Severity of Dependence Scale (SDS)
Evaluate substance dependence with the Severity of Dependence Scale (SDS)—an accurate assessment for effective healthcare interventions.


What is substance dependence?
, also referred to as substance use disorder, is a complex and chronic condition characterized by a compulsive and often uncontrollable urge to use a specific substance, despite its negative consequences to an individual's physical, mental, and social well-being. This condition involves a spectrum of substances, including alcohol, illicit drugs, prescription medications, and even behaviors like gambling.
Key features of substance dependence include tolerance, withdrawal, and a loss of control over use. Tolerance develops as the body adapts to the substance, requiring larger amounts to achieve the desired effects. When usage is reduced or stopped, physical and psychological withdrawal symptoms manifest, driving the individual to seek the substance to alleviate discomfort.
Loss of control is a hallmark sign where an individual finds it increasingly challenging to limit or control their substance use, often leading to excessive consumption even when aware of the harm it causes. This loss of control can impact various aspects of life, from work and education to relationships and personal responsibilities.
Psychological aspects are also prominent in substance dependence. Cravings and preoccupation with obtaining and using the substance become consuming, often overshadowing other priorities. As dependence progresses, the brain's reward system changes, reinforcing the cycle of substance use and diminishing the ability to experience pleasure from other sources.
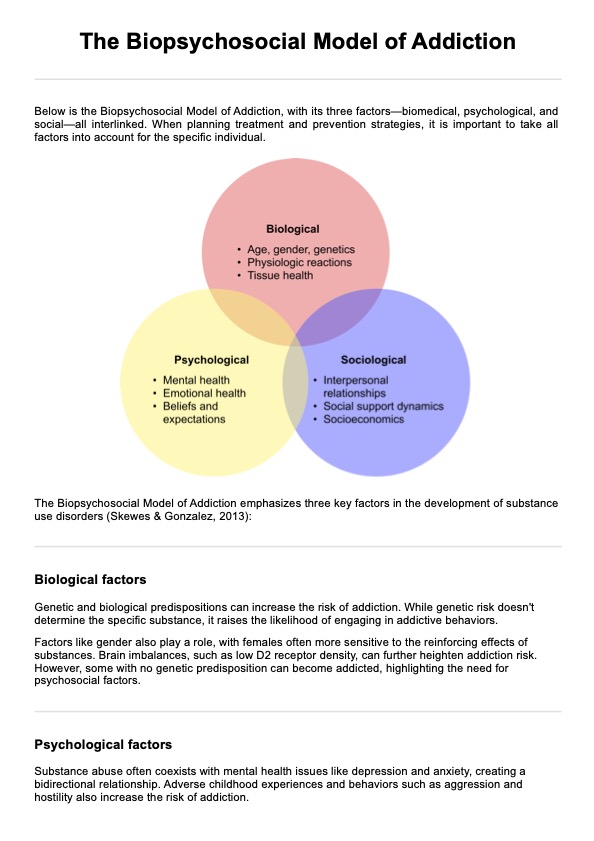
Substance dependence is a multifaceted condition with biological, psychological, and environmental factors contributing to its development. Genetic predisposition, traumatic experiences, mental health disorders, and social influences can all play roles. Effective treatment involves a comprehensive approach that addresses dependence's physical, emotional, and social aspects. Behavioral therapies, counseling, medication, and support groups are common components of treatment plans tailored to the individual's needs and circumstances.
Recognizing substance dependence as a medical condition rather than a moral failing is crucial for fostering empathy and providing appropriate care. Early intervention and comprehensive support are essential for helping individuals break free from the cycle of substance dependence and regain control over their lives.
