Factitious Disorder DSM-5 Criteria
Read our guide to learn more about the DSM-5 criteria for diagnosing factitious disorder, its symptoms, types, and treatment options.


What is factitious disorder?
Factitious disorder, also known as Munchausen syndrome, is a mental disorder characterized by the intentional falsification of medical or psychological symptoms in oneself or others without obvious external rewards. It is a type of somatic symptom disorder in the Diagnostic and Statistical Manual of Mental Disorders. Symptoms can range from exaggerating symptoms to inducing actual harm. The irony lies in that patients suffering from personality disorders like these seek treatment yet actively try to hide their disorder.
There are two main types: Factitious disorder imposed on self and factitious disorder imposed on another (previously known as factitious disorder by proxy). In the first type, individuals present themselves as ill or injured. In the second type, individuals falsely present another person, often a child, as ill or injured.
This disorder is associated with severe psychological distress and significant functional impairment, affecting not only the individual but also their family, friends, and healthcare providers.
Factitious Disorder DSM-5 Criteria Template
Factitious Disorder DSM-5 Criteria Example
How is factitious disorder diagnosed?
Diagnosing factitious disorder involves a meticulous process due to its deceptive nature. Healthcare professionals follow these steps:
- Clinical evaluation: Conduct a thorough patient history and physical examination to identify inconsistencies between reported and observed symptoms.
- Review of medical records: Examine past medical records for evidence of frequent hospitalizations, multiple medical procedures, or treatments at various facilities without conclusive diagnoses.
- Behavioral observations: Monitor the patient's behavior for signs of deceit, such as exaggeration of symptoms, tampering with medical equipment, or self-inflicted injuries.
- Psychological assessment: Conduct interviews and standardized psychological tests to assess the patient's mental state and rule out other mental disorders.
- Laboratory tests and imaging: Utilize diagnostic markers such as blood tests and imaging studies to confirm or refute the presence of reported medical conditions.
- Differential diagnosis: Differentiate factitious disorder from other conditions, including:
- Malingering: Involves symptom fabrication for external rewards (e.g., financial gain).
- Somatic symptom and related disorders: Excessive focus on symptoms without intentional deception.
- Functional neurological symptom disorder (conversion disorder): Symptoms inconsistent with medical conditions but without deceit.
- Borderline personality disorder: May involve self-harm without deception.
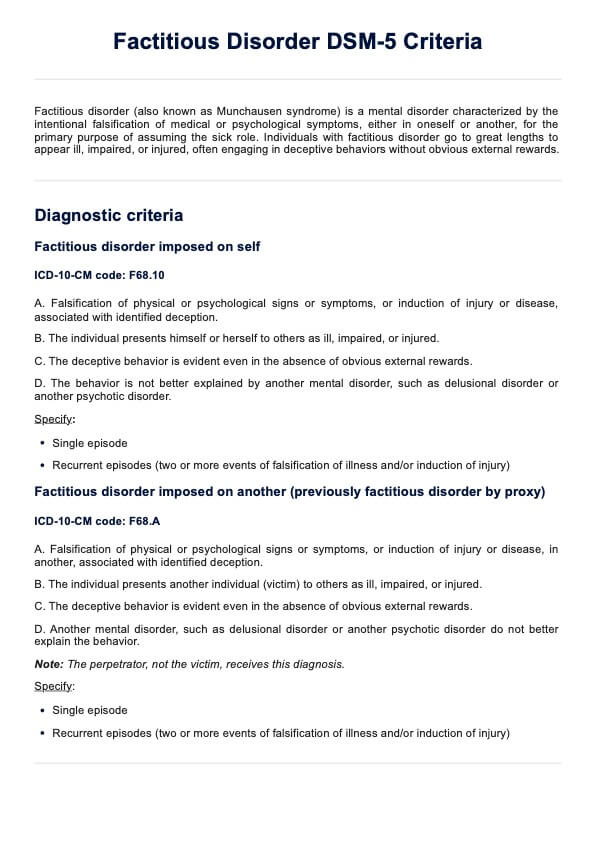
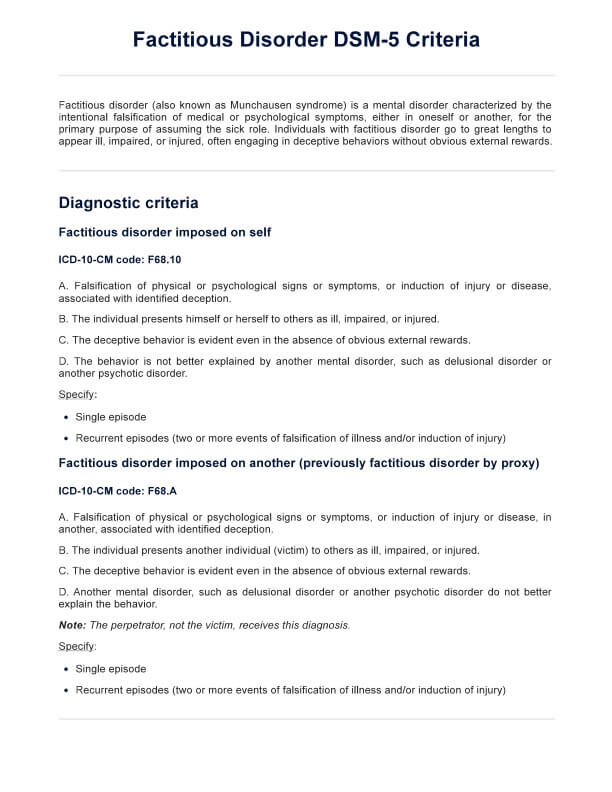
Factitious disorder DSM-5 diagnostic criteria
Here are the diagnostic criteria for the two types:
Factitious disorder imposed on self
- Criterion A: Falsification of physical or psychological signs or symptoms, or induction of injury or disease, associated with identified deception.
