Insomnia Severity Index
Access the Insomnia Severity Index to aid in diagnosing and managing sleep issues effectively.


What is the Insomnia Severity Index (ISI)?
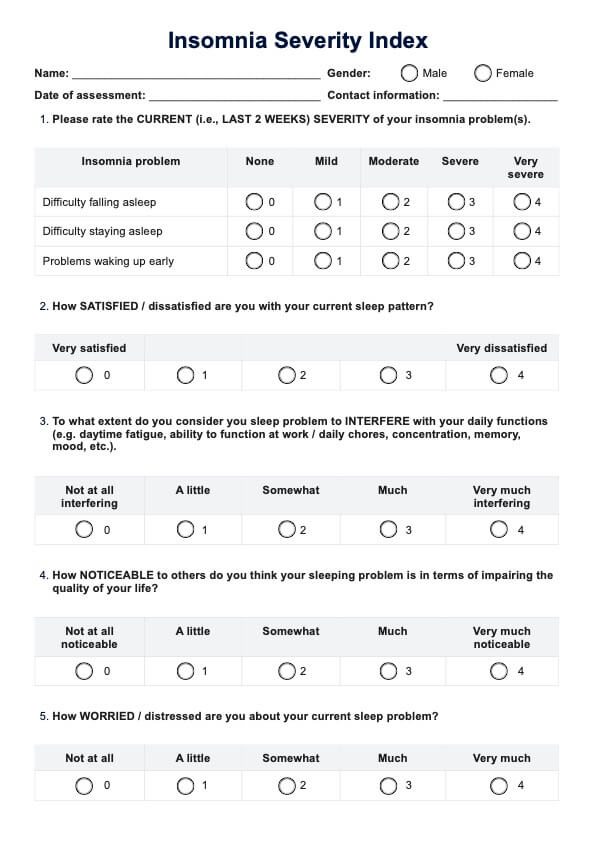
The Insomnia Severity Index (ISI) is a 7-item self-report questionnaire that evaluates insomnia’s nature, severity, and impact over the past month. It assesses several dimensions of sleep disturbances, including difficulty falling asleep, staying asleep (wake after sleep onset), and waking up too early. The ISI is also used to evaluate sleep disorders.
The ISI also measures sleep dissatisfaction, the interference of sleep problems with daytime functioning, the noticeability of sleep issues by others, and the distress caused by these sleep difficulties.
Psychometric studies have demonstrated the ISI’s ability to detect insomnia cases and evaluate treatment responses. In a community population-based sample, a cutoff score of 10 had 86.1% sensitivity and 87.7% specificity for identifying insomnia. The ISI also shows good internal consistency (Cronbach’s α = 0.90-0.91) and correlates well with sleep diaries, polysomnography, and clinical interviews (Morin et al., 2011).
The ISI has been validated in various populations, including English, Spanish, French, Arabic, Hindi, German, Korean, Chinese, and other languages. It is available in patient, clinician, and significant other versions, though the patient self-report form is most commonly used. The ISI is a widely used instrument for screening and monitoring treatment outcomes in insomnia research and clinical practice.
How is the index scored and how are the results interpreted?
Using a 5-point Likert scale (0 = no problem to 4 = very severe problem), each of the seven items yields a total score ranging from 0 to 28. Here's how to interpret the total scores in this assessment of insomnia:
- 0–7: No clinically significant insomnia
- 8–14: Subthreshold insomnia
- 15–21: Moderate insomnia
- 22–28: Severe insomnia
Next steps after using this index
After administering the ISI, interpret scores to detect cases of insomnia and determine severity using the original ISI cutoff scores. Additional moderate to severe insomnia assessments, such as a self-report questionnaire assessing sleep onset latency and the Pittsburgh Sleep Quality Index, should be considered. Evaluating poor sleep quality using additional tools can provide valuable insights into sleep disturbances.
Discuss results with the patient to develop a treatment plan, which may include therapy, medication for persistent insomnia, and addressing sleep maintenance and early morning awakenings. Track progress using valid instruments and aim for an 8.4-point (95 CI) improvement in ISI scores, indicating reduced insomnia symptoms.
Consider a possible history of insomnia and be vigilant for comorbid conditions like sleep apnea. Early detection and intervention are crucial, as insomnia often remains unrecognized and untreated.
Insomnia Severity Index Template
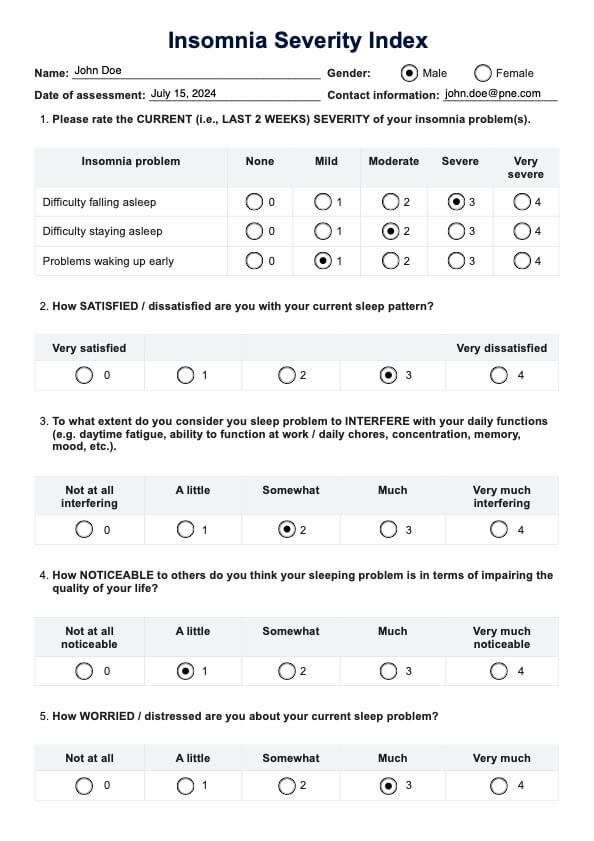
Insomnia Severity Index Example
How to use our Insomnia Severity Index template
