Healthcare professionals, including obstetricians, midwives, and other prenatal care providers, typically request a Normal Fetal Heart Rate Chart. Expectant parents may also inquire about it during routine checkups or when they have specific concerns about fetal well-being.
Normal Fetal Heart Rate
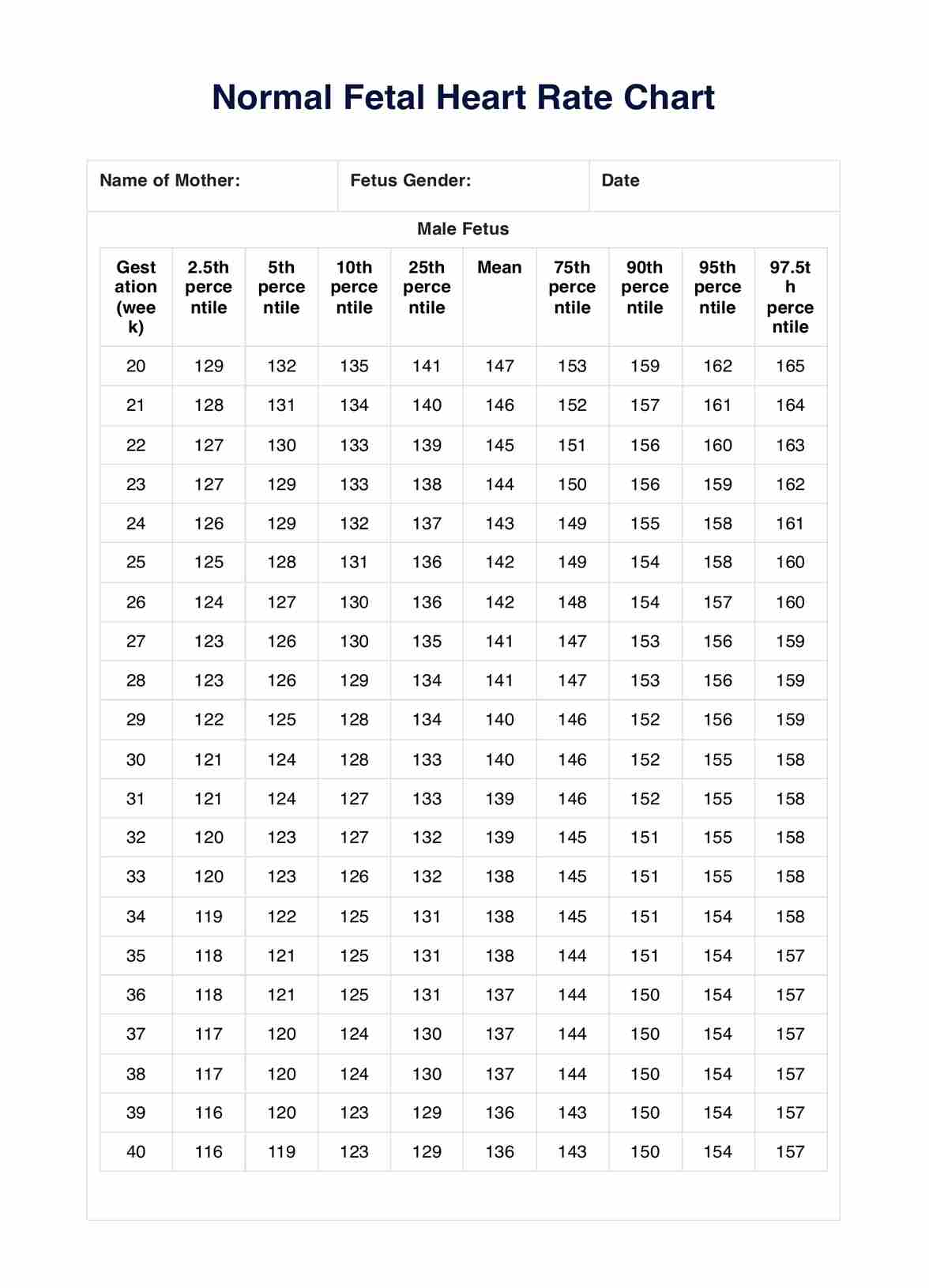
Optimize fetal monitoring with our Normal Fetal Heart Rate Chart. Download it and track fetal heart rates effortlessly and accurately.
Normal Fetal Heart Rate Template
Commonly asked questions
You use the Normal Fetal Heart Rate Chart during various stages of pregnancy. It is crucial in routine checkups, especially during the second and third trimesters. Additionally, you use it when expectant mothers experience health issues, lifestyle adjustments, medication changes, or have high-risk pregnancies that demand continuous monitoring.
Healthcare practitioners download the Normal Fetal Heart Rate Chart template and guide patients or their parents/guardians on its usage. The process involves taking the fetal heart rate, comparing it against the chart, recording the findings, and discussing the results with the healthcare provider. The chart is a visual aid that simplifies the interpretation of fetal heart rate patterns.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











