Anxiety Nursing Diagnosis
Download our Anxiety Nursing Diagnosis PDF as a helpful reference tool to aid in your care process.


How do nurses diagnose anxiety disorders?
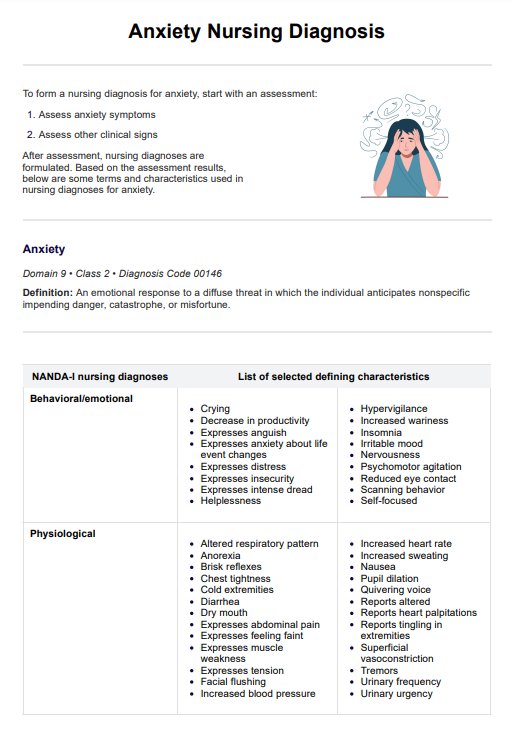
Nurses diagnose anxiety disorders by assessing a patient's anxiety symptoms and identifying related factors that contribute to emotional and physical distress. An anxiety diagnosis typically involves evaluating both physical symptoms and psychological markers, as detailed in NANDA-I's (Herdman et al., 2024) guidelines.
Anxiety disorders, including generalized anxiety disorder (GAD), panic disorder, and major depressive disorder, often involve symptoms like difficulty concentrating, irritability, hypervigilance, and panic attacks. Nurses look for defining characteristics, such as persistent feelings of dread, apprehension, or an intense sense of impending danger, even without an immediate threat. They also monitor the presence of physiological signs like increased heart rate, sweating, or muscle tension, which commonly accompany severe anxiety.
When assessing patients, nurses examine factors that may worsen anxiety symptoms. These can include interpersonal stressors, unresolved conflicts, or unmet needs. Additionally, nurses consider the patient's cognitive and emotional state, noting behaviors like hypervigilance, nervousness, or rumination, which often signal an anxiety disorder. Nurses rely on functional health patterns to collect data accurately, ensuring a comprehensive view of the patient’s mental and physical state.
Nursing interventions may include strategies to help patients manage anxiety, such as guiding relaxation techniques or providing education on anxiety management. In some cases, nurses collaborate with other healthcare professionals to suggest anti-anxiety medications as part of the treatment plan. Assessments are ongoing, and if mental health complications such as major depressive disorder or substance misuse are present, nurses adjust their approach accordingly to offer holistic care.
Examples of nursing diagnoses for anxiety
