Cold Agglutinin
Learn about the Cold Agglutinin Test for diagnosing autoimmune conditions. Understand its role in healthcare alongside Cold Caloric Test.


What is a Cold Agglutinin Test?
A Cold Agglutinin Test is a diagnostic laboratory test used in healthcare to detect the presence of cold agglutinins in a person's blood. Cold agglutinins are a type of antibody produced by the immune system that can cause red blood cells to clump together (agglutinate) when exposed to cold temperatures, typically below normal body temperature. This phenomenon is known as cold agglutinin disease (CAD) or cold autoimmune hemolytic anemia.
The test is primarily ordered when a healthcare provider suspects a patient may have CAD or related conditions, as it helps confirm the diagnosis. CAD is often associated with underlying medical conditions such as infections, autoimmune disorders, or lymphoproliferative disorders. Cold agglutinins can lead to symptoms like anemia, fatigue, pale skin, and circulation problems, especially in extremities exposed to cold.
The Cold Agglutinin Test involves drawing a blood sample from the patient, which is then sent to a laboratory for analysis. In the lab, the blood is exposed to varying temperatures, including cold conditions, to observe how the red blood cells react. If the red blood cells clump together when exposed to cold, it indicates the presence of cold agglutinins.
Once diagnosed, CAD and related conditions can be managed through various treatment options, including addressing the underlying cause (if present), keeping the body warm in cold environments, and, in some cases, medication or blood transfusions.