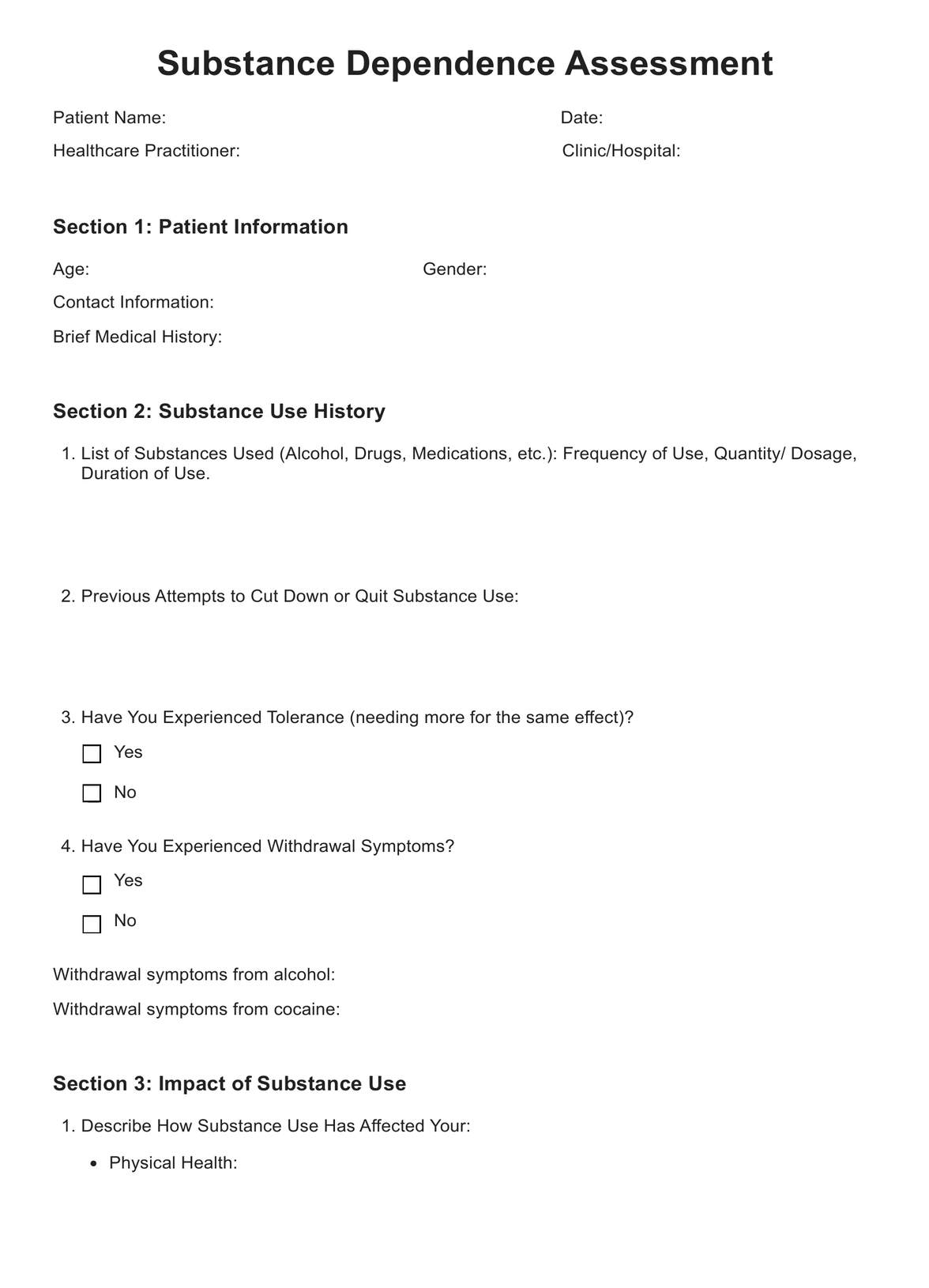
Severity of Dependence Scale (SDS) Template
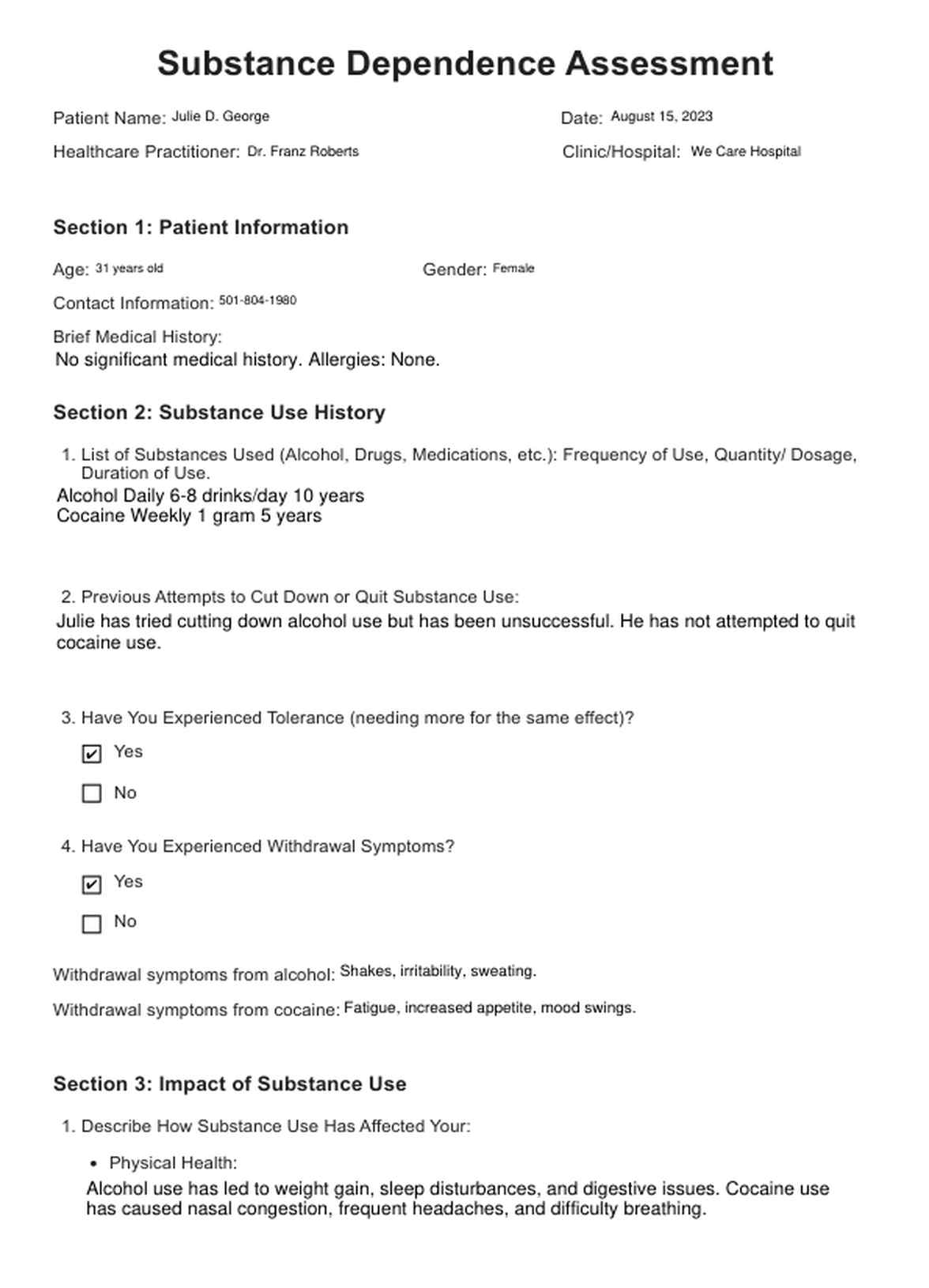
Severity of Dependence Scale (SDS) Example
How to use the Severity of Dependence Scale (SDS):
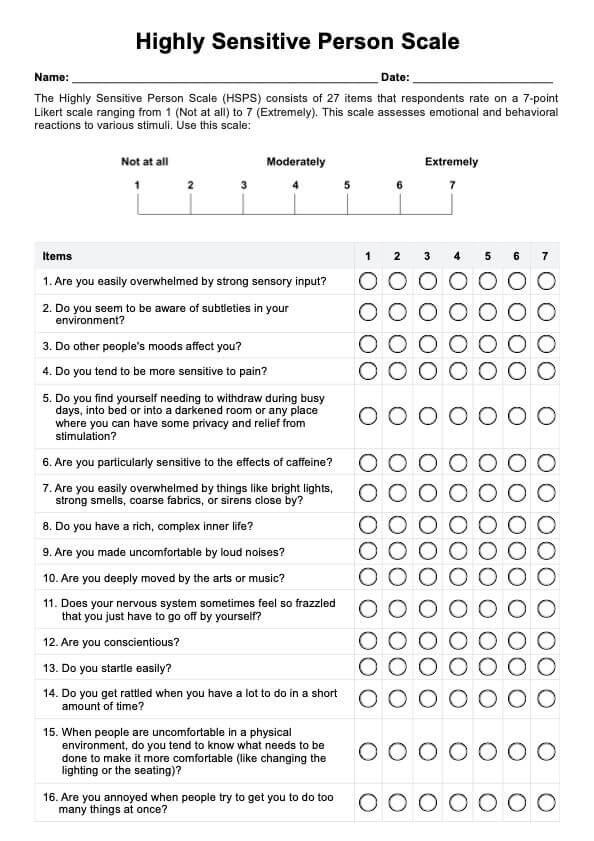
The Severity of Dependence Scale (SDS) is a valuable tool used in healthcare to assess the severity of substance dependence. It provides clinicians with insights into the degree of support a person has on a particular substance, aiding in treatment planning and interventions.
Here are the steps in using the Severity of Dependence Scale (SDS):
Step 1: Introduction