When diagnosing anxiety disorders, nurses assess both physical and cognitive symptoms that reflect the patient’s distress. These symptoms help identify the severity of anxiety and guide appropriate nursing interventions. Below are some examples of nursing diagnoses based on the observed signs and symptoms of anxiety (Cumpian, 2023):
- Anxiety related to perceived threat, evidenced by restlessness and tense appearance
- Anxiety related to chest pain secondary to heart failure, as evidenced by diaphoresis and crying
- Anxiety related to impending surgery, as evidenced by restlessness and angry outbursts
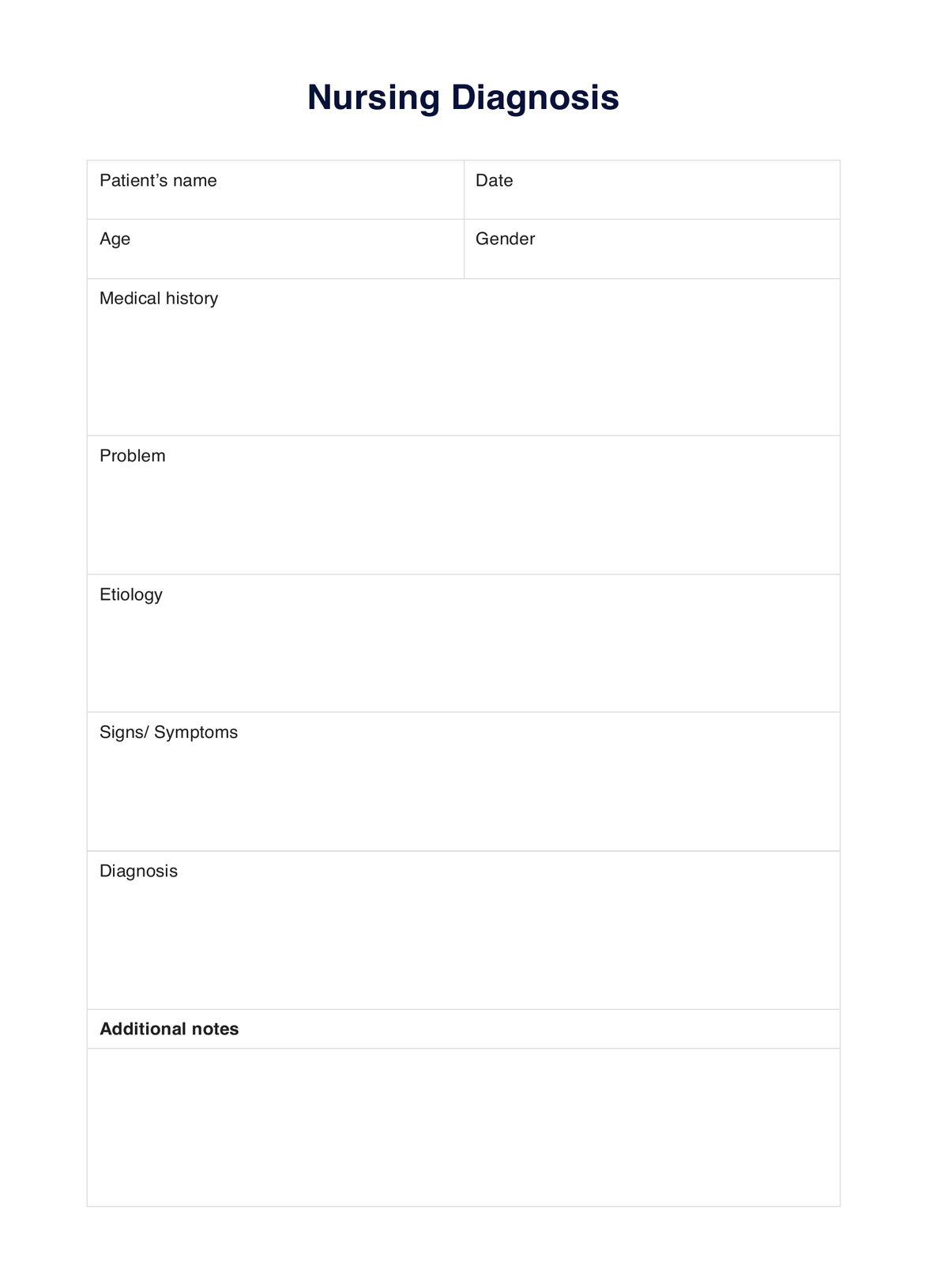
Anxiety Nursing Diagnosis Template
Anxiety Nursing Diagnosis Example
How to use our Anxiety Nursing Diagnosis template
Carepatron’s Anxiety Nursing Diagnosis template is a practical tool designed to help healthcare professionals efficiently diagnose and document anxiety disorders. By following the steps below, practitioners can systematically evaluate anxiety symptoms, make accurate diagnoses, and develop an effective care plan tailored to each patient’s needs.
Step 1: Access the template
To begin, locate the Anxiety Nursing Diagnosis template within this guide by clicking on "Use template" to access it within the Carepatron platform. You can also click "Download" to get a fillable PDF copy. This resource is readily accessible and designed to guide you through the diagnosis process, providing a structured reference tool.
Step 2: Review the diagnosis template
Before using the template with a patient, review its layout and sections. Familiarize yourself with the fields related to anxiety symptoms, such as physiological, emotional, and cognitive indicators, to ensure you’re aware of the information to collect for an accurate anxiety disorder diagnosis.
Step 3: Use the template for diagnosing anxiety
While assessing the patient, you can use the additional notes section to take notes. Document observable anxiety symptoms, like difficulty concentrating, irritability, or physical indicators of severe anxiety. This structured approach helps ensure no essential information is overlooked in diagnosing generalized anxiety disorder or related conditions.
