An RTA is performed promptly after an injury, typically at the scene of the accident, soon after emergency medical professionals arrive, or immediately on arrival at an emergency department.
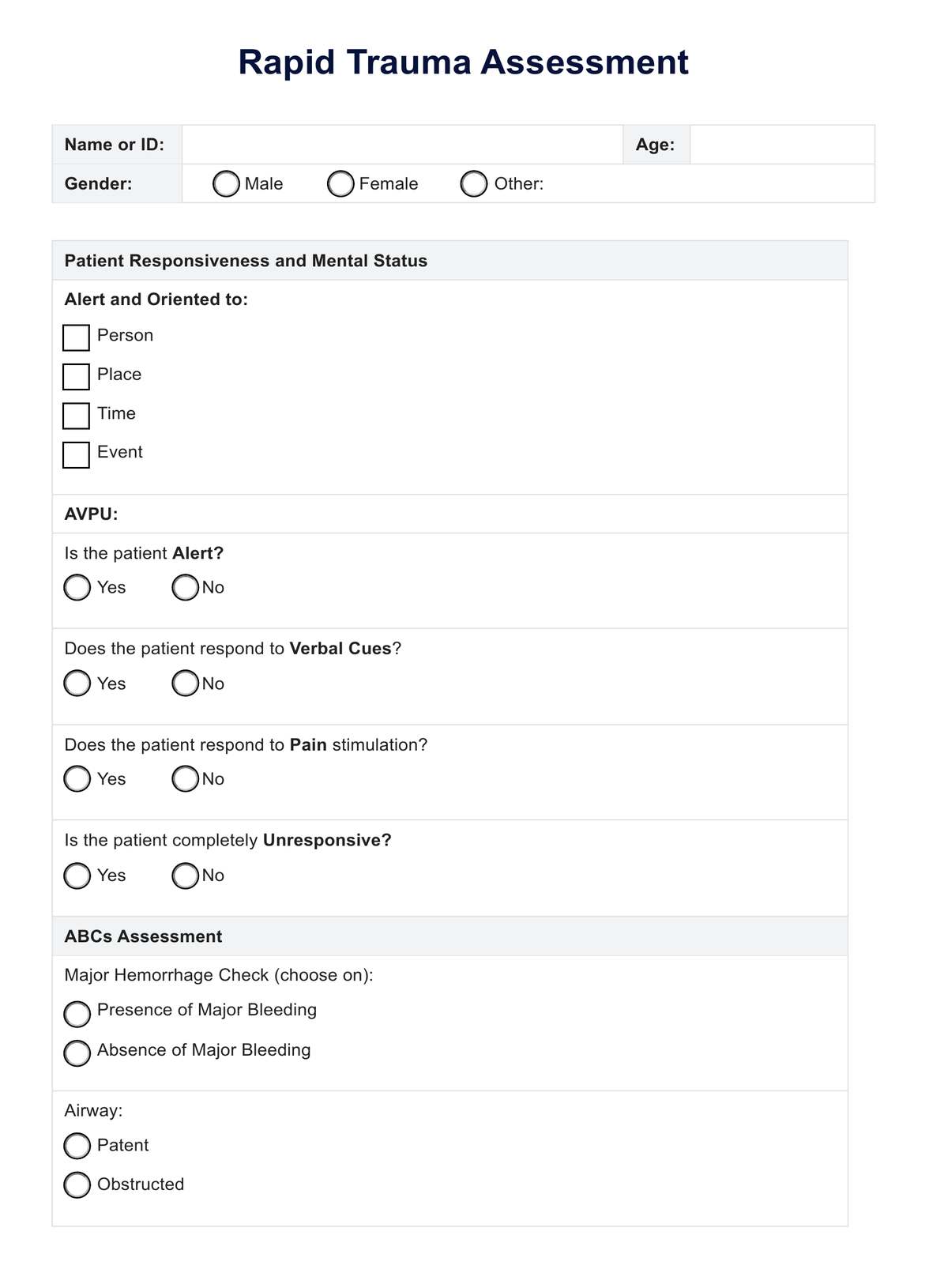
Rapid Trauma Assessment
Learn more about physical trauma and how this can be effectively assessed among patients through the Rapid Trauma Assessment. Download a free PDF resource here.
Use Template
Rapid Trauma Assessment Template
Commonly asked questions
RTA is usually performed by trained healthcare professionals such as par
Rapid recognition allows immediate treatment of life-threatening conditions, minimizing the consequences of the injury and improving the likelihood of a better patient outcome.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











