CBT for sleep, also known as CBT-I, is highly effective and is considered the first-line treatment for chronic insomnia based off , with numerous studies demonstrating its ability to improve sleep quality and efficiency.
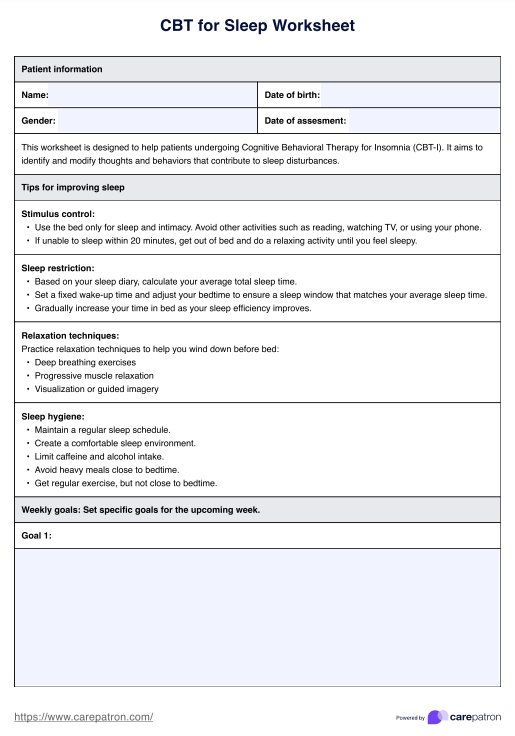
CBT for Sleep Worksheet
Unlock better sleep with our CBT for Sleep Worksheet Template, designed for healthcare professionals to address insomnia and sleep disturbances effectively.
Use Template
CBT for Sleep Worksheet Template
Commonly asked questions
CBT sleep restriction involves limiting the time spent in bed to match the actual sleep time, which helps consolidate sleep and increase sleep efficiency over time.
Cognitive behavioral interventions for treating insomnia and sleep problems focus on identifying and modifying negative thoughts and behaviors that contribute to sleep disturbances, such as poor sleep hygiene, anxiety about sleep, and irregular sleep schedules.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











