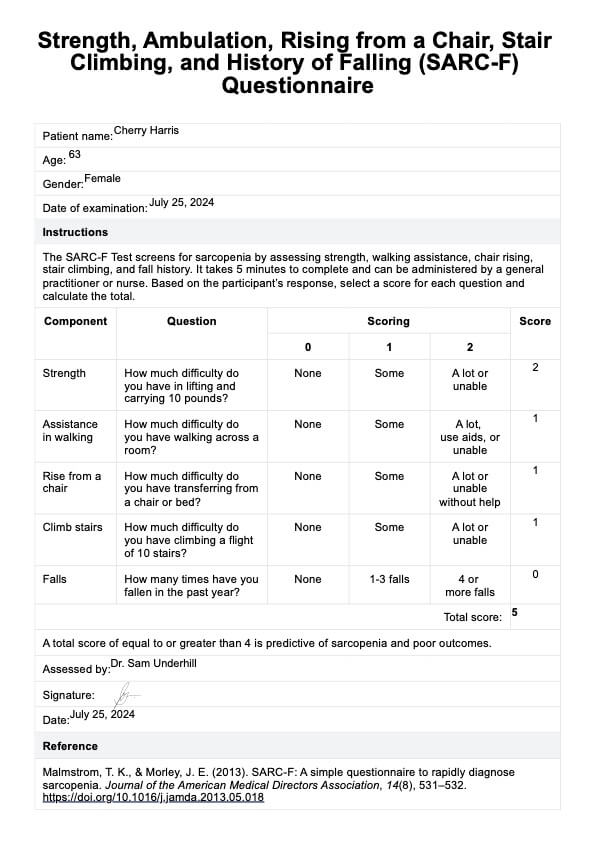
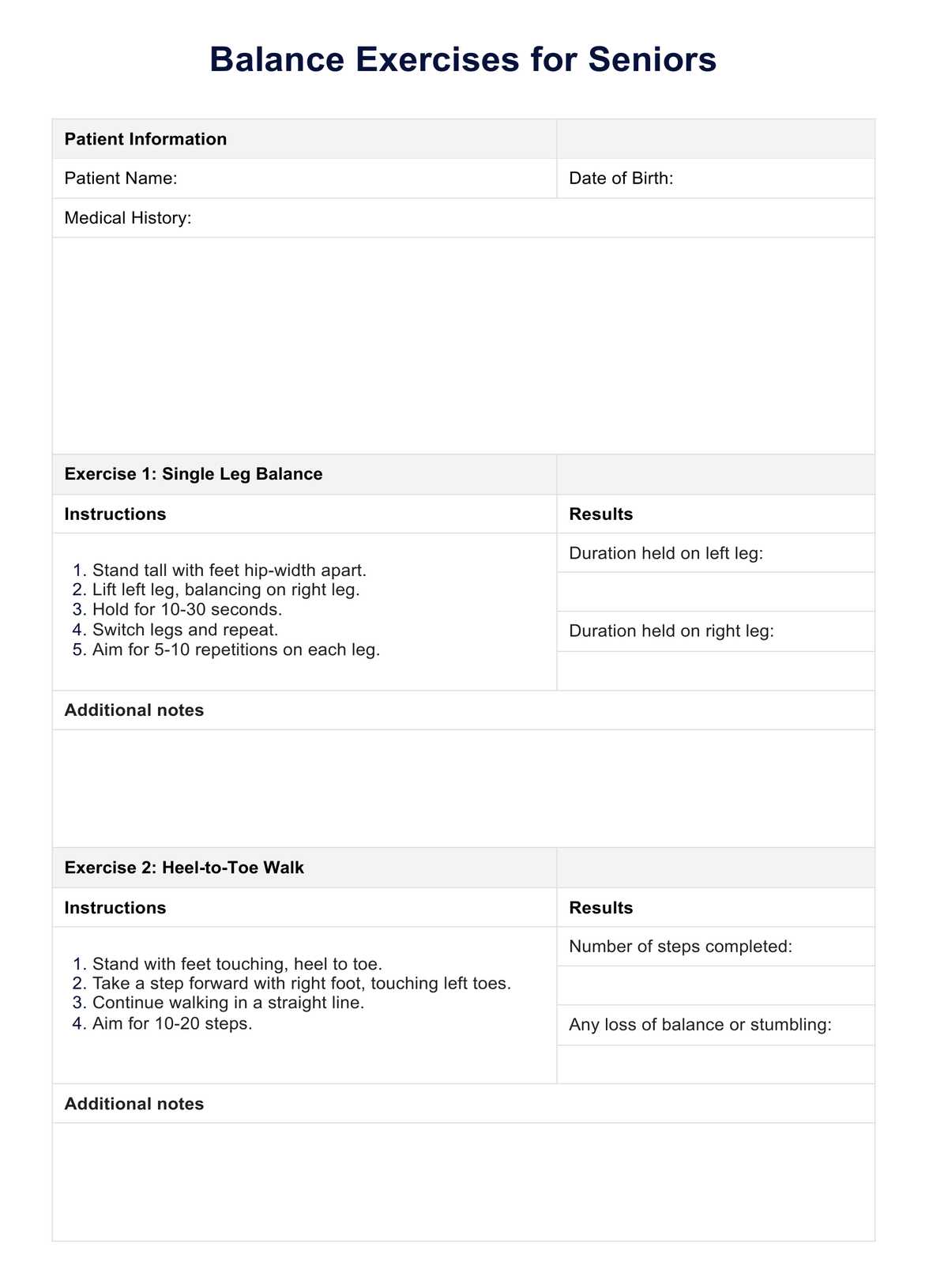
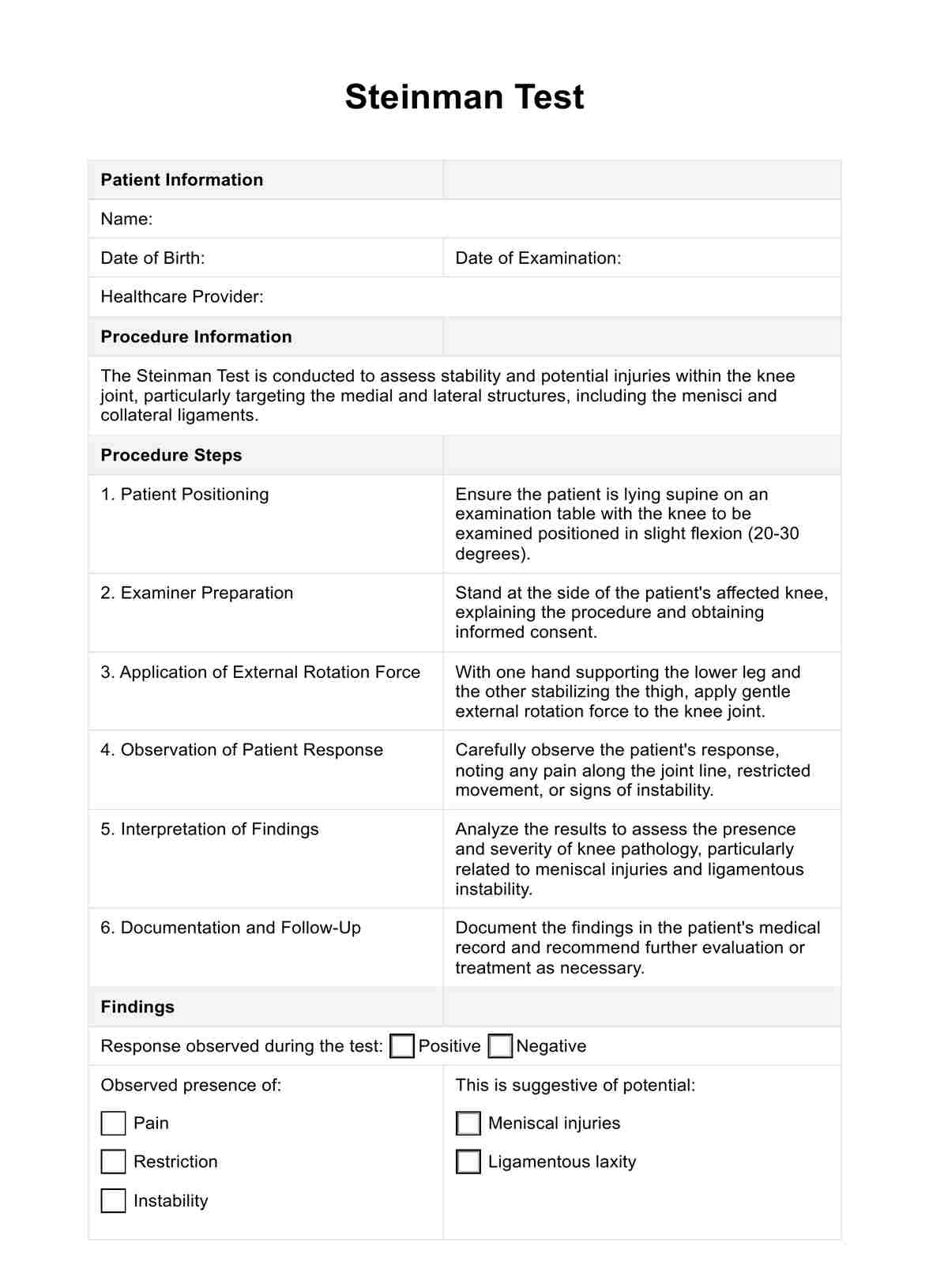
SARC-F Questionnaire Template
SARC-F Questionnaire Example
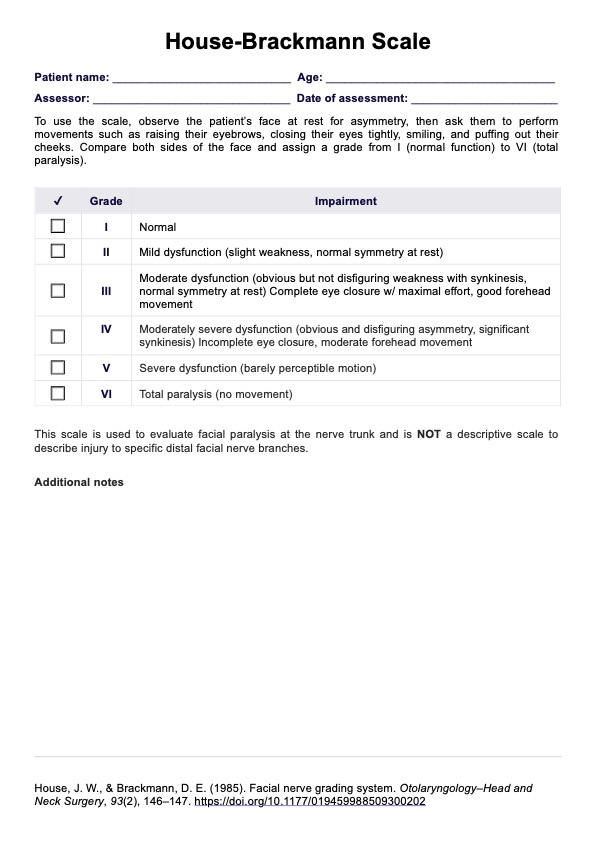
What is the SARC-F Questionnaire?
The Strength, Ambulation, Rising from a Chair, Stair Climbing, and History of Falling or SARC-F Questionnaire is a screening tool for sarcopenia by Maelstrom and Morley (2013). In a validation study, the SARC-F showed high specificity but low sensitivity. However, it is deemed a suitable tool for community screening for sarcopenia (Woo et al., 2014) and screening the condition in the elderly (Lu et al., 2020).
The questionnaire has five simple questions that assess sarcopenia by looking into an individual's strength, walking assistance, chair rising, stair climbing, and fall history (Malmstrom et al., 2015). It takes only 5 minutes to complete and can be administered by a general practitioner or nurse.
Which healthcare professionals use this?
