What is a PASS Assessment?
The Postural Assessment Scale for Stroke Patients (PASS) is a specialized tool designed to assess and measure postural control among stroke patients. This performance assessment is designed to identify the specific postural control impairments that may be affecting a patient's functional abilities, such as their ability to sit, stand, or walk.
Developed by Benaim and colleagues (1999), the PASS was specifically created to evaluate patients post-stroke. Its independence and safety scales allow therapists and clinicians to identify specific postural deficits that may be affecting their progress toward rehabilitation goals. Importantly, PASS has been validated through rigorous testing, demonstrating both high reliability and good content validity. This means the assessments accurately reflect the construct of postural control it aims to measure.
In addition to its use in clinical settings, the PASS assessment has also been used in research settings to investigate the effects of various interventions on postural control in stroke patients. For example, studies have used the PASS assessment to evaluate the effectiveness of balance training programs, gait training programs, and robotic-assisted therapy in improving postural control in stroke patients (Wu et al., 2021).
What can you expect from this test?
In practice, the PASS can be a valuable component of a patient’s rehabilitation evaluation and ongoing monitoring. It enables practitioners to:
- Quantify levels of functional independence that impact self-care skills
- Formulate targeted rehabilitation strategies
- Determine the amount of assistance needed in daily life tasks
- Monitor patient progression over time
- Enhance communication between health professionals through a shared metric
- Inform patients and their families about current abilities in a concrete manner
The administration of the PASS assessment is straightforward and can be completed in approximately 15-20 minutes. It is a valuable tool for monitoring a patient's progress over time, as it can be used to track changes in postural control and balance throughout the rehabilitation process.
One of the PASS's key strengths is the physical emphasis on posture, a crucial aspect of mobility and function often affected by stroke. The PASS produces quantifiable data, which allows practitioners to have a detailed picture of a patient's occupational performance.
However, like all assessments, the PASS must be used as part of a comprehensive evaluation. While highly effective for evaluating postural control and task independence, it does not replace assessments for other impairments that might accompany stroke, such as tests with cognitive emphasis or those that address sensory deficits.
How are results interpreted?
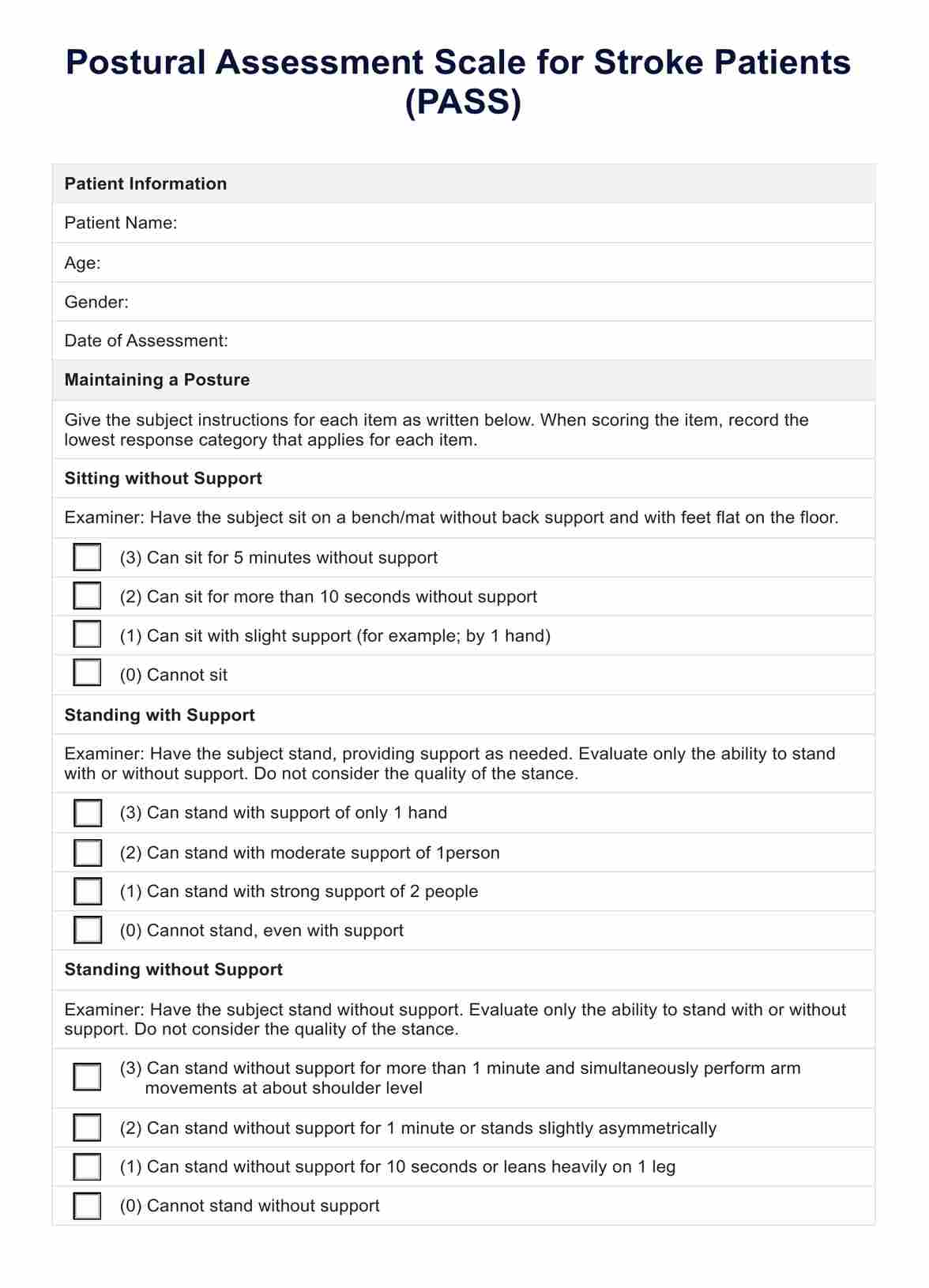
The PASS consists of a total of 12 items, each evaluated on a scale from 0 to 3. The scoring is detailed as follows:
