Risk factors for PDD include a family history of depressive disorders, experiencing traumatic life events, having other mental health conditions like anxiety disorders or substance abuse, and psychological factors like negative affectivity. Early childhood adversity and low socioeconomic status are also potential risk factors.
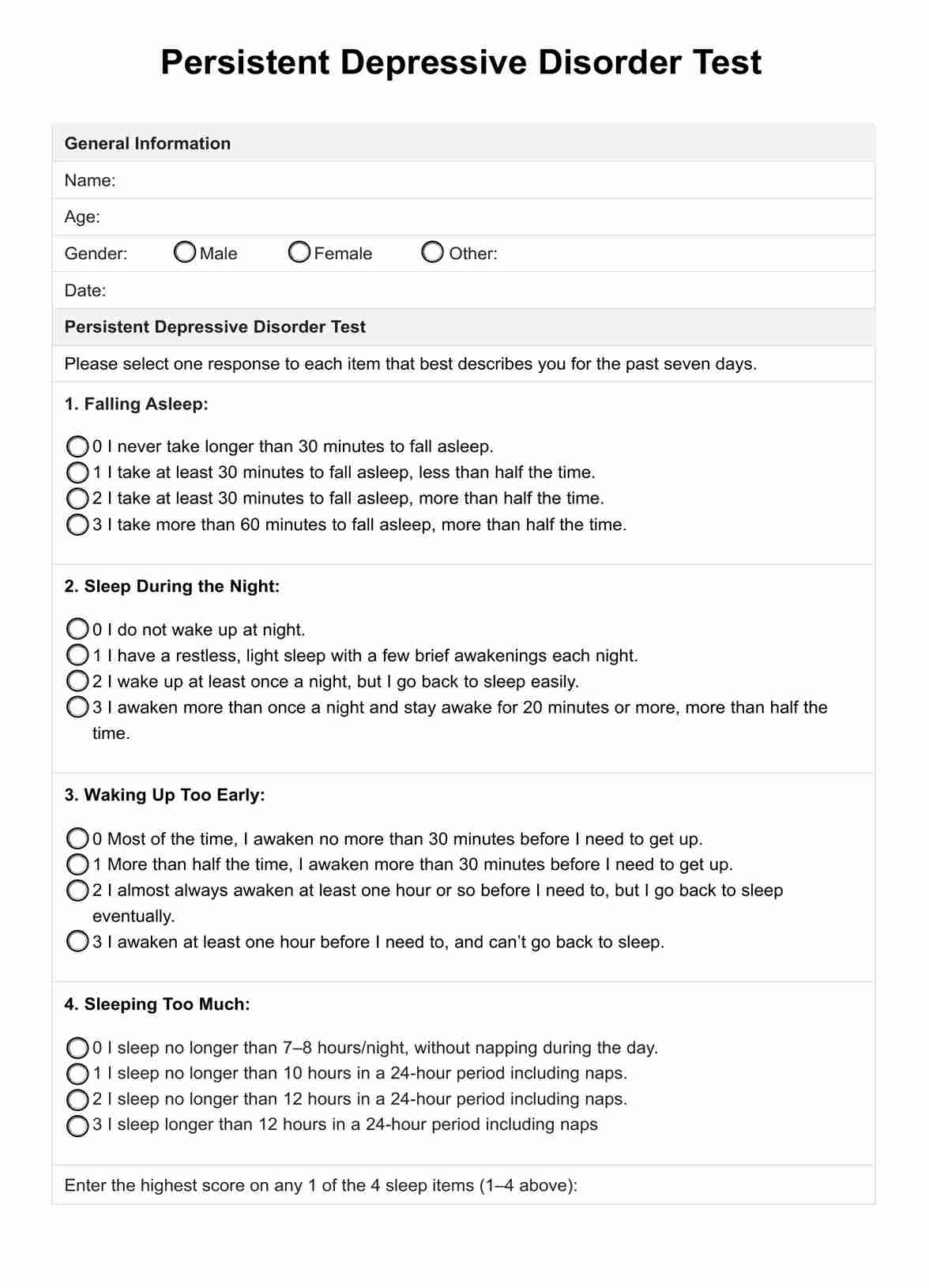
Persistent Depressive Disorder Test
Explore an evidence-based screening tool to help diagnose persistent depressive disorder among clients.
Persistent Depressive Disorder Test Template
Commonly asked questions
PDD is a chronic, long-lasting depressive condition. By definition, individuals must experience a depressed mood most days for at least two years in adults or one year in children/adolescents to meet the diagnostic criteria. For many, PDD can potentially last for several years without adequate treatment.
If dysthymia is left untreated, it can significantly impair one's quality of life and ability to function in daily activities. Untreated PDD increases the risk of developing other mental health issues like anxiety disorders or substance abuse problems. It can strain personal relationships, negatively impact work/school performance, and lead to social isolation.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











