PTSD Symptom Scale
If you have a patient suffering from PTSD and you’re looking to treat it, use this nifty PTSD Symptom Scale (PSS) to gauge the symptoms and the severity of their PTSD.


What is the PTSD Symptom Scale (PSS)?
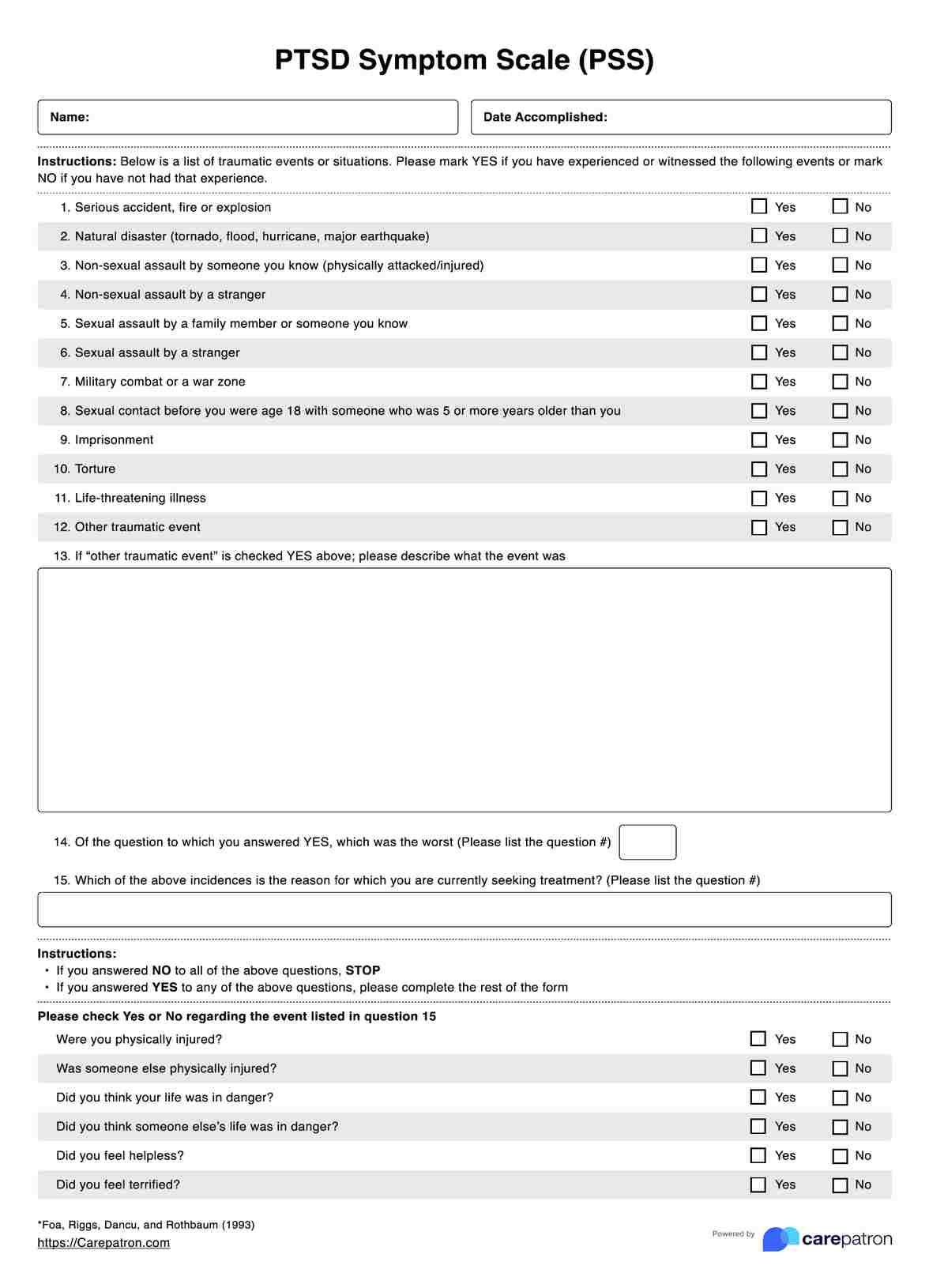
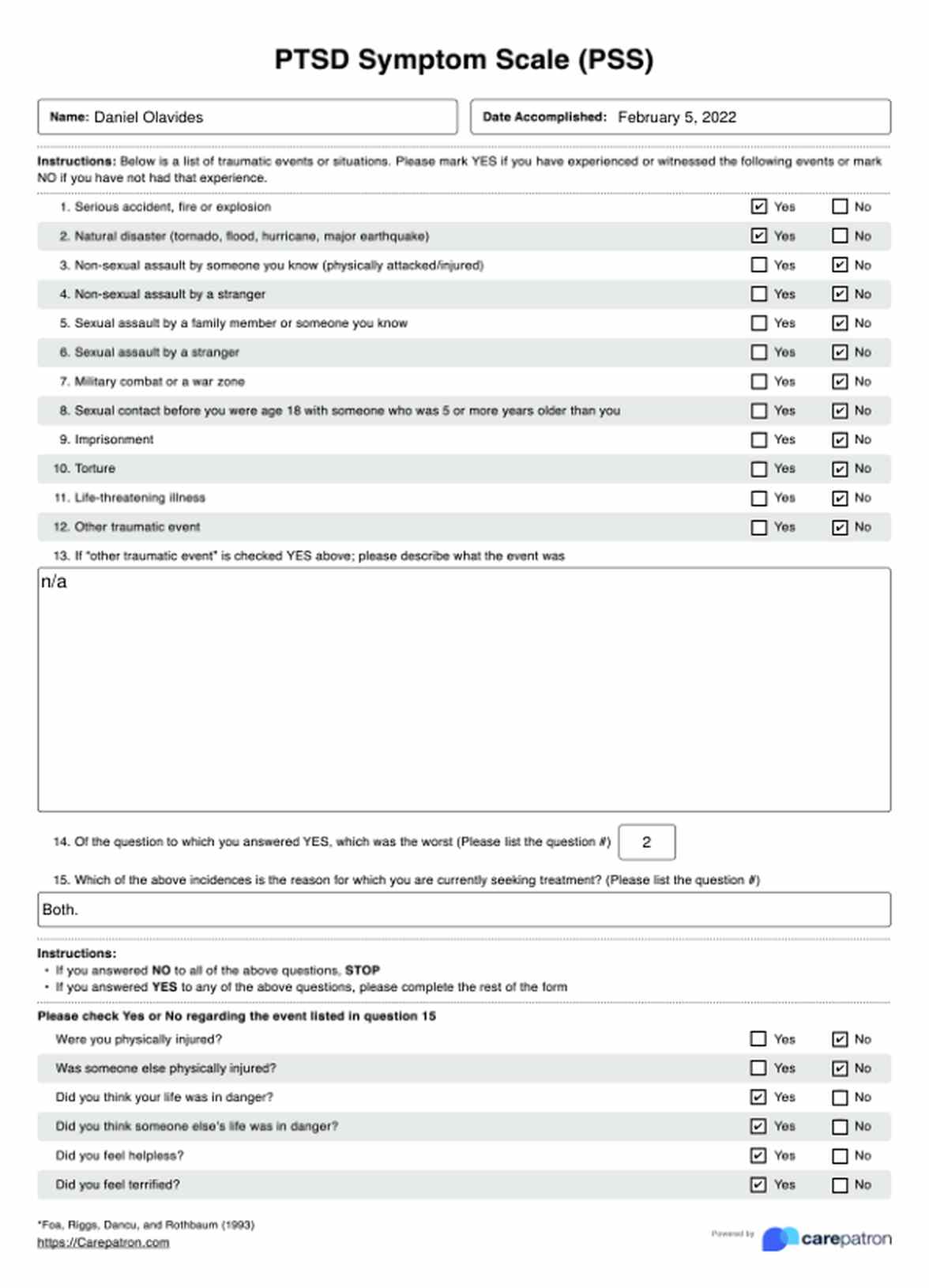
The PTSD Symptom Scale (PSS) was created by Edna B. Foa, David S. Riggs, Constance V. Dancu, and Barbara O. Rothbaum in 1993. It was developed for healthcare professionals to examine patients who suffer from PTSD. This scale assesses the severity of a person’s PTSD symptoms and the impact of PTSD as a whole.
