Renin Test
Learn about Renin Test: A crucial diagnostic tool for hypertension and kidney health. Find out how it works and its importance in healthcare.


What is a Renin Test?
A Renin Test, also known as plasma renin activity (PRA) or plasma renin concentration (PRC), is a diagnostic laboratory examination that measures the renin level in a patient's blood. This test is paramount in healthcare, particularly for healthcare practitioners dealing with hypertension, kidney diseases, and endocrine disorders.
Renin is an enzyme produced and released by the juxtaglomerular cells of the kidneys. Its primary role is to regulate blood pressure and fluid balance within the body. This is achieved by initiating the renin-angiotensin-aldosterone system (RAAS). This complex hormonal cascade ultimately leads to the constriction of blood vessels and the retention of sodium and water, thereby increasing blood pressure.
The test procedure typically involves drawing a blood sample, and the measurement can be expressed as either plasma renin activity (PRA) or plasma renin concentration (PRC). These results provide crucial insights into the patient's physiology, helping practitioners make informed decisions regarding treatment, which may include medications to control blood pressure, surgical interventions for renal artery stenosis, or further evaluation for underlying conditions.
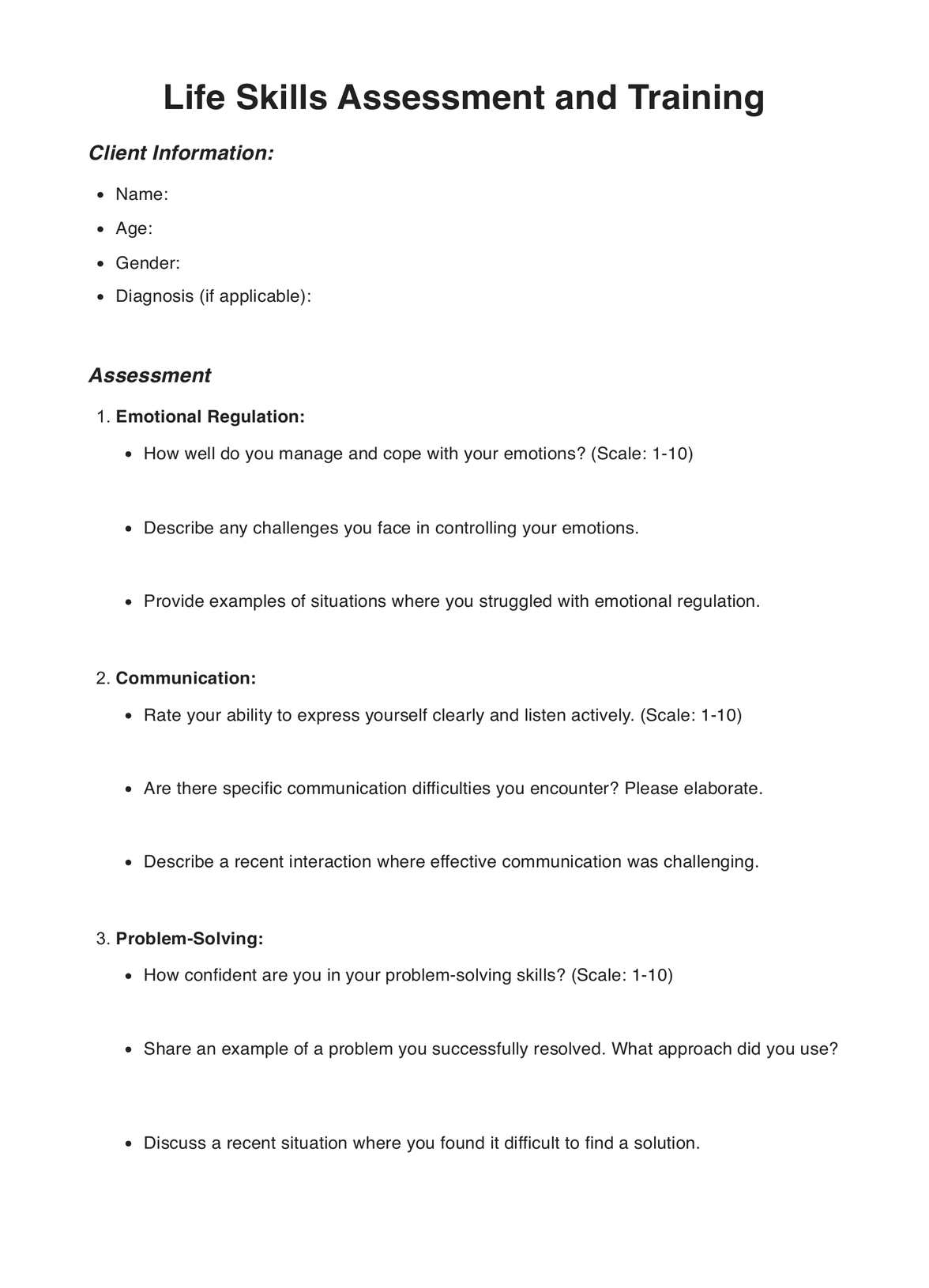
Renin Test Template
Renin Test Example
How Does it Work?
