Addiction and the Brain: List of Therapies
Explore the relationship between addiction and the brain, learn about various therapies, and access a free PDF with examples of effective treatment strategies.


What does drug abuse do to the brain?
The human brain, a marvel of complexity, governs all facets of our existence. This intricate organ, weighing merely three pounds, orchestrates every aspect of human activity. The brain is indispensable from essential bodily functions to the enjoyment of everyday pleasures. It regulates fundamental bodily processes, interprets stimuli, and guides behavior. Essentially, the brain encapsulates your thoughts, emotions, and identity, shaping your very being.
Drug abuse disrupt the intricate process of neural communication by affecting how neurons transmit, receive, and process signals through neurotransmitters. For instance, substances like marijuana and heroin possess brain chemicals makeup resembling natural neurotransmitters, enabling them to bind to and activate neurons.
However, their activation doesn't mirror that of natural neurotransmitters, leading to distorted messages within the neural network.
Conversely, drugs like amphetamine or cocaine prompt neurons to release excessive amounts of neurotransmitters or hinder their regular recycling, further distorting or intensifying neural communication
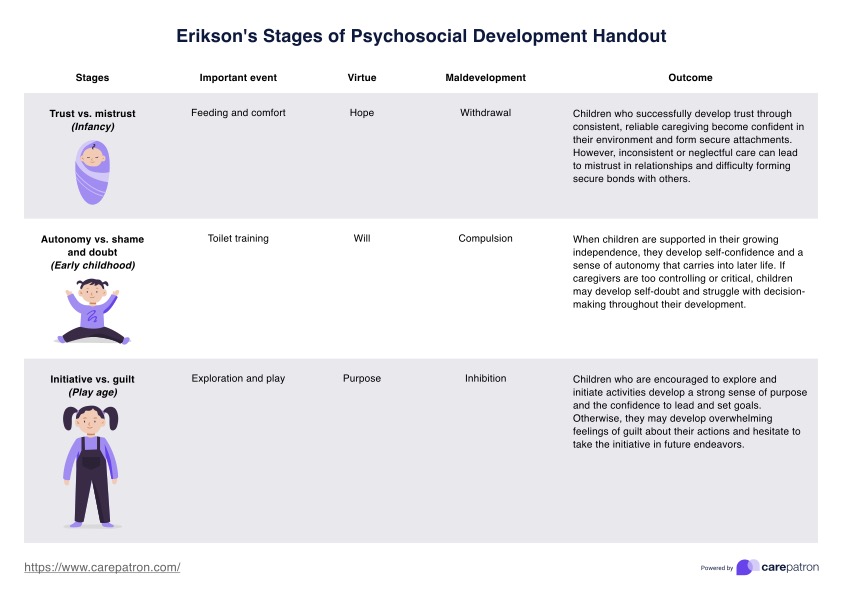
Substance abuse can impact vital brain regions crucial for sustaining life functions and driving compulsive drug-seeking behaviors associated with addiction. These include the basal ganglia, which play a pivotal role in positive motivation, encompassing pleasurable experiences like eating, socializing, and sexual activities, as well as habit formation.
Terming the brain's 'reward circuit,' these areas are excessively stimulated by drugs, leading to the euphoria of a drug-induced high. However, with prolonged use, the circuitry adapts, reducing its sensitivity and impairing the ability to derive pleasure from non-drug-related cues.
The extended amygdala is involved in generating stressful emotions such as anxiety, irritability, and unease, commonly experienced during withdrawal once the drug's effects wear off. This heightened sensitivity of the circuit drives individuals to seek the drug again.
With continued drug use, this circuit becomes increasingly reactive. Consequently, individuals with substance use disorder may resort to drugs not solely for the euphoric effects but rather to alleviate the discomfort of withdrawal symptoms.
Lastly, the prefrontal cortex controls decision-making and impulse control, particularly vulnerable during adolescence. Imbalances between this area and others involved in motivation and emotional response drive compulsive drug-seeking behavior in individuals with substance use disorder. Furthermore, opioids and other drugs can disrupt vital brainstem functions, such as regulating breathing and heart rate, leading to fatal overdoses.