The PTSD Symptom Scale comes in two parts. The first part is a general list of traumatic experiences that a patient might have experienced. The other one is a questionnaire with seventeen items:
- Having upsetting thoughts or images about the traumatic event that come into your head when you do not want them to
- Having bad dreams or nightmares about the traumatic event
- Reliving the traumatic event (acting as if it were happening again)
- Feeling emotionally upset when you are reminded of the traumatic event
- Experiencing physical reactions when reminded of the traumatic event (sweating, increased heart rate)
- Trying not to think or talk about the traumatic event
- Trying to avoid activities or people that remind you of the traumatic event
- Not being able to remember an important part of the traumatic event
- Having much less interest or participating much less often in important activities
- Feeling distant or cut off from the people around you
- Feeling emotionally numb (unable to cry or have loving feelings)
- Feeling as if your future hopes or plans will not come true
- Having trouble falling or staying asleep
- Feeling irritable or having fits of anger
- Having trouble concentrating
- Being overly alert
- Being jumpy or easily startled
If you look at the questions, they focus on certain aspects of experiencing PTSD, like:
- Having thoughts about their traumatic experience(s)
- Reliving memories they have of their traumatic experience(s)
- Avoiding areas or people tied to their traumatic experience(s)
- Being in states of hyperarousal, which could mean they have trouble sleeping and are paranoid (they are jumpy and hypervigilant about something)
While the scale is straightforward and simple, please note that PTSD is a difficult subject for anyone, so you might not get the answers from your patient immediately.
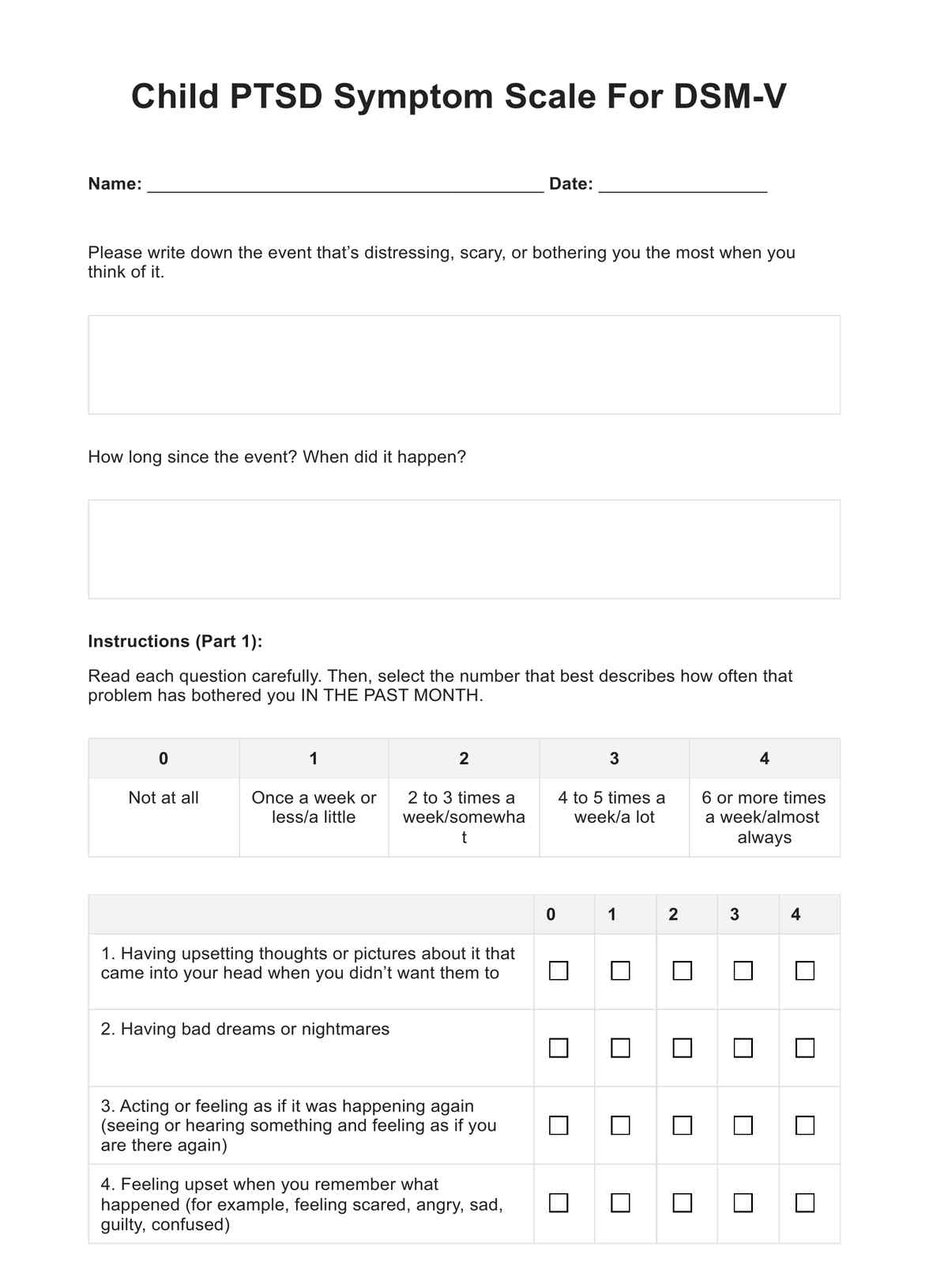
PTSD Symptom Scale Template
PTSD Symptom Scale Example
How to use the PTSD Symptom Scale (PSS)
Administer the scale to your patient.
There are two ways for you to administer this scale to your patient:
