Post-Traumatic Stress Diagnostic Scale
Looking for an effective way to assess and identify PTSD? Utilize our post-traumatic stress diagnostic scale.


What is the Post-Traumatic Stress Diagnostic Scale (PDS)?
Post-traumatic stress disorder (PTSD) is a disorder that manifests following a traumatic or shocking event, such as a natural disaster, where an individual develops frequent, fearful reactions to different events or stimuli. Although fear or stress are common reactions to and following a traumatic event, most individuals tend to overcome these symptoms relatively quickly. When an individual experiences severe fear or distress symptoms persistently, they may be experiencing PTSD symptoms.
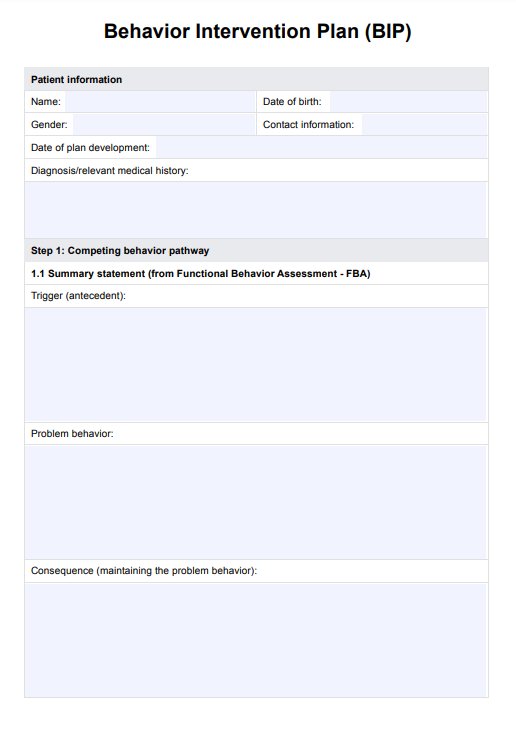
PTSD can develop in any individual during or following a traumatic event, and may even occur after witnessing or hearing of a traumatic event that occurred to someone else (NIMH, n.d.). These symptoms typically manifest within three months following the event, and PTSD is diagnosed in accordance with the following criteria:
- The symptoms must be persistent for longer than one month
- Symptoms must be severe enough to impact life functions
- Symptoms must not be linked to any medications, illness, or substance use.
Adult patients must have a:
- Minimum of one re-experiencing symptom (such as flashbacks or recurring dreams)
- Minimum of one avoidance symptom (such as avoiding thoughts or feelings)
- Minimum of two arousal/reactivity symptoms (such as tenseness or irritability)
- Minimum of two cognition and mood symptoms (such as difficulty recalling key memories or loss of interest).
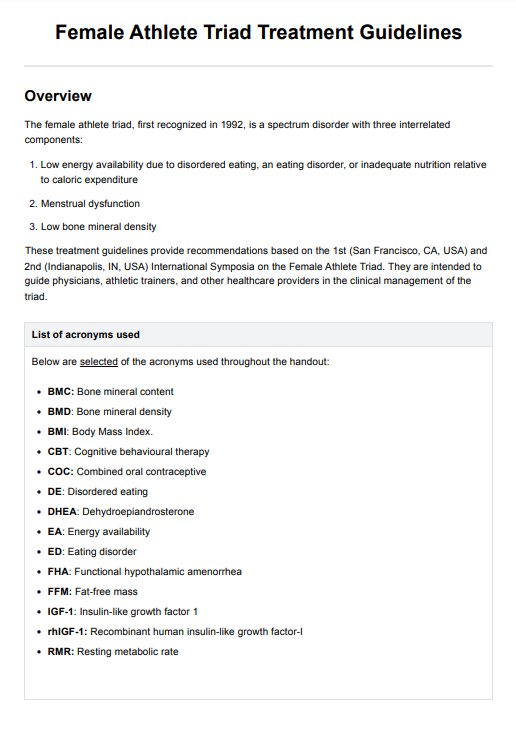
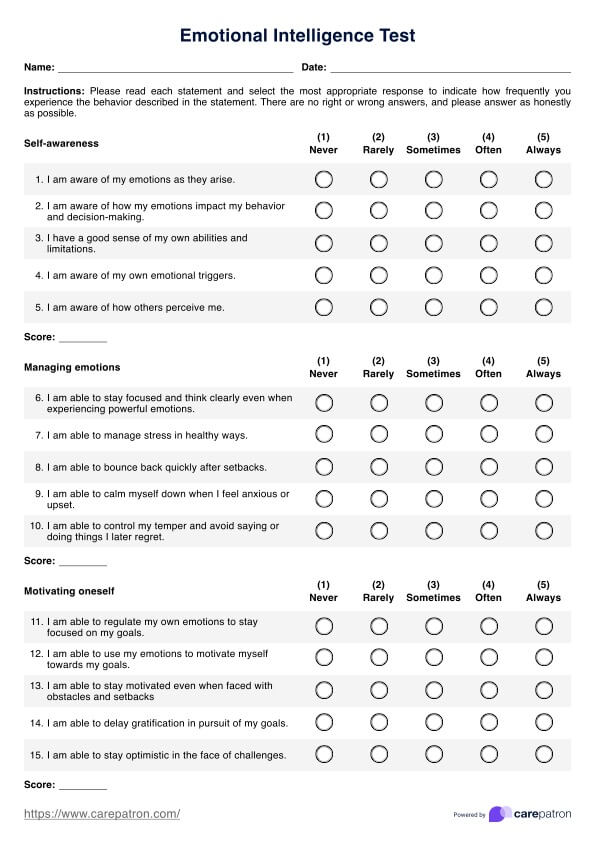
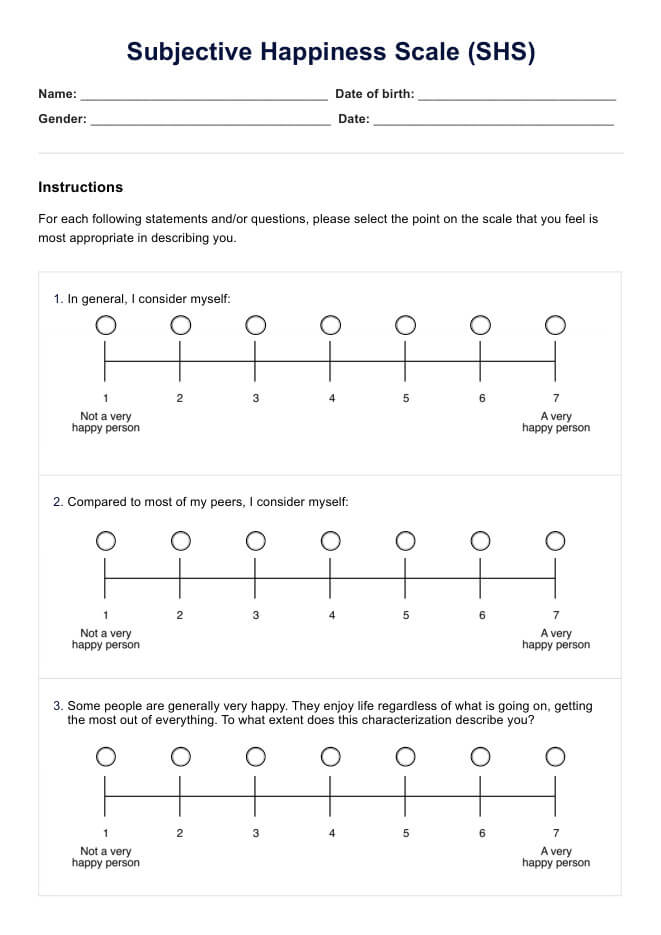
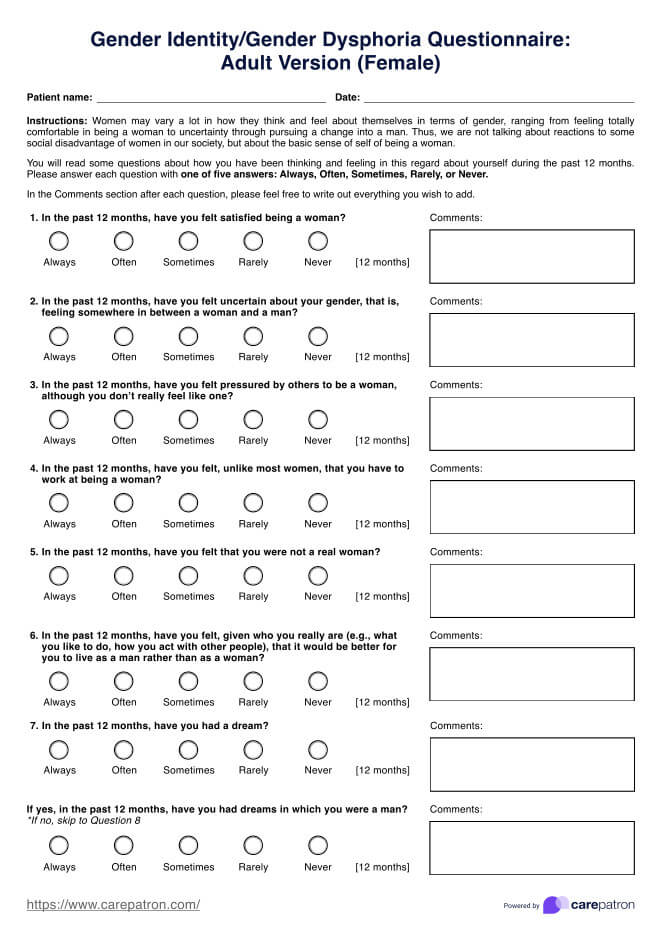
The post-traumatic stress diagnostic scale (PDS) was developed as a self-reporting psychological assessment of PTSD symptom severity. The items included in the scale reflect the DSM IV criteria, and provides a series of questions related to the occurrence of distress or intrusive thinking, hyperarousal, or avoidance behaviours (McCarthy, 2008).