Begin by explaining the purpose of the assessment to the patient. Emphasize that their honest responses will help tailor an effective treatment plan.
Step 2: Familiarization
Ensure the patient understands the SDS questions and scale. Clarify that their answers will reflect their experiences with the specific substance(s) they are dependent on.
Step 3: Questionnaire Administration
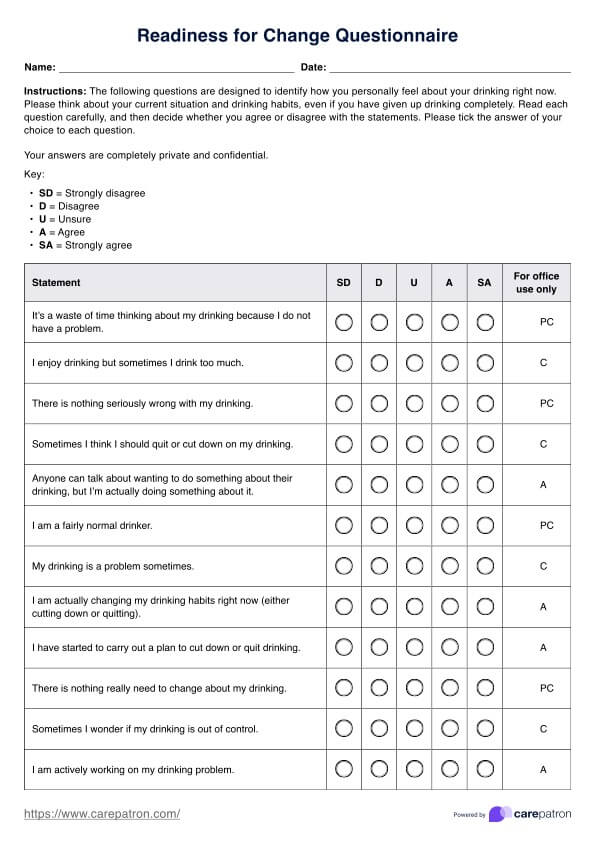
Administer the SDS questionnaire from the template. Ask the patient to respond to each item based on their substance use behavior.
Step 4: Scoring
Calculate the total score by adding up the scores assigned to each item. The scale typically ranges from 0 to 15, with higher scores indicating higher dependence.
Step 5: Interpretation
Interpret the score in the context of the patient's overall situation. Scores can be categorized into levels of dependence, such as mild, moderate, or severe, to guide treatment decisions.
Step 6: Discussion
Discuss the patient's score with them. Address any questions they have about the assessment and its implications. Use the score as a starting point for a more in-depth conversation about their substance use habits and desire for change.
Step 7: Treatment Planning
Develop a treatment plan collaboratively based on the SDS score and the patient's circumstances. This plan may include therapy, counseling, medical interventions, and support groups.
