Various factors, including family history or genetic predisposition, neurological issues, and life events, can cause hypomania. It is commonly associated with bipolar II disorder but can also be triggered by medications, sleep deprivation, or recreational drug use.
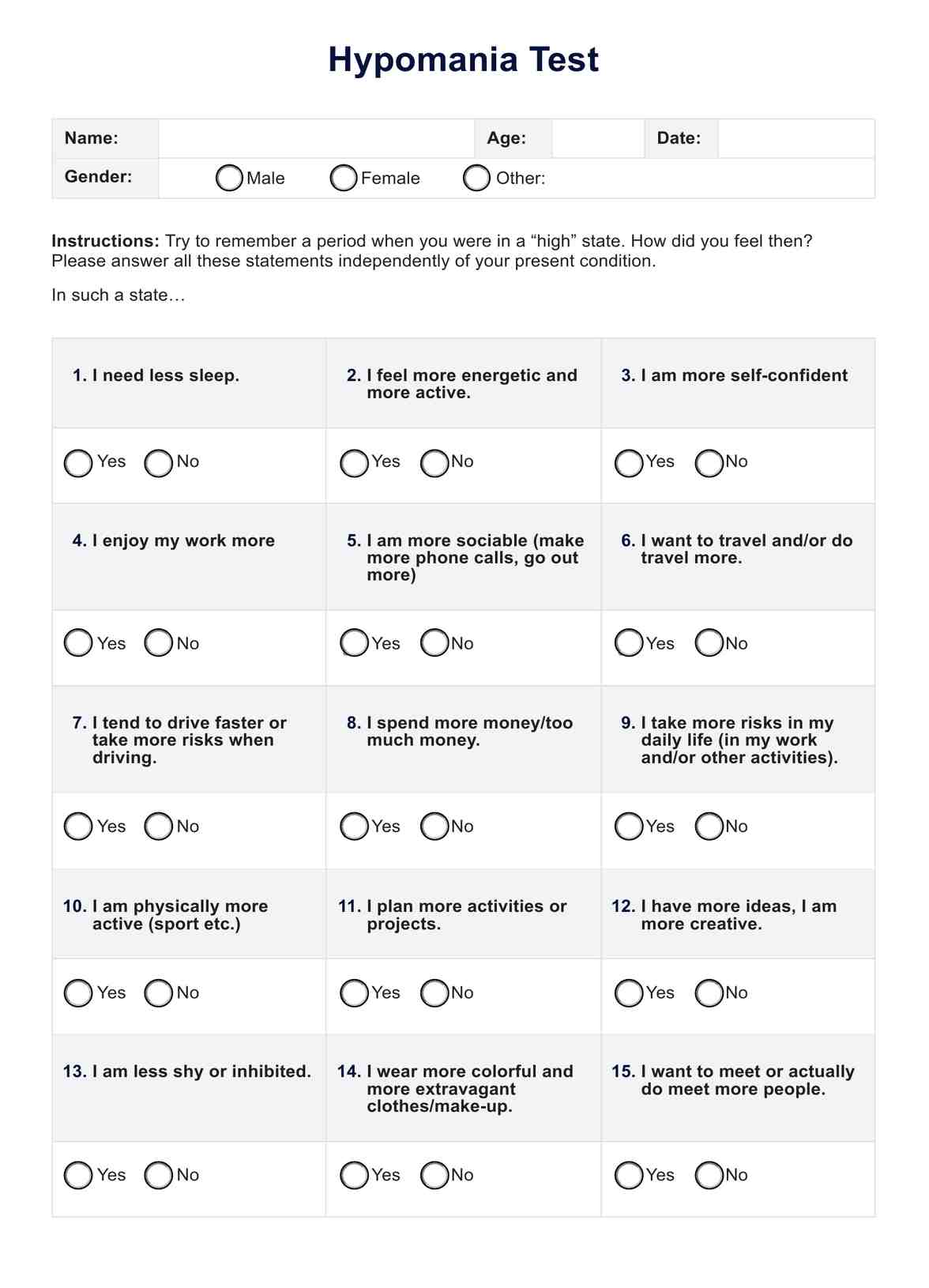
Hypomania Test
Explore using the Hypomania Test as an initial screening tool for possible presentations of hypomanic symptoms. Download your free PDF here.
Hypomania Test Template
Commonly asked questions
Treatment may include medication, such as mood stabilizers or antipsychotics, and psychotherapy. Strategies like cognitive-behavioral therapy (CBT) can help manage symptoms and develop coping mechanisms. Lifestyle changes and monitoring can also be part of a comprehensive treatment plan.
Hypomania differs from mania in its severity and impact. While both involve elevated or irritable moods, mania is more intense and often results in significant problems in work or social functioning, sometimes requiring hospitalization. Hypomania does not cause significant social or occupational impairment and lacks psychotic features.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











