BPD Favorite Person Test
Discover more about the BPD Favorite Person Test, along with an example and free PDF download from Carepatron. Learn more about this critical aspect of borderline personality disorder.


What is Borderline personality disorder?
Borderline Personality Disorder (BPD) is a complex mental health condition characterized by pervasive patterns of instability in interpersonal relationships, self-image, and emotions. Individuals with BPD often experience intense and fluctuating emotions, which can lead to difficulties in regulating their feelings and behaviors.
One of the hallmark features of BPD mental health disorders is the presence of unstable relationships, marked by alternating idealization and devaluation of others. This can result in a fear of abandonment and efforts to avoid real or perceived rejection, leading to tumultuous interpersonal dynamics.
Additionally, individuals with BPD may struggle with a fragmented sense of self, experiencing rapid shifts in self-image, identity, and goals. This instability can manifest in chronic feelings of emptiness and a lack of direction in life.
The emotional intensity experienced by those with BPD can be overwhelming and may result in impulsive behaviors such as substance abuse, self-harm, or suicidal gestures. These behaviors often serve as maladaptive coping mechanisms to manage distressing emotions.
Diagnosing Borderline Personality Disorder typically requires a comprehensive evaluation by a licensed mental health professional, such as a psychiatrist or psychologist. There isn't a single definitive borderline personality disorder test; instead, clinicians assess various symptoms and criteria outlined in diagnostic manuals like the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
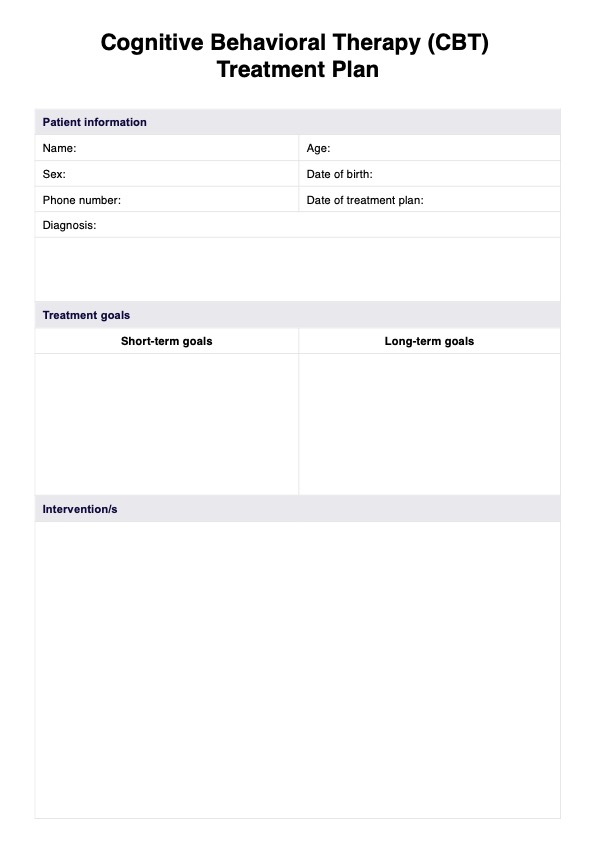
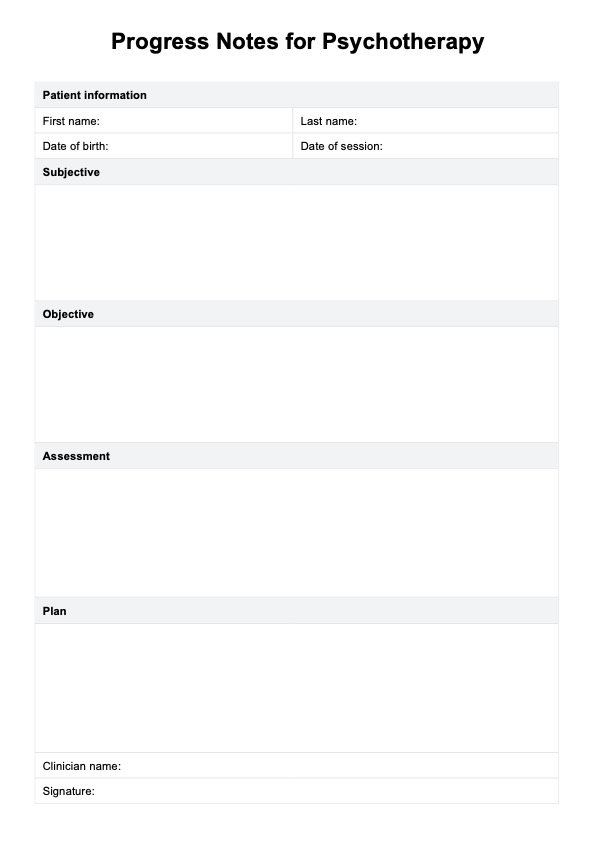
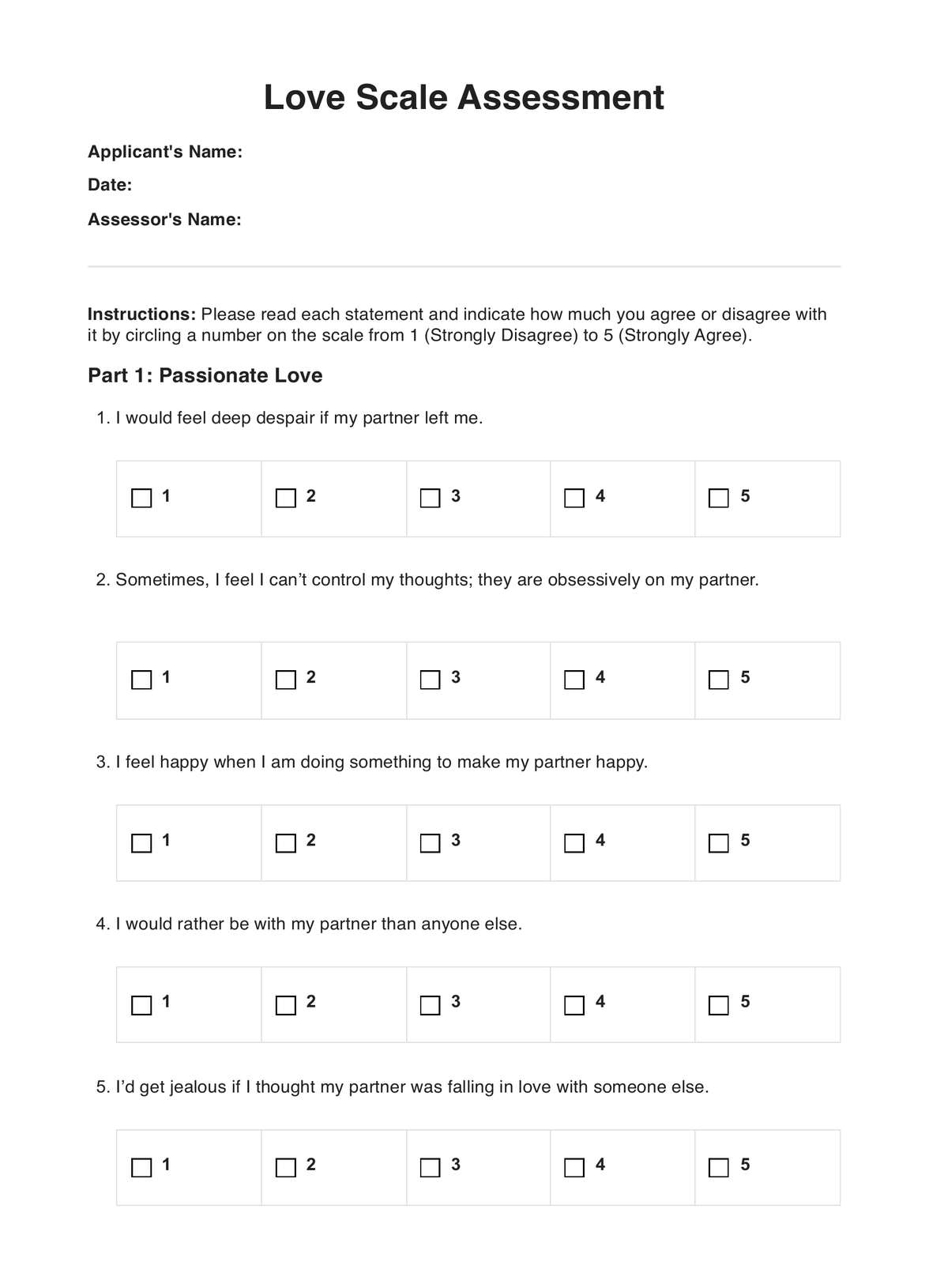
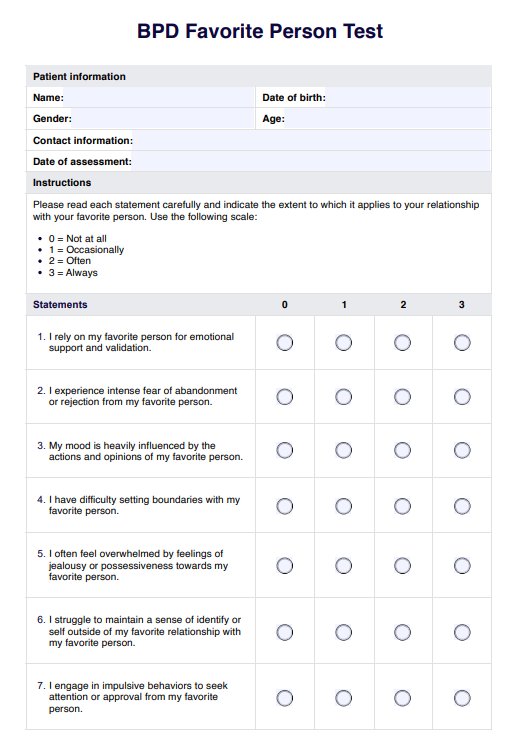
BPD Favorite Person Test Template
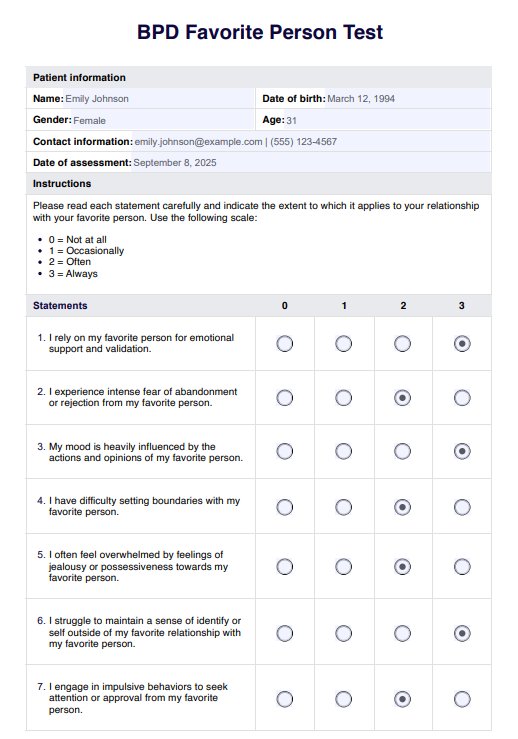
BPD Favorite Person Test Example
BPD symptoms
Borderline Personality Disorder (BPD) manifests through a variety of symptoms that can significantly impact an individual's daily life and relationships. Below are some of the key symptoms associated with BPD:
Intense and unstable relationships
People with BPD often struggle with maintaining stable and healthy relationships. They may idealize others one moment and devalue them the next, leading to a pattern of unstable interpersonal dynamics.
Distorted self-image
Individuals with BPD may have an unstable sense of self, leading to uncertainty about their identity, values, and goals. This instability can contribute to feelings of emptiness and a lack of direction in life.
Fear of abandonment
A pervasive fear of abandonment is common among those with BPD. They may go to great lengths to avoid real or perceived abandonment, even if it means engaging in destructive behaviors or clinging to unhealthy relationships.
Impulsive behavior
People with BPD often engage in impulsive behaviors that can have harmful consequences. This may include reckless driving, substance abuse, binge eating, or reckless spending.
Emotional instability
Emotional volatility is a hallmark feature of BPD. Individuals may experience intense and rapidly shifting emotions, such as anger, sadness, or anxiety. External events or internal stressors can trigger these mood swings.
Suicidal ideation and self-harm
Individuals with BPD are at increased risk of suicidal ideation and self-harming behaviors. These behaviors may serve as maladaptive coping mechanisms to alleviate emotional distress or communicate inner pain.
Chronic feelings of emptiness
Many people with BPD experience chronic feelings of emptiness or a profound sense of inner void. This pervasive emptiness can contribute to a sense of existential despair and difficulty finding meaning in life.