- 0 points indicate the patient is unable to perform the task.
- 1 point shows the patient can perform the task with major assistance.
- 2 points are given when the patient can perform the task with minimal assistance.
- 3 points reflect complete independence in performing the task, with no assistance required.
The cumulative score can range from 0, indicative of total dependence, to 36, which suggests full independence in postural tasks.
- 0-12 points: Typically indicates severe impairment in postural control. Patients with scores in this range may require substantial assistance for basic postural adjustments and are likely to be highly dependent.
- 13-24 points: Suggests moderate impairment. Patients within this score range have some ability to control posture but still need assistance to maintain or change positions safely.
- 25-36 points: Reflects mild impairment or near independence. Patients scoring in this range can perform most postural tasks and physical self-maintenance with little to no assistance, although some minor difficulties might persist.
When interpreting the PASS results, healthcare practitioners should also consider the following:
- Total PASS score: The total PASS score provides an overall measure of the patient's postural control and balance. A higher score indicates better performance, while a lower score suggests more significant deficits that may require more intensive rehabilitation interventions.
- Individual item scores: Examining the scores for each individual item can help identify specific areas of strength and weakness among only those tasks. This information can guide the development of targeted interventions to address deficits in tasks deemed relevant to their functioning.
- Changes over time: Regularly administering the PASS assessment throughout the rehabilitation process can help track the patient's progress. Observing changes in the total PASS score and individual item scores over time can provide valuable insights into the effectiveness of the rehabilitation interventions and guide adjustments as needed.
- Comparison to normative data: Healthcare practitioners can compare the patient's PASS scores to normative data, which can provide a frame of reference for interpreting the patient's performance and identifying areas that require more intensive rehabilitation efforts.
It is also important to note that the PASS assessment is just one tool in the evaluation of postural control and balance abilities in stroke patients. Healthcare practitioners should use a comprehensive approach that includes a thorough physical examination and medical history. They can also use PASS alongside other assessments, such as an instrumental self-maintenance scale, a functional assessment questionnaire, and a performance assessment of self for a self-report of the patient's needs, capacity, and goals.