The Cold Agglutinin Test is an essential tool in diagnosing conditions related to cold agglutinins in the blood, helping healthcare providers identify and manage underlying health issues affecting the patient's well-being. It plays a crucial role in tailoring appropriate treatment plans and improving the quality of life for individuals with CAD and related conditions.
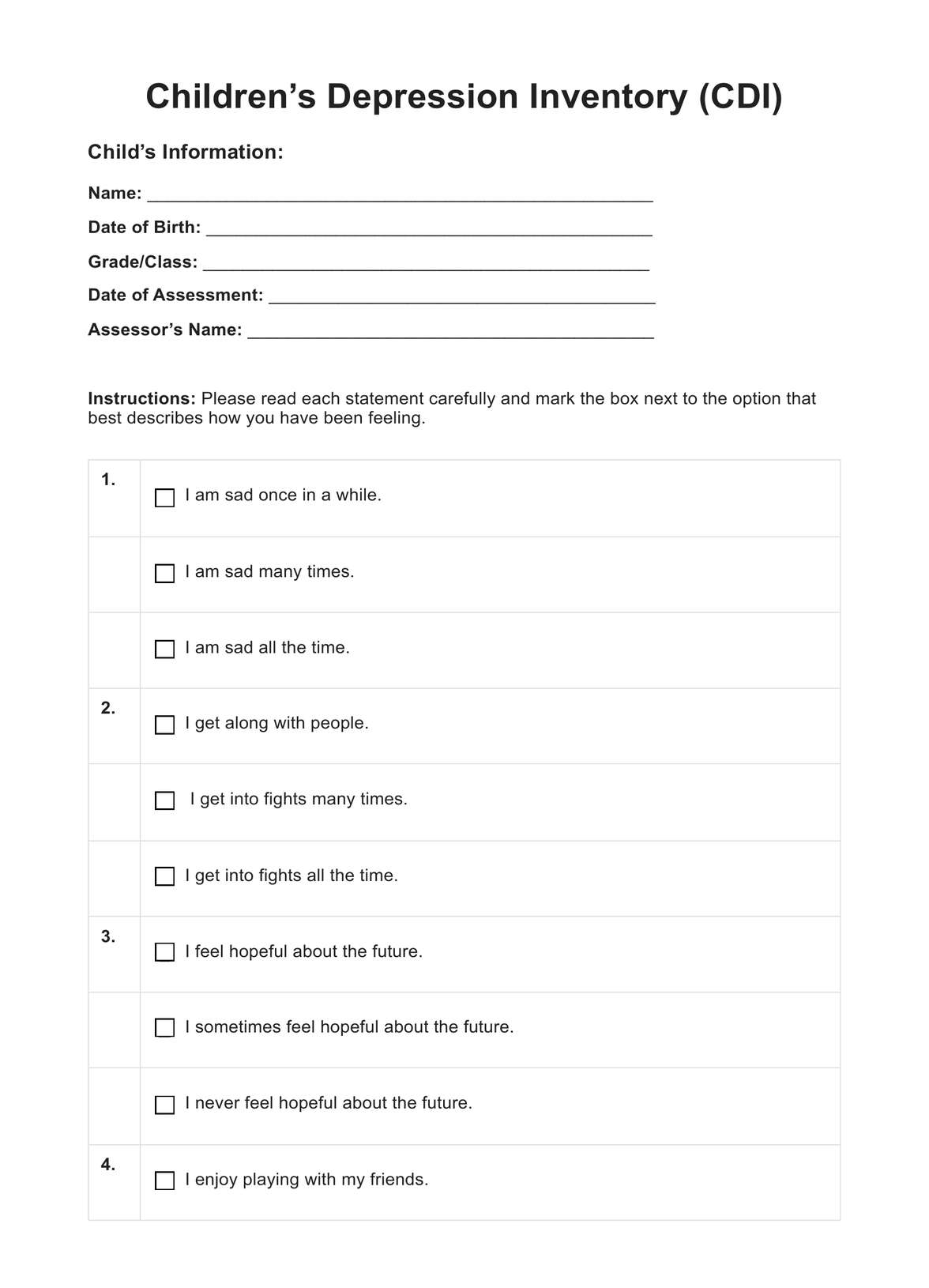
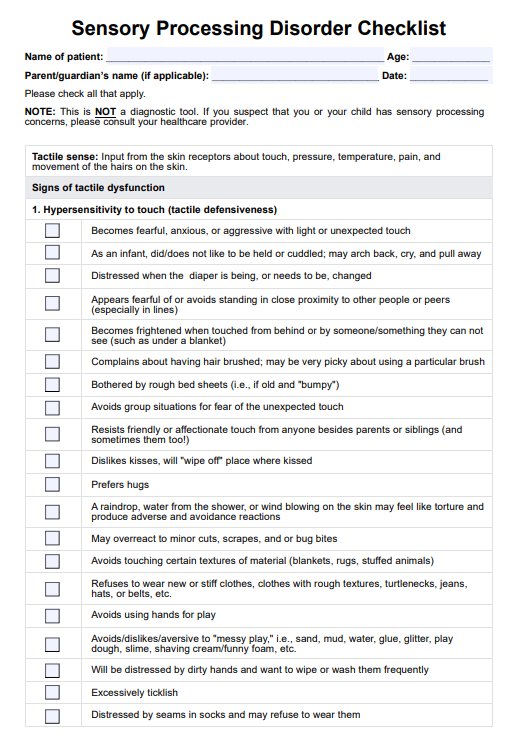
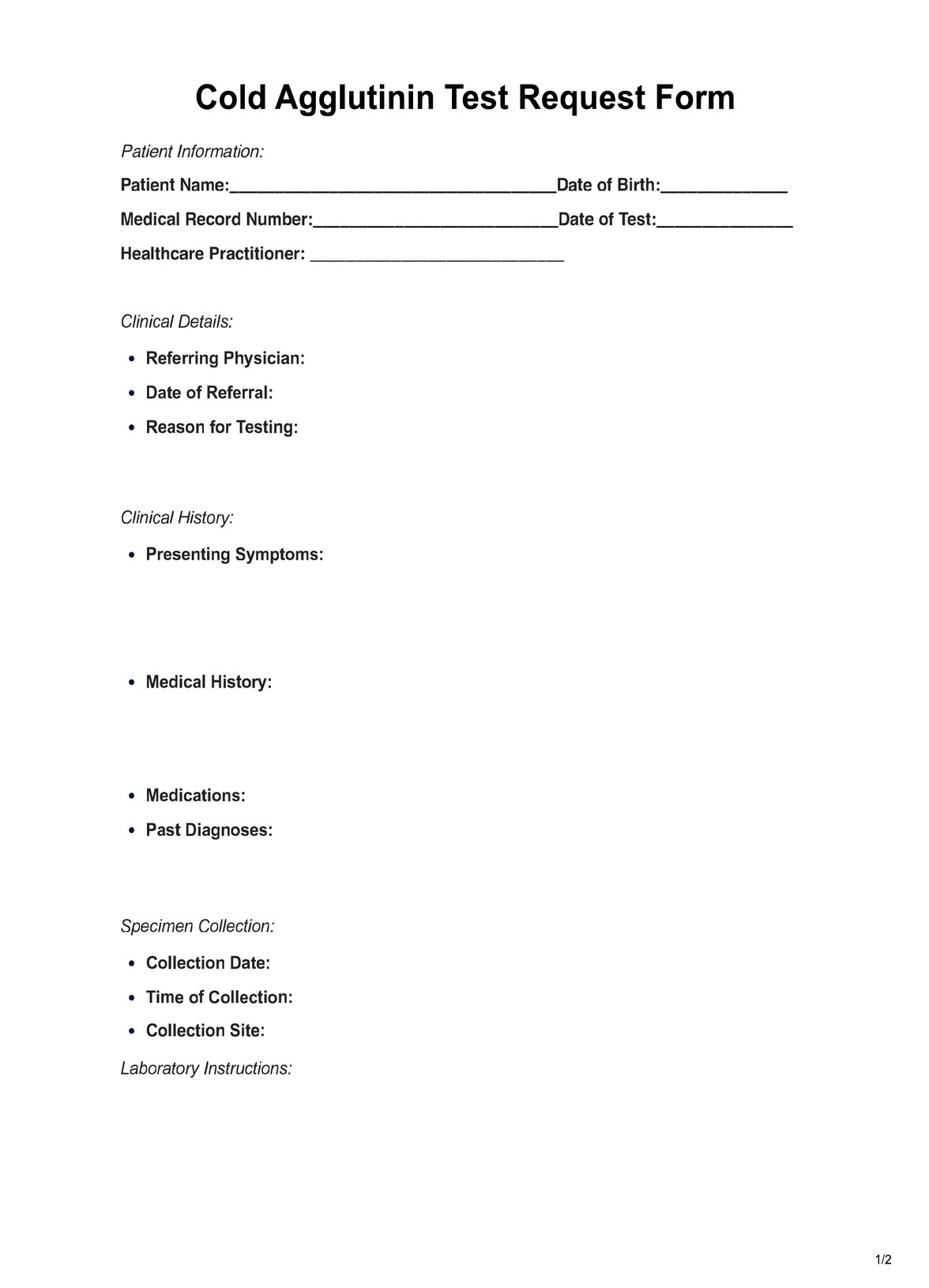
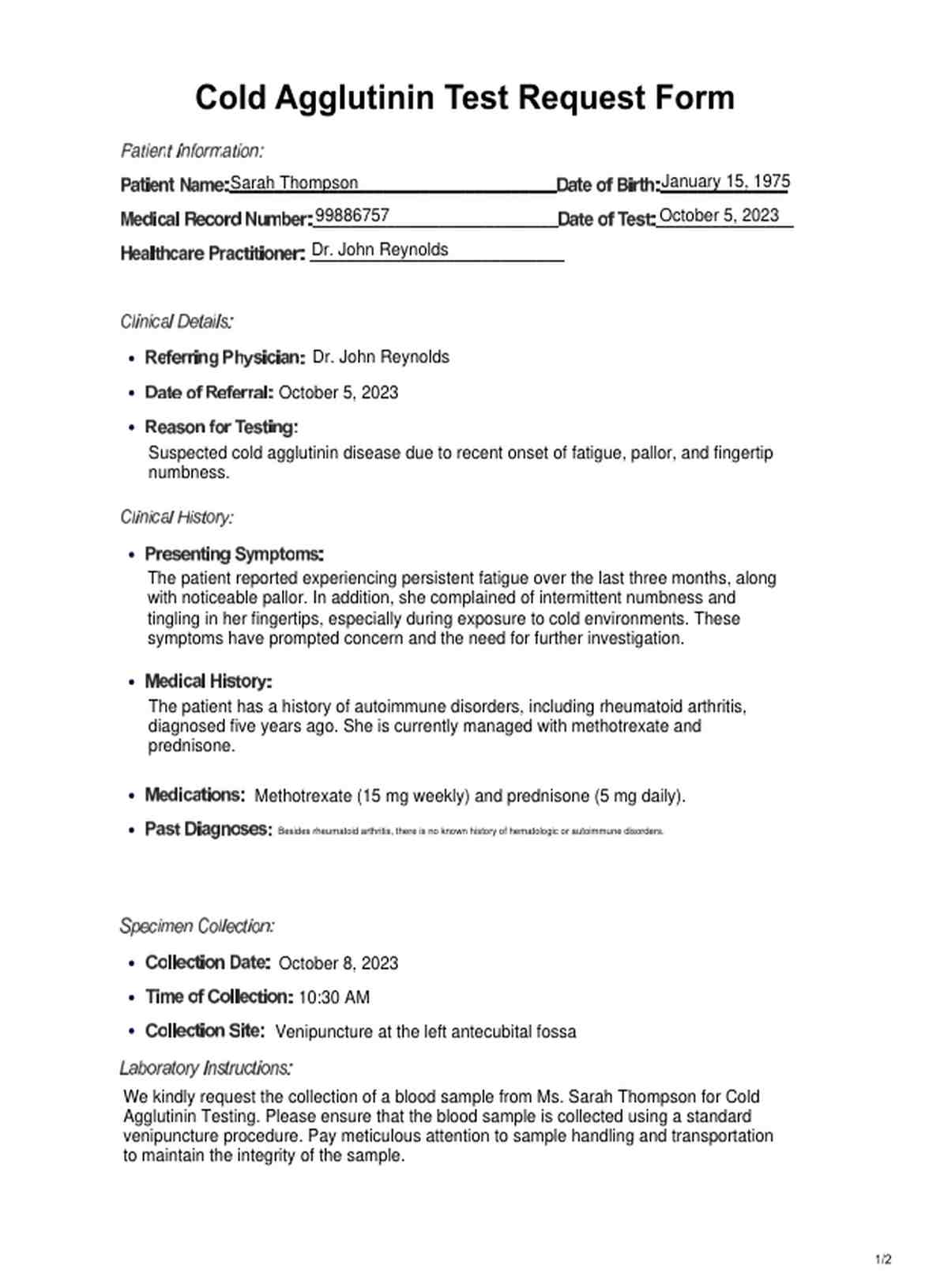
Cold Agglutinin Template
Cold Agglutinin Example
How does it work?
Using and filling out the Cold Agglutinin Test Request Form is essential for healthcare practitioners to ensure accurate diagnostic testing for patients suspected of having cold agglutinin-related conditions. Here are the steps involved in using and completing this crucial form:
Obtaining the Form
Begin by obtaining a printable Cold Agglutinin Test Request Form, either in a digital format or as a physical paper document, from your healthcare facility or laboratory.
Patient Information
Fill in the patient's details on the form, including their name, date of birth, gender, and contact information. If applicable, provide the patient's medical record number for easy reference.
Clinical Details
Include information about the referring physician, the date of referral, and the reason for testing. In this case, keywords like "Cold Agglutinin Test" and "suspected cold agglutinin disease" should provide a clear clinical context.