The SARC-F Questionnaire is commonly used by healthcare professionals such as:
- Primary care physicians
- Geriatricians
- Physical therapists
- Dietitians/nutritionists
- Nurses
This tool helps these professionals identify individuals at risk for sarcopenia, enabling early intervention and management.
How is it scored, and how are the results interpreted?
The SARC-F Questionnaire is scored by summing the responses to its five questions, with each answer scored from 0 to 2 points. The total score ranges from 0 to 10. A score of 4 or more suggests the presence of sarcopenia or a high risk of developing it.
How to use our SARC-F Questionnaire template
The SARC-F Questionnaire template helps identify individuals at risk of sarcopenia. Following these steps, you can effectively use the questionnaire to assist in sarcopenia screening.
Step 1: Download the template
First, download the SARC-F Questionnaire template from the link we provided. Ensure you have a digital or printed copy ready during the assessment.
Step 2: Use during assessment
Administer the questionnaire to the patient or individual being assessed. Ask them to answer each of the five questions, which focus on strength, difficulty walking, and other factors related to muscle health. Record their responses accurately to calculate the total score.
Step 3: Store for future use
After completing the assessment, store the filled-out questionnaire in the patient's file or digital records. This will allow for future reference and monitoring of any changes in muscle health over time.
Sarcopenia treatments
After diagnosing sarcopenia, treatment options usually focus on lifestyle modifications. Here are some ways to treat or manage sarcopenia, especially in older adults:
Resistance training
Doing exercises like weight lifting helps build and strengthen muscles, making daily activities easier and improving overall physical function. Regular resistance training can slow down muscle loss and even help gain muscle mass.