- You can administer this like an interview. If you want, you can structure one of your sessions based on the scale and have them answer the items on the spot. You simply have to ask the questions and indicate the answers they can give.
- Give them the scale to answer on their own. This might be the best choice considering PTSD is not something that is easily discussed. The first choice only works if the person is willing to discuss their responses immediately and in person. If they are not, give them the space and comfort they need. Come to an agreement as to when it would be best to hand in the accomplished scale.
Have the patient tick any of the general traumatic experiences that apply to them.
Again, the first section of this PTSD Symptom Scale is a checklist of general traumatic experiences that the patient might have gone through. They simply need to answer Yes or No.
There is also one part where the patient is asked about specific traumatic events they have experienced not included in the list.
If the patient does not say Yes to anything and does not mention a specific traumatic event, then they don’t need to complete the list given that this is for those who have experienced traumatic events.
After the list of traumatic experiences, the patient needs to answer the following questions with Yes or No:
- Were you physically injured?
- Was someone else physically injured?
- Did you think your life was in danger?
- Did you think someone else’s life was in danger?
- Did you feel helpless?
- Did you feel terrified?
Answer the 17-item list.
The next part is the seventeen-item list that we mentioned earlier. All the patient needs to do is rate each of the prompts with the following:
- 0 = “Not at all”
- 1 = “Once per week or less / a little bit / one in a while”
- 2 = “2 to 4 times per week / somewhat / half the time”
- 3 = “3 to 5 or more times per week / very much / almost always”
After that, there is a checklist to tick. They simply need to tick what aspects of their life have been affected by their PTSD.
Determine what to do next after receiving a fully-accomplished scale.
