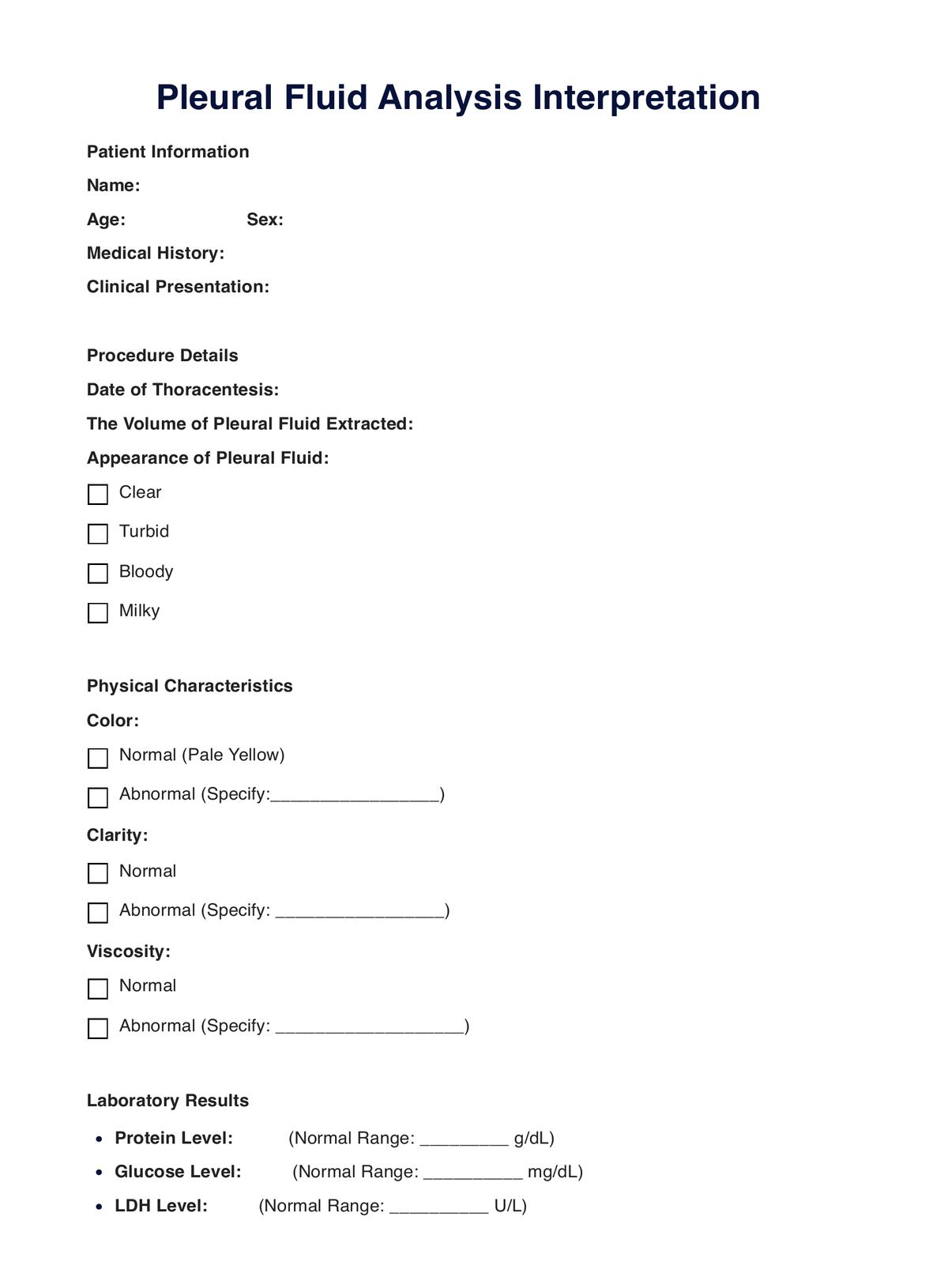
Pleural Fluid Analyses are crucial for diagnosing the underlying causes of pleural effusion and guiding targeted treatment plans for conditions like infections, inflammation, and malignancies.
Pleural Fluid Analysis
Unlock diagnostic insights with pleural fluid analysis. Comprehensive and timely results for effective management of respiratory conditions.
Use Template
Pleural Fluid Analysis Template
Commonly asked questions
The results typically take a few days, but urgency may expedite the process. Timely communication is maintained to address patient needs.
Minimal preparation is required. Patients may be asked to refrain from eating or drinking for a few hours before the procedure. Informing the healthcare provider about medications is essential.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