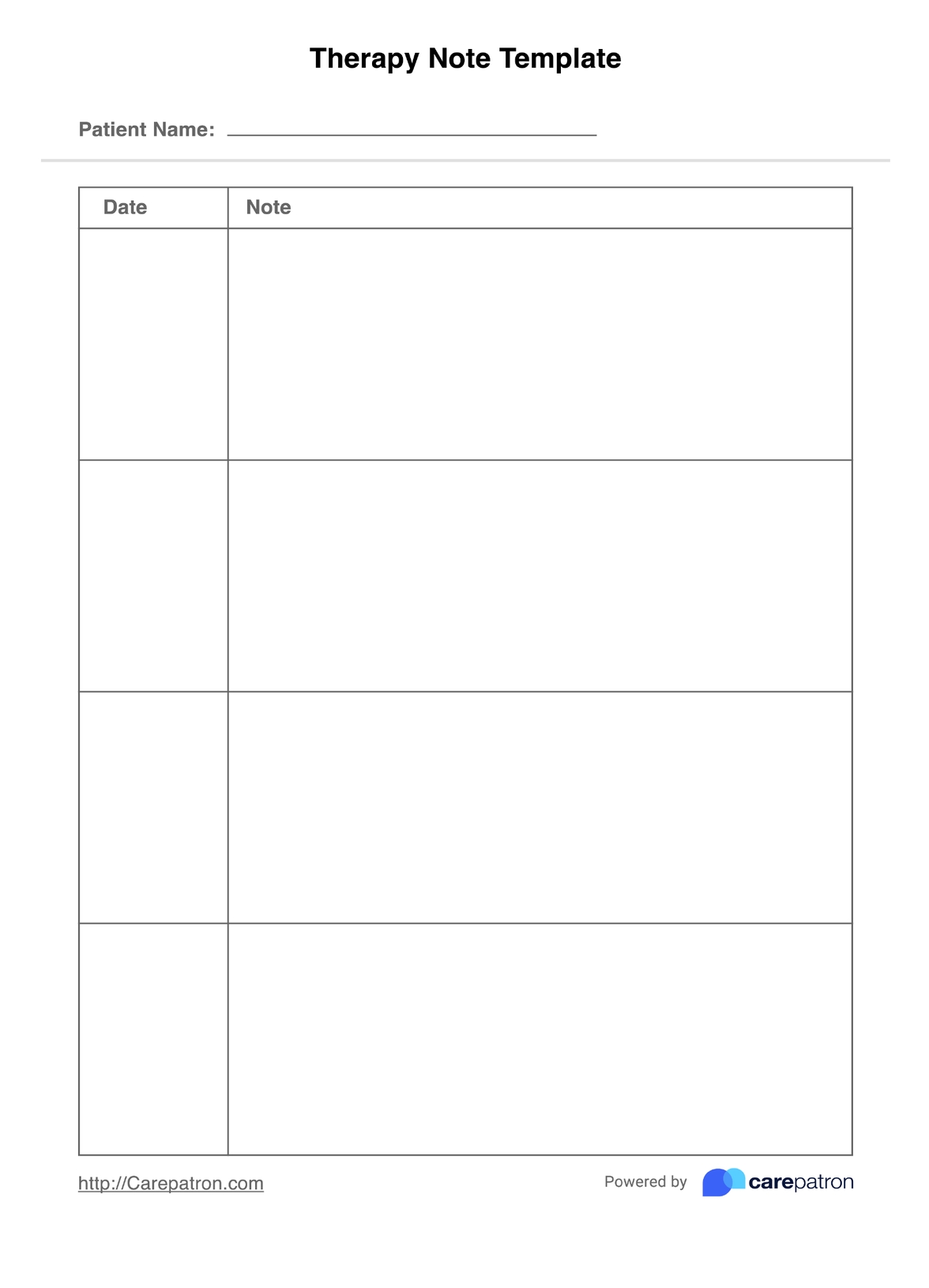
Addiction and the Brain: List of Therapies Template
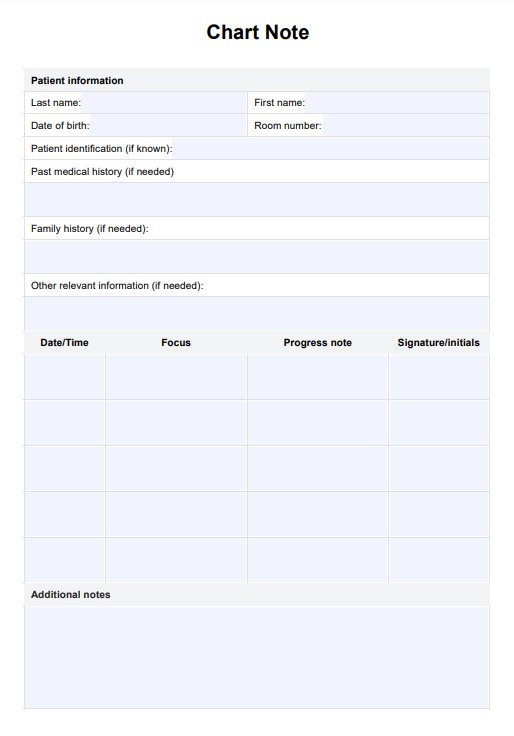
Addiction and the Brain: List of Therapies Example
What happens to the brain during withdrawal symptoms
During the withdrawal stage of drug usage, the brain undergoes significant changes as it adapts to the absence of the substance. Withdrawal symptoms can manifest in various ways, impacting both mental and physical well-being. Understanding these changes is crucial for comprehending the challenges individuals face during recovery.
