List of Mood Disorders
Use our List of Mood Disorders as a quick reference of symptoms to help clients going through these challenges.


What are mood disorders?
Mood disorders represent a category of mental health conditions characterized by significant and persistent disturbances in a person's emotional state. These disturbances are specified in the Diagnostic and Statistical Manual of Mental Disorders as conditions that significantly impact an individual's daily functioning, affecting everything from personal relationships to job performance.
Key indicators of mood disorders vary widely among individuals but often include noticeable changes in mood, energy levels, and behavior. Individuals may exhibit:
- Persistent sadness or depressed mood
- Feelings of hopelessness or pessimism
- Irritability or frustration
- Loss of interest in activities once enjoyed
- Changes in sleep patterns and appetite
- Difficulty concentrating, remembering, or making decisions
- Physical symptoms that are unexplained by other health conditions
Mood disorders represent a significant and diverse category. It is then essential for practitioners to understand the risk factors and different types of mood disorders that patients may experience. This understanding can help diagnose and tailor treatment strategies effectively for each patient's unique situation. The following defines how mood disorders are often categorized into:
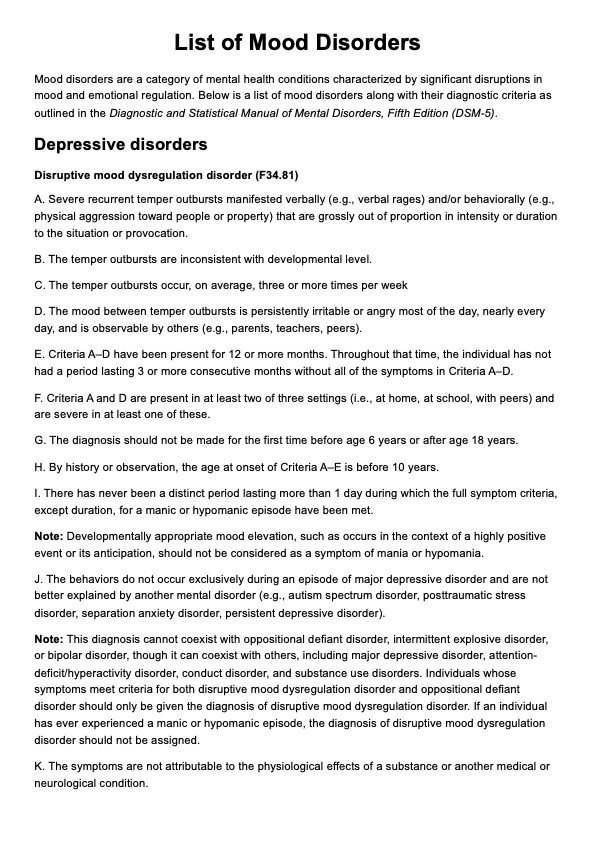
Depressive disorders
The category of depressive disorders includes several conditions marked by feelings of extreme sadness or a loss of interest in life. Here's a closer look at some critical types:
- Major depression: This form of clinical depression is characterized by an intense, persistent feeling of depression that lasts for at least two weeks. The depressive symptoms can significantly impair an individual's ability to function in daily life.
- Seasonal affective disorder (SAD): SAD is a type of depression that occurs at specific times of the year, typically during the fall and winter months, when there's less natural sunlight.
- Persistent depressive disorder: Known for its long-term grip, this form of depression stretches out for two years or more, often making it difficult for individuals to remember a time when they felt well.
- Disruptive mood dysregulation disorder: This disorder is diagnosed in children and teenagers and is characterized by severe and persistent irritability and episodes of extreme, disproportionate anger.
- Premenstrual dysphoric disorder: This involves severe mood disturbances that occur as premenstrual symptoms, significantly more severe than typical premenstrual syndrome.
Bipolar and related disorders
Bipolar disorders are marked by dramatic shifts in a person's mood, energy, and ability to think clearly. These shifts range from highs (mania or hypomania) to lows (depression), affecting their behavior and functioning significantly.
- Bipolar I disorder: Individuals with this disorder experience manic episodes that last at least a week or are so severe that hospital care is needed. These episodes are characterized by an enduring period of significantly elevated or irritable mood and inflated self-esteem, among other symptoms.