Step 4: Discuss findings with the patient
After completing the assessment, share your findings with the patient in an approachable, supportive manner. Clearly explain any anxiety symptoms observed and describe how they relate to their overall mental health. This discussion builds understanding and encourages patient engagement in managing their anxiety disorder.
Step 5: Provide patient education and next steps
Finally, educate patients on anxiety and possible treatment options. Outline steps they can take, including lifestyle adjustments, coping strategies, and, if necessary, anti-anxiety medications. Establishing clear next steps helps patients feel empowered and informed about managing their condition effectively.
What criteria do nurses follow for diagnoses?
NANDA-I, originally known as the North American Nursing Diagnosis Association, is a global professional organization that develops and maintains a comprehensive taxonomy of nursing diagnoses. This organization aims to improve patient care through standardized terminology that reflects actual or potential human responses to health problems and life processes, based on empirical research findings.
NANDA-I outlines specific criteria for formulating nursing diagnoses, which typically include three components:
- Diagnosis label: An approved diagnosis from the NANDA-I list.
- Related factors: A statement identifying the underlying causes or contributing factors associated with the diagnosis.
- Defining characteristics: Observable cues or evidence that support the diagnosis, often described as "as evidenced by" statements
What interventions can nurses provide for those with anxiety?
Nurses play a key role in supporting patients with anxiety disorders by providing interventions that reduce symptoms of anxiety and enhance overall well-being. These interventions address both physical and cognitive symptoms associated with anxiety and are tailored to manage varying levels of mild anxiety to more intense episodes, such as panic attacks.
Therapeutic communication
Nurses use therapeutic communication to create a safe, supportive space where patients feel comfortable discussing their feelings. This approach is crucial when a disorder involves anxiety symptoms that may not be easy for patients to express. By actively listening and showing empathy, nurses help alleviate patients' distress and reduce their anxiety-provoking situations.
Relaxation techniques
For patients experiencing mild anxiety or social anxiety disorder, nurses can teach relaxation techniques like deep breathing, progressive muscle relaxation, or guided imagery. These practices help decrease physical symptoms such as chest pain and tension. They are especially helpful for patients whose anxiety symptoms produce clinically significant distress.
Education on anxiety and triggers
Educating patients on anxiety disorders and potential triggers empowers them to understand their condition better. Nurses explain how mental disorders like anxiety can arise from stress, medical conditions, or life events. By helping patients recognize and avoid specific anxiety-provoking situations, nurses support the long-term management of their symptoms of anxiety.
Coping strategies for panic attacks
In cases of intense anxiety, like panic attacks, nurses can guide patients through coping strategies to manage acute distress. Techniques such as grounding exercises or mindfulness help patients re-center themselves during episodes, reducing the physical and cognitive symptoms often associated with severe anxiety.
Collaborative care and referrals
When anxiety disorders occur alongside other mental disorders or when anxiety symptoms indicate complex health issues, nurses may collaborate with mental health specialists or refer patients for further care. This interdisciplinary approach ensures patients receive comprehensive support tailored to their individual needs and clinical context.
Reference
Herdman, T. H., Kamitsuru, S., & Lopes, C. T. (2024). NANDA International nursing diagnoses: Definitions & classification, 2024-2026 (13 2024). Thieme. https://nanda.org/publications-resources/publications/nanda-international-nursing-diagnoses/
Cumpian, T. (2023, July 22). Anxiety nursing diagnosis & care plan. NurseTogether. https://www.nursetogether.com/anxiety-nursing-diagnosis-care-plan/
Commonly asked questions
The nursing diagnosis for anxiety is characterized by feelings of unease, dread, or apprehension in response to perceived threats, often accompanied by physical and cognitive symptoms like restlessness, tension, or difficulty concentrating. It enables nurses to identify specific anxiety symptoms and plan targeted interventions to help the patient manage their condition.
Key nursing interventions for a client with an anxiety disorder include providing therapeutic communication, teaching relaxation techniques, and helping the patient recognize and manage anxiety triggers. These interventions aim to reduce distress and improve coping skills for managing anxiety symptoms effectively.
Nurses follow NANDA-I guidelines and standardized frameworks, like functional health patterns, to assess physical, cognitive, and emotional symptoms when diagnosing anxiety disorders. These guidelines ensure an accurate and comprehensive diagnosis, supporting effective care planning and intervention.























-template.jpg)













































