Mental results
Withdrawal from addictive drugs often precipitates mental symptoms characterized by cognitive impairment, including difficulty concentrating, memory problems, and impaired decision-making abilities.
These cognitive deficits stem from neurotransmitter levels and disrupted neural circuitry alterations, particularly in regions responsible for executive function, such as the prefrontal cortex.
Additionally, individuals may experience heightened anxiety, irritability, and mood swings as the brain stem struggles to restore equilibrium in the absence of the drug's effects.
Physical results
Physically, withdrawal symptoms can manifest as flu-like symptoms, including nausea, vomiting, muscle aches, brain disease, and tremors. These symptoms arise as the body detoxifies from the substance and attempts to regain homeostasis.
Moreover, individuals may experience changes in appetite, sleep disturbances, and heart rate and blood pressure fluctuations. These physical manifestations underscore the profound impact of drug withdrawal on the body's physiological processes.
Emotional results
Emotionally, withdrawal can evoke intense feelings of dysphoria, depression, and dysregulation of emotions. The brain's reward circuitry, including the extended amygdala, undergoes dysregulation, leading to heightened stress responses and emotional instability.
Individuals may also experience cravings for the drug as the brain's reward system becomes hypersensitive to cues associated with substance use.
Addressing these emotional challenges is essential in supporting individuals through the withdrawal process and promoting long-term recovery.
What parts of the brain are affected by substance abuse?
Substance abuse exerts a profound impact on various regions of the brain, disrupting neural circuitry and neurotransmitter systems implicated in addiction. Understanding how different parts of the brain are affected by drug use is essential for devising effective treatment strategies and interventions.
Addiction inside neurons
Within neurons, drug addiction alters the intricate machinery of neurotransmission. Drugs interact with the brain's neurotransmitter systems, particularly the dopamine system, which plays a central role in reward processing and reinforcement.
Prolonged drug use leads to dysregulation of dopamine signaling, resulting in diminished sensitivity to natural rewards and an increased drive to seek drugs.
These neuroadaptive changes perpetuate the cycle of addiction, driving individuals to prioritize drug-seeking behaviors over other life-sustaining activities.
Addressing addiction inside neurons involves restoring balance to neurotransmitter systems through pharmacological interventions and behavioral therapies aimed at retraining the brain's reward circuitry.
Addiction and dopamine receptors
Dopamine receptors play a pivotal role in mediating the rewarding effects of drugs and reinforcing drug-seeking behaviors. Chronic drug use leads to alterations in dopamine receptor density and function, contributing to the development of tolerance and dependence.
Moreover, drugs of abuse hijack the brain's natural reward system, flooding it with unnaturally high levels of dopamine, which can lead to long-lasting changes in receptor expression and sensitivity. As a result, individuals may experience cravings and compulsive drug-seeking behaviors even in the absence of external cues.
Understanding the intricate interplay between addiction and dopamine receptors is crucial for developing targeted therapies to restore normal dopaminergic function and treat addiction effectively.
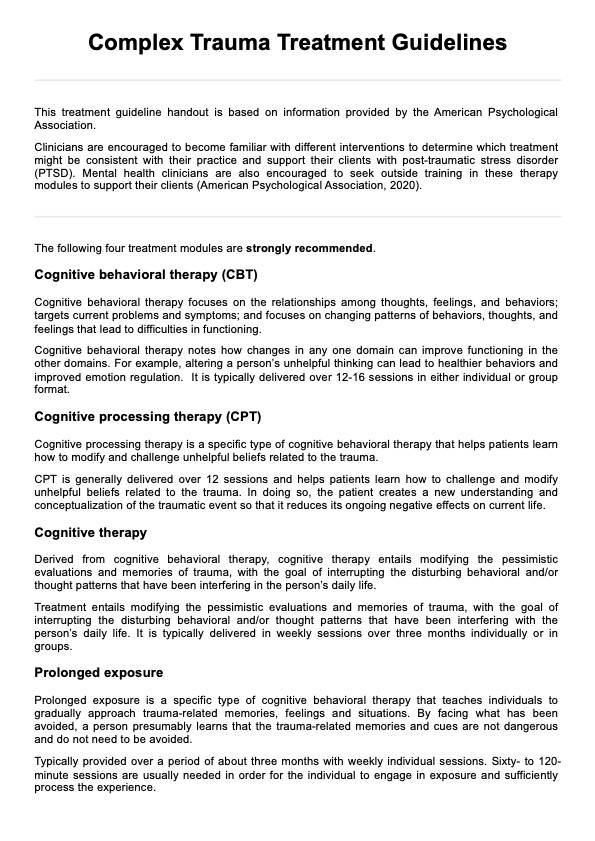
Brain therapies for addiction
Brain therapies offer promising avenues for treating addiction by targeting neural mechanisms underlying substance use disorders. Here are some therapies aim to restore normal brain function and promote recovery from addiction:
Brain imaging studies
Brain imaging studies, such as functional magnetic resonance imaging (fMRI) and positron emission tomography (PET), provide valuable insights into the neural correlates of addiction.