- Bipolar II disorder: This condition is defined by a pattern of depressive episodes shifting back and forth with hypomanic episodes, which are less severe than the full-blown mania of bipolar I.
- Cyclothymic disorder: Those diagnosed with cyclothymia experience milder, yet chronic, mood swings from highs to lows. These mood changes are less extreme than the ones found in bipolar I or II disorders but can still hinder one's daily life.
List of Mood Disorders Template
List of Mood Disorders Example
How to use this List of Mood Disorders PDF?
This handout tool is designed to help healthcare practitioners better understand and identify various mood disorders. It outlines common mood disorders and their symptoms for informed and empathetic care. Feel free to follow these steps as you use this resource to help you in practice:
Step 1: Access the handout
Click the "Use template" to customize the handout within the Carepatron platform before printing or sending a copy to clients. You can also click "Download" for a free PDF copy.
Step 2: Familiarize the content of the handout
Recognize the characteristics of the most common mood disorders. Major depressive disorder is known for persistent sadness and loss of interest. Other specifiers can also include peripartum onset or postpartum depression and mild to severe depression. Bipolar disorders encompass a spectrum of mood swings ranging from depressive lows to manic or hypomanic highs.
Step 3: Individualize patient care
Understand that no two patients are alike. Gather comprehensive life and symptom histories to inform your diagnoses. Engage with patients about their experiences and adjust evaluation and treatment strategies based on their feedback and clinical observations.
Step 4: Use standard tools
Conduct validated screening and diagnostic tools to help quantify symptoms and their impact. Use assessment tools such as the Mood Disorder Questionnaire and clinical judgment for a more complete picture of the patient's mental health status, leading to a more precise diagnosis and tailored treatment plans.
How are mood disorders treated?
As there are a wide range of mood disorders that also significantly differ in their presentation, there are also different methods that a mental health professional typically uses to treat mood disorders. This includes the following:
Psychotherapy
Also known as talk therapy, psychotherapy is a commonly used method in treating mood disorders. It provides a supportive environment for patients to discuss their feelings and thoughts and to identify and change troubling emotions, thoughts, and behaviors.
Cognitive behavioral therapy (CBT)
CBT is particularly effective for mood disorders, focusing on identifying and modifying negative thought patterns and behaviors. It teaches patients coping strategies to manage stress and challenges.
Medication
Psychiatric medications do not cure mood disorders, but they can significantly improve their symptoms.
- Antidepressants: Used primarily for depression, antidepressants such as selective serotonin reuptake inhibitors (SSRIs) can also be helpful in certain bipolar disorder cases, particularly when combined with mood stabilizers.
- Mood stabilizers: These are the go-to medication for bipolar disorder, helping control swings between depression and mania.
- Anti-anxiety medications: For those patients where anxiety is a prominent feature of their mood disorder, or their mood disorder is comorbid with generalized anxiety disorder and related conditions, these medications may offer relief.
Lifestyle modifications
Encouraging patients to make lifestyle changes can also greatly support their recovery. This usually involves recommending the following:
- Regular exercise: Physical activity is known to help reduce depression and anxiety symptoms.
- Healthy diet: A balanced diet can impact overall well-being and mood.
- Sleep hygiene: Improving sleep patterns can significantly affect mood disorder symptoms.
- Stress reduction techniques: Mindfulness, meditation, and yoga are just a few methods that can help patients manage stress better.
Commonly asked questions
Even if your symptoms don't fully align with the diagnostic criteria for mood disorders, it's crucial to seek professional help. There are also further categories for mood disorders as well such as unspecified bipolar disorder and unspecified depressive disorder, which may account for this. Many people experience subthreshold symptoms that can still significantly affect their lives and may benefit from treatment or intervention.
A mood disorder due to a general medical condition is a diagnosis given when a significant mood disturbance results directly from the physiological effects of a separate medical condition. This diagnosis underscores the direct link between the medical condition and the mood disorder symptoms.
Substance-induced mood disorders are specific types of mental health conditions characterized by depressive, anxiety, psychotic, or manic symptoms that directly result from the physiological effects of substance use, including prescription medications, illegal drugs, and alcohol. These disorders can manifest during active substance use, intoxication, or withdrawal phases.























-template.jpg)