Clinical History
Record the patient's presenting symptoms, medical history, current medications, and past diagnoses. This section is critical for understanding the patient's health and potential risk factors.
Specimen Collection
Indicate the date and time of blood sample collection. Specify the collection site, typically through venipuncture at a specific location, such as the left antecubital fossa.
Laboratory Instructions
Clearly state that a blood sample is being requested for Cold agglutinin testing. Emphasize the importance of proper sample handling and transportation to maintain sample integrity.
Special Considerations
Provide any additional clinical information that may aid in interpreting test results. Mention if the patient has a history of cold agglutinin-related conditions or if symptoms worsen in cold environments.
Provider's Name and Signature
The referring physician should sign and date the form to validate the request.
Attach Relevant Records
If applicable, attach any relevant medical records or additional information that could assist in interpreting the Cold Agglutinin Test results.
Inform the Patient
Ensure that the patient is informed about the purpose and potential implications of the test. Address any questions or concerns they may have.
By following these steps and accurately filling out the Cold Agglutinin Test Request Form, healthcare practitioners can facilitate the diagnostic process and effectively manage patients with suspected cold agglutinin-related conditions, ultimately improving patient care and outcomes.
When would you use this test?
The Cold Agglutinin Test is a crucial diagnostic tool employed by healthcare practitioners in various specialties to investigate and confirm the presence of cold agglutinins in a patient's blood. It is used in several clinical scenarios:
Hematologists and Immunologists
Hematologists and immunologists frequently employ the Cold Agglutinin Test when patients present with symptoms such as anemia, fatigue, and pale skin. These symptoms can indicate underlying cold agglutinin disease (CAD) or other autoimmune hemolytic anemias. The test helps identify the specific autoimmune mechanism causing hemolysis.
Rheumatologists
Rheumatologists utilize this test when managing patients with autoimmune disorders, as autoimmune conditions like rheumatoid arthritis can be associated with cold agglutinins. Monitoring cold agglutinin levels can aid in disease management and treatment decisions.
Primary Care Physicians
Primary care physicians may use the Cold Agglutinin Test when patients report symptoms exacerbated by cold exposure, such as numbness, tingling, or color changes in extremities. This can help diagnose cold-induced autoimmune reactions or underlying conditions.
Infectious Disease Specialists
In some cases, infections like Mycoplasma pneumoniae can trigger the production of cold agglutinins. Infectious disease specialists may request this test to investigate the presence of these antibodies as part of their diagnostic workup.
Transfusion Medicine Specialists
Before transfusing blood to a patient, particularly in emergencies, transfusion medicine specialists may request the Cold Agglutinin Test to ensure compatibility and prevent adverse reactions to cold agglutinins in the recipient's blood.
Clinical Pathologists and Laboratory Technologists
These professionals perform the Cold Agglutinin Test in clinical laboratories. They play a pivotal role in accurately processing and interpreting the test results, aiding in diagnosing and managing cold agglutin-related disorders.
What do the results mean?
The results of a Cold Agglutinin Test provide valuable information about the presence and activity of cold agglutinins in a patient's blood. Here's a breakdown of common results and their meanings:
Negative Result:
- Normal: A negative result indicates the absence of cold agglutinins in the patient's blood. This is typically considered normal, suggesting no evidence of cold agglutinin disease (CAD) or related autoimmune hemolytic anemias.
Positive Result:
- Positive with Symptoms: A positive result with concurrent clinical symptoms like anemia, fatigue, and circulation problems may indicate the presence of active cold agglutinins. This can be indicative of CAD or another cold-antibody-related condition.
- Positive without Symptoms: A positive result may occur without apparent clinical symptoms. In such cases, it's crucial to evaluate the patient's medical history and perform additional tests to determine if treatment or further monitoring is necessary.
Titers and Temperature Sensitivity:
- High Titers: High cold agglutinin titers indicate a significant presence of these antibodies in the blood. Higher titers are often associated with more severe symptoms and may require more aggressive management.