These techniques enable researchers to visualize brain changes associated with drug addiction, including alterations in neurotransmitter systems, changes in brain structure and function, and disruptions in reward circuitry.
Furthermore, neuroimaging techniques facilitate the monitoring of treatment progress and the evaluation of intervention efficacy, guiding clinical decision-making in addiction management.
Brain stimulation
Brain stimulation techniques, such as transcranial direct current stimulation (tDCS) and deep brain stimulation (DBS), modulate neural activity in targeted brain regions implicated in addiction.
tDCS delivers low-intensity electrical currents to the brain's surface, modulating cortical excitability and influencing neural networks involved in craving, impulsivity, and decision-making.
DBS involves the implantation of electrodes into specific brain regions, such as the nucleus accumbens or prefrontal cortex, to modulate neuronal activity and regulate dysfunctional circuits associated with addiction.
Transcranial magnetic stimulation
Transcranial magnetic stimulation (TMS) is a non-invasive brain stimulation technique that delivers magnetic pulses to targeted brain regions.
TMS has shown efficacy in reducing cravings and promoting abstinence in individuals with drug addiction, offering a promising adjunctive treatment option alongside traditional pharmacotherapy and behavioral interventions. Moreover, TMS is well-tolerated and devoid of systemic side effects, making it a safe and viable option for treating addiction-related brain changes.
Ongoing research efforts aim to optimize TMS protocols further and identify optimal stimulation parameters for maximizing therapeutic outcomes in addiction treatment.
Commonly asked questions
During addiction, the brain undergoes changes in its reward circuitry, including alterations in neurotransmitter levels, particularly dopamine. This leads to compulsive drug-seeking behavior and diminished sensitivity to natural rewards.
Addiction and narcissism are distinct conditions, but some individuals with addiction may display narcissistic traits. However, addiction is primarily driven by neurological and psychological factors rather than personality traits like narcissism.
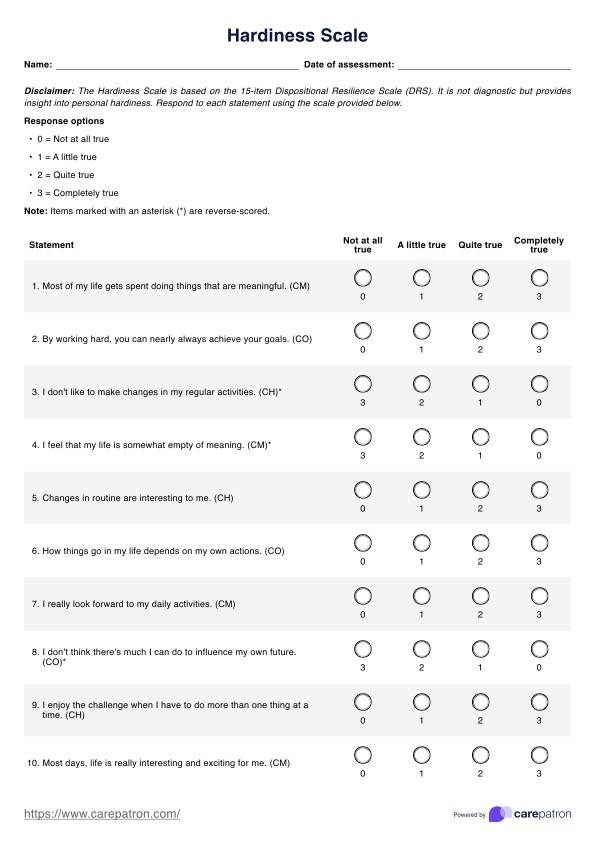
The 5 recovery skills include coping strategies for managing cravings and triggers, building a supportive network, developing problem-solving skills, practicing self-care, and cultivating resilience in the face of setbacks.







-template.jpg)