- Criterion B: The individual presents himself or herself to others as ill, impaired, or injured.
- Criterion C: The deceptive behavior is evident even in the absence of obvious external rewards.
- Criterion D: The behavior is not better explained by another mental disorder, such as delusional disorder or another psychotic disorder.
Specify:
- Single episode
- Recurrent episodes (two or more events of falsification of illness and/or induction of injury)
Factitious disorder imposed on another (previously factitious disorder by proxy)
- Criterion A: Falsification of physical or psychological signs or symptoms, or induction of injury or disease, in another, associated with identified deception.
- Criterion B: The individual presents another individual (victim) to others as ill, impaired, or injured.
- Criterion C: The deceptive behavior is evident even in the absence of obvious external rewards.
- Criterion D: The behavior is not better explained by another mental disorder, such as delusional disorder or another psychotic disorder.
Note: The perpetrator, not the victim, receives this diagnosis.
Specify:
- Single episode
- Recurrent episodes (two or more events of falsification of illness and/or induction of injury)
Differences between the DSM-4 and DSM-5 criteria
The criteria for factitious disorder underwent significant changes from DSM-IV to DSM-5. In DSM-IV, factitious disorder was categorized distinctly, with subtypes based on whether the symptoms were predominantly physical or psychological. It also distinguished factitious disorder from malingering, emphasizing that factitious disorder involved intentional falsification without external rewards, while malingering involved falsification for external gains.
In DSM-5, factitious disorder is classified under the broader "somatic symptom and related disorders" category. The distinction between physical and psychological subtypes has been removed, focusing on the overall falsification of symptoms rather than the type. DSM-5 acknowledges that individuals with factitious disorder may receive some form of reward, even if it is not the primary motivation.
Additionally, DSM-5 distinguishes between factitious disorder imposed on self and factitious disorder imposed on another (previously called factitious disorder by proxy). The diagnosis can also be specified as a single episode or recurrent episodes.
How is factitious disorder treated?
Treating and managing factitious disorder is challenging due to the deceptive nature of the condition. While there is no cure, several strategies can help manage the disorder effectively:
- Psychotherapy: Cognitive-behavioral therapy (CBT) is commonly used to address underlying psychological issues, improve coping mechanisms, and reduce deceptive behaviors. Therapy focuses on building a therapeutic alliance, which is crucial for treatment adherence.
- Medication: While no specific medications treat factitious disorder directly, medications can manage associated symptoms such as depression or anxiety. Antidepressants or anxiolytics may be prescribed based on individual needs.
- Medical supervision: Regular, non-punitive medical follow-ups can help monitor the patient's health and prevent unnecessary medical interventions. Establishing a single primary care provider to coordinate care can reduce the risk of excessive medical procedures.
- Family therapy and education: Educating family members about the disorder and involving them in the treatment process can provide support and improve the patient's social environment. Family therapy can help address any familial dynamics contributing to the disorder.
- Multidisciplinary approach: Collaboration among healthcare providers, including psychologists, psychiatrists, primary care physicians, and social workers, ensures a comprehensive treatment plan tailored to the patient's needs.
Effective management requires patience, consistency, and a non-judgmental approach from healthcare professionals. Early intervention and continuous support can significantly improve outcomes for individuals with factitious disorder.
Commonly asked questions
Malingering involves the intentional production of false psychological or physical symptoms for external rewards, such as financial gain or avoiding work, while factitious disorder involves falsification of symptoms without obvious external incentives.
Assessment involves a thorough clinical evaluation, review of medical history, behavioral observations, psychological assessments, and differentiation from other conditions such as malingering or somatic symptom disorders.
Previously, DSM-IV identified three subtypes based on physical or psychological symptoms. However, DSM-5 recognizes two types: factitious disorder imposed on self and factitious disorder imposed on another.


















-template.jpg)



















































