A Renin Test is a fundamental diagnostic tool in healthcare, particularly for assessing blood pressure and kidney health. Using and filling out the Renin Test Results and Interpretation Form involves several key steps to ensure accurate results and appropriate patient care.
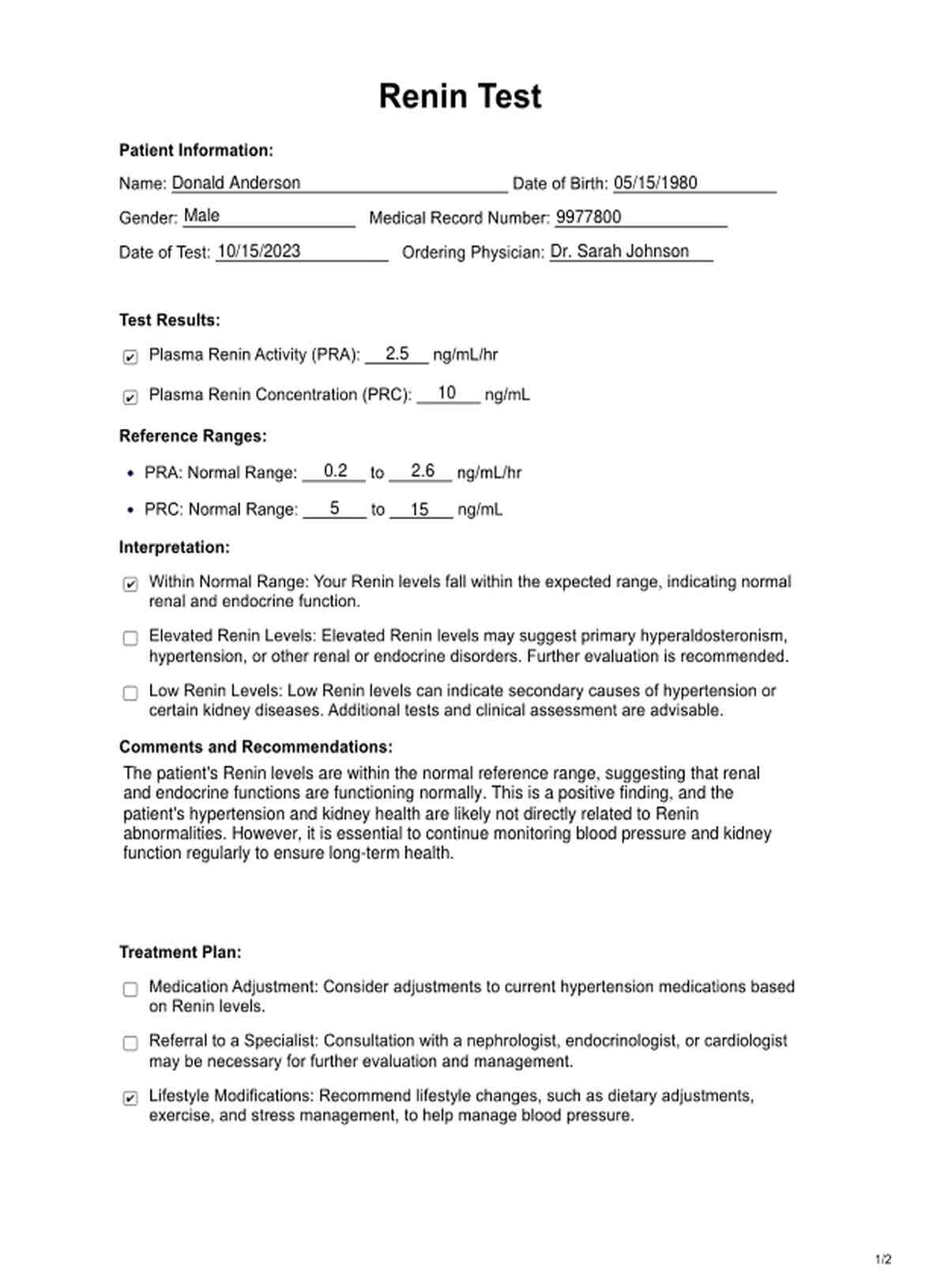
1. Patient Information
The first step in using the form is to gather essential patient information. This includes the patient's name, date of birth, gender, medical record number, and test date. This information is crucial for maintaining accurate medical records and ensuring the results are associated with the correct patient.