Download our Insomnia Severity Index (ISI) Template to easily assess and track insomnia in your patients. Our user-friendly template allows you to fill in patient responses and calculate the total ISI score to determine insomnia severity. This tool leverages psychometric indicators to detect insomnia with high sensitivity and specificity. It accounts for latency, wake after sleep, and is validated across community and clinical samples as well as population-based samples. Streamline your workflow and ensure consistent, accurate assessments of insomnia.
How this index benefits mental health professionals
Understanding and addressing sleep issues is crucial for mental health professionals. It is also important to assess for psychiatric disorders, such as mood and anxiety disorders, in patients with insomnia. The Insomnia Severity Index is a valuable tool that offers numerous benefits in the clinical setting.
- Standardized assessment: The ISI provides a standardized method for evaluating insomnia, ensuring consistent and reliable measurement across different patients and settings. This helps compare data accurately, facilitating better diagnosis and treatment planning.
- Evidence-based tool: The ISI has robust psychometric properties, making it an evidence-based tool validated in various clinical and community samples. Its proven reliability and validity enhance the confidence of mental health professionals in using it as part of their assessment toolkit.
- Treatment monitoring: The ISI is a diagnostic tool and an effective way to monitor changes in insomnia severity over time. This monitoring capability allows professionals to evaluate the treatment response in clinical interventions and adjust them as needed, ensuring that patients receive the most effective care.
- Enhanced patient communication: The ISI facilitates better patient communication about sleep issues. It helps structure more informed discussions and collaborative treatment planning, empowering patients to take an active role in their own care.
Incorporating the ISI into clinical practice can significantly enhance the quality of care provided to patients suffering from insomnia, ultimately leading to better outcomes and improved overall well-being.
References
Morin, C. M., Belleville, G., Bélanger, L., & Ivers, H. (2011). The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep, 34(5), 601–608. https://doi.org/10.1093/sleep/34.5.601
Sadeh, A. (2011). The role and validity of actigraphy in sleep medicine: An update. Sleep Medicine Reviews, 15(4), 259–267. https://doi.org/10.1016/j.smrv.2010.10.001
Commonly asked questions
The ISI is primarily designed for adults but can be adapted for adolescents under clinical guidance.
While the ISI is valuable for assessing insomnia severity, it should not be used as a standalone diagnostic tool. Clinical judgment and additional assessments are necessary for a comprehensive diagnosis.
The ISI can be administered at regular intervals (e.g., monthly) to monitor changes in insomnia severity and evaluate treatment effectiveness.
Global improvement ratings obtained from an independent assessor are used to compare change scores in participants before and after treatment. These ratings help quantify minimally important changes in relation to treatment response.

.jpg)




















-template.jpg)














































