Once you receive a fully-accomplished scale, all you need to do is to tally the scores. The maximum score that a person can get is 51, with higher scores meaning higher severity levels of PTSD symptoms.
There is no score range or designations to work with, so your decisions will be based on not just the total score, but also their ratings per item. Do you need to have your patient undergo more comprehensive assessments? Do you have enough information to work on a treatment plan at this point? These are just two of the questions that you’ll get an answer to after receiving a fully-answered scale.
When does one typically administer the PTSD Symptom Scale (PSS)?
Given the purpose of this instrument, the PTSD Symptom Scale (PSS) is normally administered whenever a patient starts seeing a professional after going through a traumatic experience.
However, before you administer this, you need to gauge if the patient has had enough time to process what they have been through. If you are wondering why you should hold off using this immediately, issuing it to a patient who hasn’t fully processed their experience runs the risk of overestimating the severity of their symptoms and leaving out symptoms that may emerge over time.
Once you are sure that the patient has had time to process their traumatic experiences, then feel free to administer the scale to them.
Of course, this scale doesn’t always have to be used for initial appointments. You may reuse this later to check on the severity of symptoms and see if patients are getting better or worse over time, especially if they are already undergoing a treatment plan.
Who can use this PTSD Symptom Scale (PSS)?
The PTSD Symptom Scale (PSS) can be used by the following healthcare professionals:
- (Clinical) Psychologists
- Psychiatrists
- Counselors
- (Mental Health) Therapists
So long as the healthcare professional is highly-trained and specializes in treating patients who suffer from PTSD, they can definitely use this scale for their work. Though, it is important to note that the PTSD Symptom Scale is not a diagnostic tool. It was created to assess the level of severity of PTSD symptoms in a patient who experienced something traumatic. If you are a healthcare professional who deals with patients with PTSD but are not equipped to make an official diagnosis, please make sure to pass them on to someone who is more equipped to do so.

What are the benefits of using the PTSD Symptom Scale (PSS)?
The scale is, more or less, easy to answer.
The scale is, more or less, simple and straightforward to answer. Most of the questions have Yes and No responses and the scale proper just requires patients to pick a number between 0 to 3 based on which one applies to them the most per item.
The scale is a good tool when it comes to researching populations.
The scale is not just meant to be used in a clinical setting. The PTSD Symptom Scale (PSS) can be used to assess PTSD for people who have gone through certain experiences like survivors of sexual assault, survivors of murder attempts, and veterans who were sent to war.
The scale can be used to track similarities between people within certain populations and observe any commonalities when it comes to symptoms.
It can also be used to create tailor-fitted plans.
The PTSD Symptom Scale (PSS) can be used to help professionals develop treatment plans for patients when they have already undergone comprehensive assessments and have been diagnosed with PTSD. Just make sure that the treatment plan is tailor-fitted to the patient since how they grapple with PTSD may be different from another person, so general treatment plans may not always be the best choice.
It also serves as a monitoring tool.
After implementing a treatment plan, you are surely looking forward to it working and helping the patient. But how can one truly know that? You can simply reissue the PTSD Symptom Scale (PSS) every now and then to monitor your patient’s progress. Are their PTSD symptoms becoming more manageable or not? What part of your plan needs some improvement? These are two of the questions you can answer if you reuse this scale.
Commonly asked questions
It shouldn’t take longer than 10 minutes, but of course, considering the subject matter, don’t be surprised if it takes too long. The important thing is your patient is able to finish answering it. To help them do that, give them the time and space they need to do so.
Yes. The only thing you need to know is that the higher the score your patient has, the more likely it is that their symptoms of PTSD are more severe. If you want, you may even use other related assessments to give you a more well-rounded perspective on the matter.
Yes, but under no circumstance should you diagnose yourself or make any medical-related decisions in relation to whatever result you get, save for seeing an actual professional. This is also a screening tool, not a diagnostic tool.


















-template.jpg)