2. Test Results
The next step involves recording the actual Renin test results. This includes measuring the Plasma Renin Activity (PRA) and Plasma Renin Concentration (PRC) from the blood sample collected. These numerical values provide insights into the patient's Renin levels.
3. Reference Ranges
It's vital to compare the obtained results to the established reference ranges for Renin levels. These reference ranges are specific to the laboratory or institution performing the test and help determine whether the patient's Renin levels are within a normal range.
4. Interpretation
The form includes interpretation options based on the test results. Healthcare practitioners must select the appropriate interpretation based on whether the patient's Renin levels are within the normal range, elevated, or low.
5. Comments and Recommendations
In this section, healthcare practitioners can provide additional context, comments, and recommendations based on the test results. This might include suggestions for further evaluation, medication adjustments, lifestyle modifications, or specialist referrals.
6. Treatment Plan
The form outlines potential treatment plans, including adjusting medications, referring the patient to a specialist, and recommending lifestyle modifications. The healthcare practitioner can select the most relevant options based on the patient's situation.
7. Follow-Up
To ensure continuity of care, a follow-up appointment date should be scheduled. This enables the healthcare practitioner to re-evaluate Renin levels and assess the effectiveness of any treatment or lifestyle changes.
The completed form is a valuable tool for healthcare practitioners to document and communicate test results and recommendations clearly to the patient. It is printable, making it a tangible record that can be shared with patients for their reference and future healthcare needs.
When would you use this test?
The Renin Test is a valuable diagnostic tool primarily utilized by healthcare practitioners, including cardiologists, nephrologists, endocrinologists, and general practitioners, in various clinical scenarios to assess blood pressure regulation and kidney function. Here are the key instances when this test is appropriately employed:
Hypertension Diagnosis and Management
One of the primary indications for a Renin Test is in evaluating hypertension, commonly known as high blood pressure. Elevated blood pressure is a widespread health concern that increases the risk of heart disease, stroke, and kidney problems. Practitioners use the Renin Test to identify the underlying causes of hypertension, such as primary hyperaldosteronism, which leads to excess aldosterone production and high blood pressure. By understanding the Renin levels, healthcare professionals can make informed decisions about treatment strategies, including medication adjustments.
Kidney Health Assessment
The Renin Test is instrumental in assessing kidney function and identifying kidney-related disorders. Abnormal renal levels may signal issues such as renal artery stenosis or renal parenchymal diseases, which can compromise kidney health. For nephrologists and other kidney specialists, this test aids in pinpointing the cause of kidney dysfunction and guiding appropriate management.
Endocrine Disorders
Endocrinologists use the Renin Test to diagnose conditions related to the endocrine system, particularly when there's suspicion of hormone imbalances. For instance, Conn's syndrome, characterized by excessive aldosterone production, is diagnosed using the Renin Test. It helps to differentiate primary from secondary causes of this endocrine disorder.
Uncontrolled Hypertension
In cases where a patient's blood pressure remains uncontrolled despite standard treatments, the Renin Test can be an essential resource. It allows practitioners to investigate whether an underlying condition, such as primary hyperaldosteronism, contributes to hypertension.
Cardiovascular Risk Assessment
Cardiologists may employ the Renin Test to assess cardiovascular risk factors, as hypertension is a significant risk factor for heart diseases. By understanding Renin levels, they can gauge the patient's risk profile and tailor preventive measures accordingly.
Medication Optimization
Healthcare practitioners may use this test to optimize the choice and dosage of antihypertensive medications. It helps tailor treatment to the patient's needs and improve overall management.
What do the results mean?