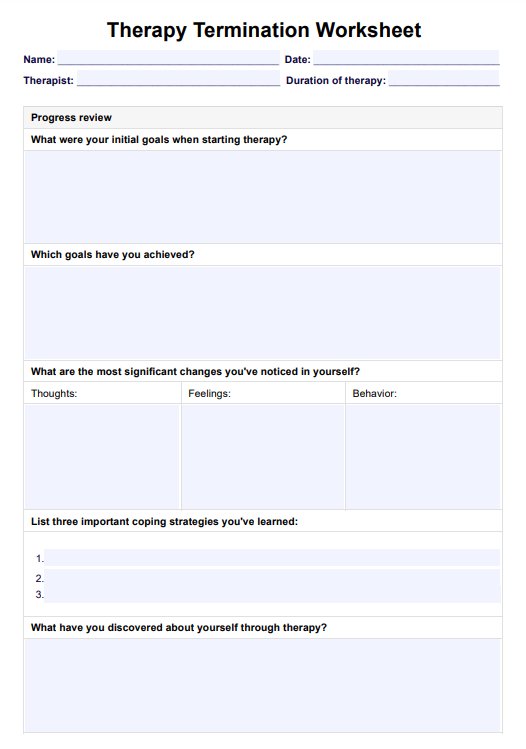
Post-Traumatic Stress Diagnostic Scale Template
Post-Traumatic Stress Diagnostic Scale Example
Signs and symptoms of PTSD
Signs and symptoms of PTSD encompass a range of re-experiencing, avoidance, arousal, reactive, cognitive, and mood-related behaviors that reflect the impact of a traumatic event on an individual's well-being. These typically include having difficulty falling asleep, keeping away from places that serve as reminders, and feeling isolated from the world.
Identifying these symptoms is essential for both the individual, those around them, and mental health practitioners, as they can be early indicators of psychological trauma. By being able to sense these, individuals can seek support and guidance from registered psychologists or counselors to receive a psychological assessment and interventions.