Step 8: Ongoing Assessment
The SDS can also be used to track progress throughout the treatment journey. Periodically administer the assessment to monitor changes in dependence severity and adjust the treatment plan accordingly.
When would you use this Severity of Dependence Scale (SDS)?
The Severity of Dependence Scale (SDS) is a crucial assessment tool employed by various healthcare professionals to gauge the severity of substance dependence in individuals. Its application is precious during critical junctures in a patient's journey toward recovery from substance use disorders.
Initiation of Treatment
Healthcare professionals, including addiction counselors, psychiatrists, and primary care physicians, can administer the SDS as part of the initial assessment when a patient seeks help for substance-related concerns. This aids in understanding the depth of the dependence and guiding treatment planning.
Treatment Progress Monitoring
The SDS is used intermittently during treatment. Addiction specialists and therapists use it to track dependence severity changes over time. Comparing scores between assessments informs adjustments in therapeutic interventions, ensuring alignment with the patient's progress.
After Relapse
Following a relapse, addiction counselors and therapists use the SDS to determine if dependence severity has altered. This informs discussions about triggers and challenges that may have contributed to the relapse, allowing for targeted intervention adjustments.
Transitions in Care
When patients move from inpatient to outpatient care or from one treatment phase to another, the SDS can provide insight into the ongoing treatment needs. This aids in creating continuity of care and personalized interventions.
Discharge Planning
Healthcare professionals, including social workers and case managers, employ the SDS to guide discharge planning. It assists in determining appropriate aftercare options and support services based on the patient's dependence severity and readiness for change.
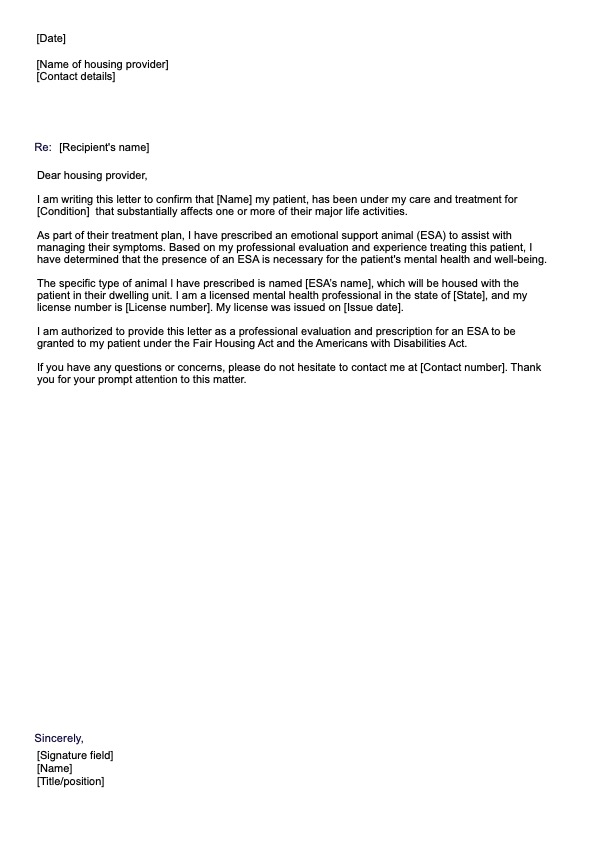
Also, utilizing a prescription template can streamline your practice and improve accuracy in medication management. This tool ensures that all necessary details are included, such as dosage, frequency, and special instructions, minimizing the risk of errors.
What are the benefits of using this Severity of Dependence Scale (SDS)?
Benefits of Using the Severity of Dependence Scale (SDS):
Objective Assessment
The free Severity of Dependence Scale (SDS) provides a standardized and structured approach to assess substance dependence. It ensures objectivity in evaluating dependence severity, reducing potential biases in clinical judgment.
Treatment Planning
Healthcare professionals can utilize the SDS to tailor treatment plans based on the assessed severity. It guides the selection of appropriate interventions, therapies, and support services, enhancing the chances of successful recovery.
