Nursing brain sheets enhance patient care by offering a structured layout where nurses can track important medical information in real-time, prioritize tasks, and document patient changes promptly. This efficient information management helps nurses maintain a clear view of each patient’s needs throughout their shift, which can be crucial for preventing oversights.
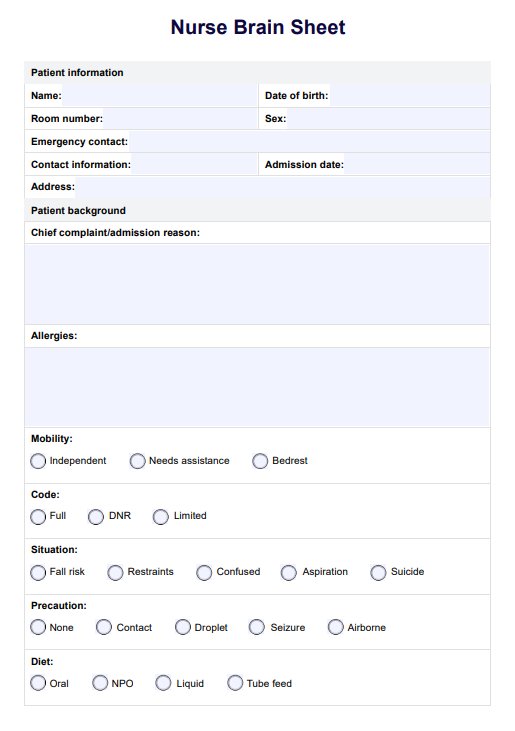
Nurse Brain Sheet
Optimize patient care with our Nurse Brain Sheet Template. Streamline communication and boost efficiency in healthcare settings.
Nurse Brain Sheet Template
Commonly asked questions
When selecting a nursing brain sheet, look for sections dedicated to critical patient details such as vital signs, medications, lab results, and notes on the care plan. Customizable brain sheets for nurses are ideal, allowing each nurse to modify the template according to specific unit needs or patient acuity levels.
Selecting the right nursing brain sheet depends on one patient, the unit’s demands, and the patient load. Test out a few templates to determine which brain sheets for nurses offer the best balance of information organization, clarity, and ease of use for your workflow.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