Completing diagnostic procedures such as a PTSD checklist or standardized self-report measures can provide a severity score, or assess symptom severity to gain more insight of the degree of PTSD. In knowing this information, the health professional can provide personalized treatment and support to the individual to reduce the individual's subjective distress, and enhance their well-being.
What does the Post-Traumatic Stress Diagnostic Scale (PDS) assess?
The PDS is most typically used as a self-report measure for PTSD, that seeks to screen for the presence and severity of symptoms following a traumatic event. It covers a range of symptoms related to PTSD, generating a subscale score for each type of symptom, as well as an overall symptom severity score to indicate the level of PTSD.
Given that PTSD can manifest in many ways and present many different symptoms, assessing psychological trauma can be different. The PDS can help mental health practitioners assess symptom severity, and can serve as a document for further psychological assessments, such as a trauma test. In doing so, it can be a form of early detection which is essential for effective treatment and wellbeing of individuals experiencing PTSD.
Why use the PDS?
As a self-report psychological assessment, the PDS is a clinically significant way to assess PTSD. Though it is primarily used in assessment, the following are some scenarios and reasons for using the PDS, which may highlight the relevance of this resource in clinical practice:
Early detection of PTSD
Given that PTSD can manifest in many different ways and can be expressed through several different behaviors, it can be difficult to diagnose. The PDS provides a checklist for symptoms and behaviors that may be indicative of PTSD symptoms, which can be used as an initial basis for further psychological assessment. This may allow for the early detection of PTSD, which is essential for effective trauma treatment plans.
Clinically significant
The post-traumatic stress diagnostic scale (PDS) was developed as a self-report measure for post-traumatic stress disorder (PTSD), established by renowned clinical psychologist, Professor Edna Foa (McCarthy, 2008). Designed for practical use in clinical and research environments, the scale functions to investigate the presence or severity of PTSD in patients who have self-identified or have had a history of the disorder following a traumatic event.
Self-report
Mental health conditions like PTSD are often difficult to diagnose, as unlike any other serious injury, it is often not as easily observed physically. As a self-report measure, the PDS provides an opportunity for individuals to express their internal distressing and intrusive thoughts, allowing practitioners a glimpse into their inner dialogue. This is essential for the diagnosis of PTSD, and can help inform trauma therapy techniques.
Further testing
The PDS can be a provisional PTSD diagnosis, and can serve as a catalyst for further psychological assessment. Completing further testing in accordance with the PDS may also identify other mental disorders.
References
McCarthy, S. (2008). Post-Traumatic Stress Diagnostic Scale (PDS). Occupational Medicine, 58(5), 379. DOI: https://doi.org/10.1093/occmed/kqn062
NIMH (n.d.). Post-Traumatic Stress Disorder. National Institute of Mental Health. https://www.nimh.nih.gov/health/topics/post-traumatic-stress-disorder-ptsd#:~:text=Post%2Dtraumatic%20stress%20disorder%20(PTSD)%20is%20a%20disorder%20that,or%20respond%20to%20potential%20danger.
Commonly asked questions
The post-traumatic stress diagnostic scale (PDS) is a self-report measure that helps identify the presence and severity of post-traumatic stress disorder (PTSD).
Post-traumatic stress disorder or PTSD, is a condition where an individual experiences frequent bouts of distressing and intrusive thoughts following a traumatic event. Though PTSD can occur for a variety of reasons, it may typically manifest following a particularly traumatic event like a natural disaster, or after hearing of a traumatic event within someone else's life.
Although many symptoms may indicate PTSD, the most common include the following:
- Arousal and reactivity symptoms, like irritability or tenseness
- Avoidance symptoms, like avoiding thoughts or feelings
- Cognition and mood symptoms, like poor memory or loss of interest
- Re-experiencing symptoms, like dreams or flashbacks


.jpg)
-sample.jpg)












-template.jpg)