While some nondisplaced fractures might heal with proper immobilization, untreated or improperly treated scaphoid fractures can lead to nonunion or avascular necrosis, necessitating more complex treatments.
Scaphoid Fracture Test
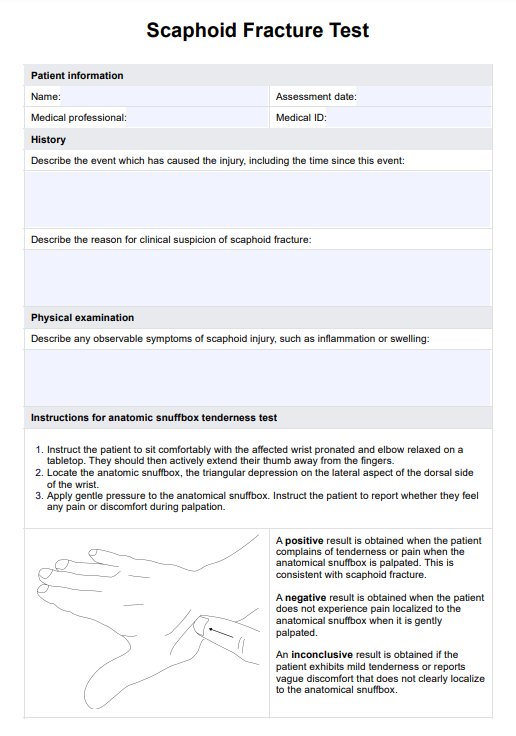
Access our free Scaphoid Fracture Test for thorough and accurate physical examination in cases of suspected scaphoid fracture.
Scaphoid Fracture Test Template
Commonly asked questions
Healing times vary depending on the fracture's location and whether it is displaced. Nondisplaced fractures may heal within 6 to 12 weeks with proper immobilization, whereas displaced fractures or those requiring surgery might take longer.
Nondisplaced fractures, or those caught early, can often be treated conservatively, i.e. with casting. However, surgery may be recommended for displaced fractures, nonunions, or when the fractured scaphoid exhibits instability after extended immobilization.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