Progress Tracking
Regular use of the SDS allows for tracking changes in dependence severity over time. This enables clinicians to gauge treatment efficacy, make informed adjustments, and celebrate progress.
Communication
The SDS aids in effective communication between healthcare professionals and patients. It provides a common language to discuss the impact of substance dependence and motivates patients to engage in conversations about their struggles.
Informed Decision-Making
The SDS assists clinicians in making well-informed decisions regarding the intensity and type of care needed. It helps allocate resources effectively and prioritize interventions based on the severity level.
Research and Data Collection
For researchers and healthcare organizations, the SDS offers a standardized tool to collect and analyze data on substance dependence. This contributes to a better understanding of trends, treatment outcomes, and the effectiveness of interventions.
Incorporating the free Severity of Dependence Scale (SDS) into clinical practice brings these benefits, ultimately supporting improved patient care, informed treatment planning, and a more comprehensive approach to substance dependence.
The Severity of Dependence Scale (SDS) is a well-established assessment tool that has gained recognition and support through research and clinical practice. Developed by Gossop et al. in 1995, the SDS was designed to measure the severity of dependence on various substances, providing a standardized way to assess support across different meanings. Its development was informed by the Diagnostic and Statistical Manual of Mental Disorders (DSM-III-R) criteria for substance dependence.
Research conducted between 2018 and 2021 has consistently highlighted the utility of the SDS in clinical settings. Al-Rabadi et al. (2018) examined the SDS's effectiveness in assessing opioid dependence severity and found significant correlations with other established measures, reinforcing its validity. Similarly, a study by Zhou et al. (2019) demonstrated the reliability and validity of the SDS in evaluating alcohol dependence severity among Chinese individuals seeking treatment.
Moreover, research by Turner et al. (2020) explored the SDS's role in predicting treatment outcomes. They found that higher SDS scores were associated with poorer treatment outcomes in individuals undergoing methadone maintenance treatment for opioid dependence.
The SDS's history of development, coupled with consistent empirical evidence, underscores its reliability, validity, and clinical utility. The tool's ability to provide standardized and quantifiable measures of dependence severity has contributed to its integration into addiction treatment and research. Its incorporation into clinical practice aids in accurate assessment, informed treatment planning, and improved patient outcomes, making it an invaluable resource for healthcare professionals working with individuals struggling with substance dependence.
References:
Al-Rabadi, L. J., & Akour, A. M. (2018). The Severity of Dependence Scale for assessing opioid dependence among patients with cancer pain. Pain Management Nursing, 19(2), 135-141.
Gossop, M., Darke, S., Griffiths, P., Hando, J., Powis, B., Hall, W., ... & Strang, J. (1995). The Severity of Dependence Scale (SDS): psychometric properties of the SDS in English and Australian samples of heroin, cocaine, and amphetamine users. Addiction, 90(5), 607-614.
Turner, N., De Cunto, A., & Larkin, T. A. (2020). Predicting opioid treatment outcomes using the Severity of Dependence Scale: a prospective cohort study. Substance Abuse, 1-6.
Zhou, Y., Liang, X., Dai, Z., He, X., Lao, G., & Fan, X. (2019). The Severity of Dependence Scale predicts the retention of methadone maintenance treatment: An observational study. Medicine, 98(16), e15204.
Commonly asked questions
The worksheet aims to increase awareness of how avoidance patterns contribute to emotional suffering and hinder personal growth. By documenting avoidance-related experiences, you can better understand your behavior and work toward embracing challenges instead of avoiding them.
The Avoidance and Suffering Diary benefits anyone looking to enhance their emotional well-being and practice mindfulness. It's beneficial for individuals struggling with avoidance behaviors, anxiety, and depression or those seeking to improve their psychological flexibility.
You can use this worksheet whenever you notice avoidance tendencies or feel a sense of emotional distress. Consistent practice can lead to better self-awareness, increased emotional regulation, and a more remarkable ability to face challenging situations.
While the worksheet can be a valuable tool for self-exploration, it is not a substitute for professional therapy. If you're dealing with severe emotional difficulties, it's recommended to consult a qualified therapist for personalized support.












-template.jpg)