- Temperature Sensitivity: The test may also report the temperature at which agglutination (clumping of red blood cells) occurs. Lower temperature sensitivity indicates that agglutination happens at a higher temperature, which may correlate with milder symptoms.
Underlying Conditions:
- Associated Conditions: A positive result may lead to further investigations to identify underlying conditions that trigger cold agglutinin production. These conditions can include infections (e.g., Mycoplasma pneumoniae), autoimmune diseases (e.g., rheumatoid arthritis), or lymphoproliferative disorders.
- Management and Treatment: The results guide healthcare practitioners in determining the appropriate management and treatment options, such as avoiding cold exposure, addressing underlying conditions, and, in severe cases, considering medications or blood transfusions.
Interpreting Cold Agglutinin Test results in conjunction with the patient's clinical presentation, medical history, and other relevant diagnostic tests is essential. Additionally, follow-up testing and monitoring may be necessary to assess the progression of cold agglutinin-related conditions. Ultimately, the results are critical in tailoring a patient's treatment plan to alleviate symptoms and improve their health and well-being.
Research & Evidence
The Cold Agglutinin Test, an essential diagnostic tool in hematology and immunology, has a history rooted in the understanding of autoimmune hemolytic anemias and cold agglutinin disease (CAD).
Research during this period has focused on refining the diagnostic accuracy and understanding the clinical significance of cold agglutinins. A study by Berentsen and Tjønnfjord (2018) highlighted advancements in understanding CAD's pathophysiology, emphasizing the immune system's role in the development of cold agglutinins and their impact on red blood cell destruction.
Further studies, such as by Sharma et al. (2019), delved into the association of cold agglutinins with specific infections, especially Mycoplasma pneumoniae. The research explored the prevalence of cold agglutinins in such cases and its implications for diagnosis and treatment.
In terms of diagnostic accuracy, a study by Michel et al. (2020) investigated the use of automated hematology analyzers in detecting cold agglutinins, aiming to improve efficiency and reduce manual errors. This research provided valuable insights into leveraging technology for better diagnostic outcomes.
Recent studies have also explored treatment strategies. A study by Patel et al. (2021) discussed therapeutic approaches for managing CAD and related disorders, including using rituximab and complement inhibitors. This research highlighted evolving treatment options that could potentially improve patient outcomes.
References
Berentsen, S., & Tjønnfjord, G. E. (2018). Diagnosis and treatment of cold agglutinin mediated autoimmune hemolytic anemia. Blood Reviews, 32(2), 93-100. doi:10.1016/j.blre.2017.10.002
Michel, M., Bird, R. G., & Talbot, D. (2020). Diagnostic use of automated hematology analyzers to detect cold agglutinins. The Journal of Applied Laboratory Medicine, 5(3), 615-619. doi:10.1093/jalm/jfaa023
Patel, D. S., Spivak, J., & Cserti-Gazdewich, C. (2021). Cold agglutinin disease: an underrecognized cause of autoimmune hemolytic anemia. Transfusion Medicine Reviews, 35(1), 62-70. doi:10.1016/j.tmrv.2020.03.003
Sharma, S., Bhargava, M., Agrawal, A., & Sharma, A. (2019). Cold agglutinins in patients with Mycoplasma pneumoniae infection: How cold is cold? Journal of Laboratory Physicians, 11(2), 146-149. doi:10.4103/JLP.JLP_7_19
Commonly asked questions
Cold agglutinins can be associated with autoimmune disorders (e.g., rheumatoid arthritis), infections (e.g., Mycoplasma pneumoniae), or lymphoproliferative disorders.
The test is generally safe, but like any blood draw, there may be minor risks such as bruising or infection at the collection site. These risks are minimal and rare.
Treatment depends on the underlying cause and severity of symptoms. It may include avoiding cold exposure, addressing the underlying condition, and, in severe cases, medications or blood transfusions.




















-template.jpg)