Nutritional interventions
Eating enough protein and sometimes taking supplements can support muscle repair and growth. Good nutrition helps ensure your muscles get the nutrients they need to stay strong and healthy.
Physical activity
Regular exercise, such as walking or swimming, improves muscle function and mobility. Staying active helps prevent further muscle loss and keeps you moving more freely.
References
Aging in Motion. (n.d.). Sarcopenia facts and figures [Fact sheet]. https://www.aginginmotion.org/app/uploads/2021/07/Sarcopenia-Facts-and-Figures-2.pdf
Cruz-Jentoft, A. J., Bahat, G., Bauer, J., Boirie, Y., Bruyère, O., Cederholm, T., Cooper, C., Landi, F., Rolland, Y., Sayer, A. A., Schneider, S. M., Sieber, C. C., Topinkova, E., Vandewoude, M., Visser, M., Zamboni, M., Bautmans, I., Baeyens, J.-P., Cesari, M., & Cherubini, A. (2018). Sarcopenia: Revised European consensus on definition and diagnosis. Age and Ageing, 48(1), 16–31. https://doi.org/10.1093/ageing/afy169
Duque, G., Hajj-Boutros, G., & Morais, J. A. (2024, June 21). Sarcopenia - symptoms, diagnosis and treatment. BMJ Best Practice. https://bestpractice.bmj.com/topics/en-us/3000319
Lu, J.-L. ., Ding, L.-Y. ., Xu, Q., Zhu, S., Xu, X.-Y. ., Hua, H.-X. ., Chen, L., & Xu, H. (2020). Screening accuracy of SARC-F for sarcopenia in the elderly: A diagnostic meta-analysis. J Nutr Health Aging, 25(2), 172–182. https://doi.org/10.1007/s12603-020-1471-8
Malmstrom, T. K., & Morley, J. E. (2013). SARC-F: A simple questionnaire to rapidly diagnose sarcopenia. J Am Med Dir Assoc, 14(8), 531–532. https://doi.org/10.1016/j.jamda.2013.05.018
Malmstrom, T. K., Miller, D. K., Simonsick, E. M., Ferrucci, L., & Morley, J. E. (2015). SARC-F: A symptom score to predict persons with sarcopenia at risk for poor functional outcomes. J Cachexia Sarcopenia Muscle, 7(1), 28–36. https://doi.org/10.1002/jcsm.12048
Office on Women's Health. (2023, August 23). Sarcopenia. Office of the Assistant Secretary for Health. https://www.womenshealth.gov/sarcopenia
Rolland, Y., & Vellas, B. (2010). Sarcopenia. In H. M. Fillit, K. Rockwood, & K. Woodhouse (Eds.), Brocklehurst's textbook of geriatric medicine and gerontology (7th ed., pp. 587-593). W.B. Saunders. https://doi.org/10.1016/B978-1-4160-6231-8.10073-X
Wallengren, O., Bosaeus, I., Frändin, K., Lissner, L., Falk Erhag, H., Wetterberg, H., Rydberg Sterner, T., Rydén, L., Rothenberg, E., & Skoog, I. (2021). Comparison of the 2010 and 2019 diagnostic criteria for sarcopenia by the European working group on sarcopenia in older people (EWGSOP) in two cohorts of Swedish older adults. BMC Geriatrics, 21(1). https://doi.org/10.1186/s12877-021-02533-y
Woo, J., Leung, J., & Morley, J. E. (2014). Validating the SARC-F: A suitable community screening tool for sarcopenia? J Am Med Dir Assoc, 15(9), 630–634. https://doi.org/10.1016/j.jamda.2014.04.021
Yuan, S., & Larsson, S. C. (2023). Epidemiology of sarcopenia: Prevalence, risk factors, and consequences. Metabolism, 144(155533), 155533. https://doi.org/10.1016/j.metabol.2023.155533
Commonly asked questions
No medications are currently approved to treat or cure sarcopenia, but specific treatments and supplements can help manage and slow its progression.
The SARC-F Questionnaire includes five components: assessing strength, difficulty climbing stairs, walking ability, frequency of falls, and overall muscle weakness. Each question helps evaluate different aspects of muscle health and function.
Baumgartner et al. performed DEXA (bone-density) scans to measure muscle mass in the four limbs of the body, defining the skeletal muscle mass index (SMI) as appendicular skeletal muscle mass (ASM) divided by height squared (kg/m²). Sarcopenia was identified when an individual's SMI was two standard deviations below the average of a reference group of middle-aged men and women (Rolland & Yves, 2010).