The results of a Renin Test, also called a Free Renin Test, provide essential insights into a patient's blood pressure regulation and kidney health. This test measures the renin concentration in the blood, and interpreting the results is pivotal for healthcare practitioners in various clinical contexts.
Normal Results
When Renin levels fall within the established reference range, the patient's blood pressure and kidney function operate within expected norms. This reassuring result suggests no immediate concerns regarding hypertension or kidney-related disorders.
Elevated Renin Levels
Elevated Renin levels can indicate specific health conditions, most notably primary hyperaldosteronism. This condition involves excessive production of aldosterone, a hormone that regulates sodium and potassium levels in the body. Elevated Renin levels may lead to hypertension due to increased sodium and water retention. It is crucial to further investigate the cause of the elevated Renin, as it could signify underlying issues that need attention. Healthcare practitioners may consider referrals to specialists for in-depth evaluation and management.
Low Renin Levels
Low Renin levels are concerning as they may suggest secondary causes of hypertension or kidney diseases, including renal artery stenosis or renal parenchymal disorders. A low Renin result implies reduced renin-angiotensin-aldosterone system (RAAS) activation, which is essential for blood pressure regulation. Practitioners should investigate the potential reasons for low Renin levels, which often necessitates further testing and clinical assessment. The treatment approach will vary depending on the specific diagnosis.
Research & Evidence
The history of the Renin Test can be traced back to the mid-20th century when the Renin-Angiotensin-Aldosterone System (RAAS) was first discovered and described. In 1959, Robert W. Berliner and his colleagues identified the enzyme renin, a key RAAS component responsible for regulating blood pressure and fluid balance.
In the years following the discovery of renin, extensive research was conducted to understand its role in blood pressure regulation and its potential as a diagnostic tool.
Over the past few decades, numerous studies have been conducted to evaluate the clinical utility of the Renin Test. These studies have investigated the diagnostic value of Renin measurements in various medical conditions, with a primary focus on hypertension, kidney disease, and endocrine disorders.
A study published in the "Journal of Hypertension" in 2019 explored using Renin measurements to guide antihypertensive therapy. The research highlighted the importance of accurate Renin assessment in tailoring medication regimens, particularly in cases of resistant hypertension.
Another study in the "Journal of the American Society of Nephrology" in 2018 examined the role of the Renin-Angiotensin System in kidney disease. It demonstrated how measuring Renin levels is instrumental in identifying renal artery stenosis, which often results in secondary hypertension.
The "American Journal of Kidney Diseases" published research in 2020 that assessed the use of Renin measurements in diagnosing endocrine disorders, particularly primary hyperaldosteronism. This research emphasized the significance of Renin as a diagnostic tool in endocrinology.
These studies and numerous others have consistently demonstrated the clinical utility of Renin measurements in diagnosing and managing conditions related to blood pressure, kidney health, and endocrine disorders. The Renin Test has evolved into a well-established diagnostic tool with a robust research foundation and evidence supporting its use, making it an invaluable resource for healthcare practitioners.
References
Berliner, R. W., Cournand, A., & Donald, D. E. (1959). The Renin-Angiotensin-Aldosterone System: An Appraisal of Its Importance in Physiology and Pathology. Physiological Reviews, 39(1), 97-156.
Carey, R. M., Sakhuja, S., & Calhoun, D. A. (2019). Research and Clinical Practice: The Evolution of Hypertension Diagnosis and Treatment. Journal of Hypertension, 37(3), 433-441.
Garovic, V. D., & August, P. (2018). Role of the Renin-Angiotensin System in Renal Vasculature in Hypertension. Journal of the American Society of Nephrology, 29(12), 2957-2965.
Sweeney, A. T., & Krishnan, G. M. (2020). Approach to the Diagnosis of Primary Aldosteronism. American Journal of Kidney Diseases, 75(4), 499-503.
Commonly asked questions
A Renin Test is typically performed to assess blood pressure regulation and kidney function. It helps diagnose and manage hypertension, kidney diseases, and endocrine disorders like primary hyperaldosteronism.
The test involves drawing a blood sample from the patient, usually from a vein in the arm. The collected blood is then sent to a laboratory for analysis. Results are typically expressed as Plasma Renin Activity (PRA) or Plasma Renin Concentration (PRC).
Normal reference ranges for Renin levels can vary by laboratory and measurement method. It is essential to interpret the results in the context of the specific reference ranges provided by the testing facility.













-template.jpg)