A Primary Trauma Survey (PTS) is an immediate, systematic assessment protocol designed to identify and address life-threatening injuries in trauma patients as soon as they arrive at the emergency department. These injuries commonly include cardiac tamponade, tension pneumothorax or airway obstruction.
Primary Trauma Survey
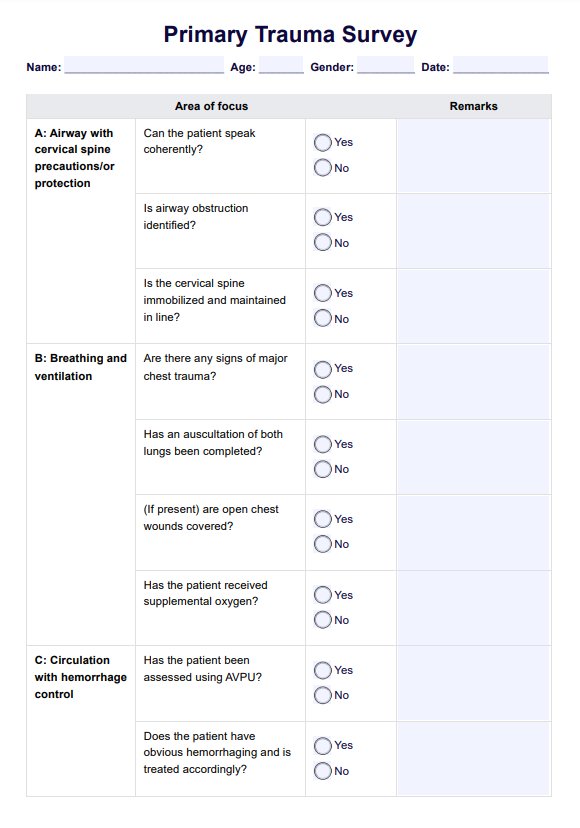
Learn how to perform a Primary Trauma Survey to identify areas requiring immediate physical trauma intervention and stabilize the patient's condition.
Use Template
Primary Trauma Survey Template
Commonly asked questions
A PTS should be performed immediately upon a trauma patient's arrival to the emergency department before any detailed history taking or secondary examination.
Rapid assessment is crucial because life-threatening injuries require immediate intervention to stabilize the patient and prevent further harm or death.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