Difficulty regulating emotions
Individuals with BPD often struggle with regulating their intense emotions effectively. They may experience intense emotional reactions that are disproportionate to the situation, making it challenging to maintain stable and healthy relationships.
How to diagnose borderline personality disorder?
Diagnosing BPD involves a comprehensive assessment by a licensed mental health professional. Below are the steps typically involved in the diagnostic process:
Initial evaluation
The diagnostic process of this mental health condition usually begins with an initial evaluation conducted by a licensed mental health professional, such as a psychiatrist or psychologist. During this evaluation, the clinician will gather information about the individual's medical history, current symptoms, and any previous psychiatric treatment.
Diagnostic criteria
The clinician will then assess whether the individual meets the diagnostic criteria for BPD as outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). This involves identifying patterns of behavior and emotional functioning consistent with BPD, including unstable relationships, identity disturbance, impulsivity, and emotional dysregulation.
Clinical interviews
Clinical interviews are essential for gathering detailed information about the individual's symptoms and history. The clinician may ask about specific experiences, relationships, and behaviors to gain insight into the severity and impact of BPD symptoms on the individual's life.
Differential diagnosis
It's crucial to differentiate BPD from other mental health conditions that may present similar symptoms, such as bipolar disorder, depression, or anxiety disorders. Carefully assessing the individual's symptoms and history helps ensure an accurate diagnosis and appropriate treatment plans.
Collaborative assessment
Sometimes, a collaborative assessment involving input from a family member, friends, or other healthcare providers may help understand the individual's symptoms and functioning. This collaborative approach can provide additional perspectives and insights into the individual's behavior and relationships.
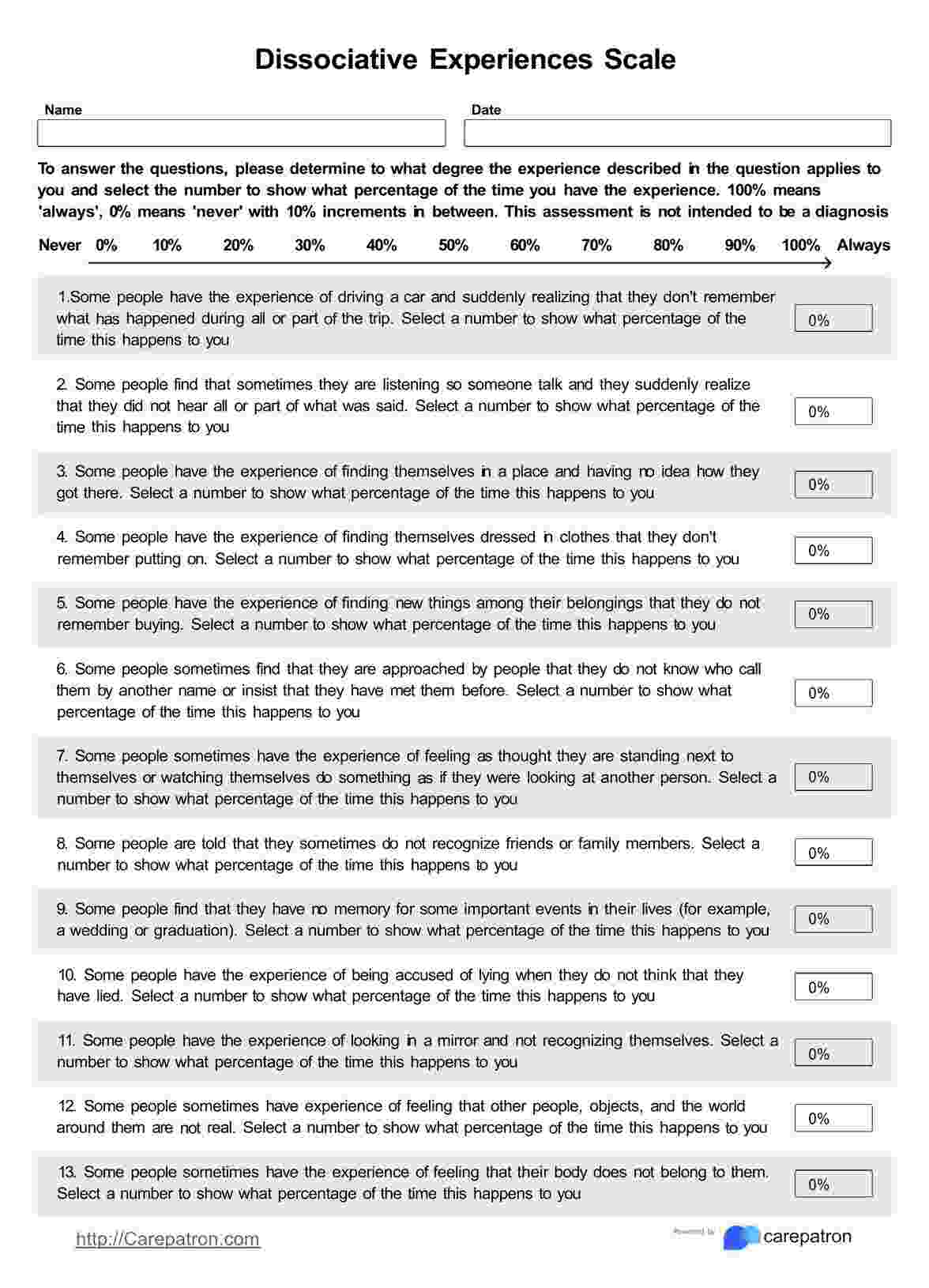
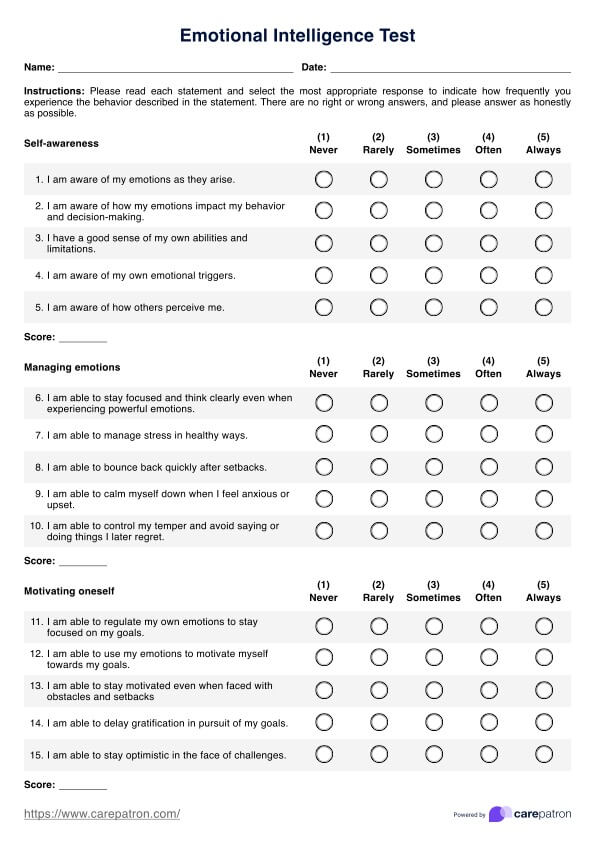
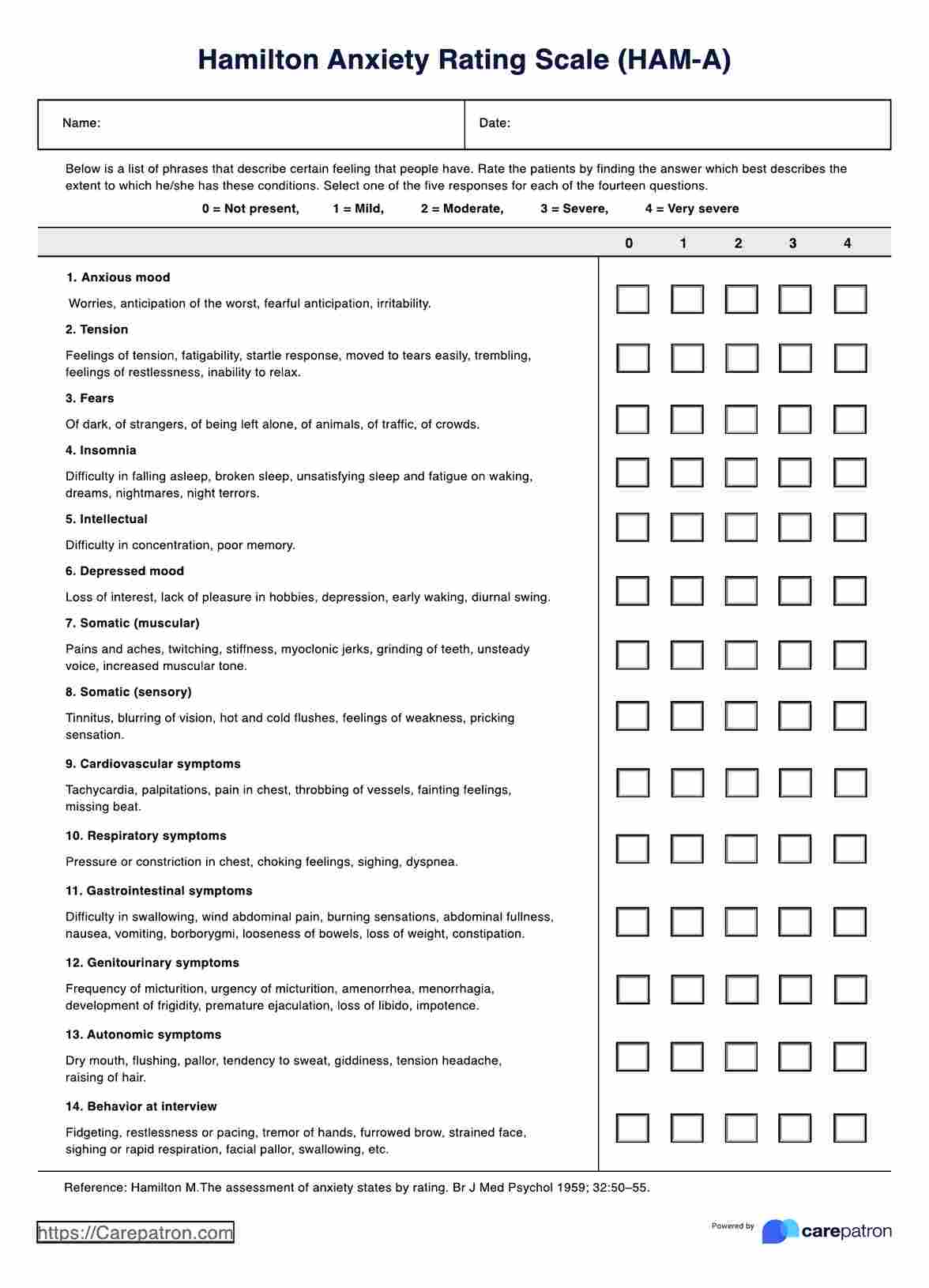
Psychological testing
Psychological testing, such as personality assessments or mood inventories, may supplement the clinical interview and provide further insight into the individual's emotional and cognitive functioning. While there isn't a specific "borderline personality disorder test," these assessments can help support the diagnosis when used in conjunction with clinical evaluation.
What is a BPD favorite person?
In the context of Borderline Personality Disorder (BPD), a "favorite person" refers to an individual whom someone with BPD becomes emotionally reliant on or intensely attached to. This attachment can be characterized by idealization, intense emotional connection, and a strong desire for validation and support from the favorite person.
Individuals with BPD often experience intense emotions and struggle with maintaining stable and healthier relationships. The concept of a favorite person can arise as a coping mechanism to alleviate feelings of emptiness, loneliness, or insecurity. The favorite person BPD relationship may serve as a primary source of emotional support and validation for the individual with BPD.
It's important to note that the designation of someone's favorite person can be both positive and challenging for individuals with BPD and their chosen confidant. While the intense emotional bond may initially feel rewarding and fulfilling, it can also place significant pressure on the favorite person to meet the individual's emotional needs and expectations.
Signs the patient has a favorite person
Recognizing signs that a patient with Borderline Personality Disorder has a favorite person can provide valuable insight into their emotional dynamics and interpersonal relationships. Below are some common indicators that may suggest the presence of a favorite person:
Intense emotional bonding
Individuals with BPD may exhibit an unusually intense emotional connection with someone they designate as their favorite person. This bond often goes beyond typical friendship or familial relationships and may involve feelings of admiration, dependency, and idealization.
Idealization
Patients with BPD may idealize their favorite person, viewing them as perfect or flawless. They may place the individual on a pedestal, attributing qualities or characteristics that exceed reality. This idealization can contribute to a strong desire for validation and approval from the favorite person.
Dependency
A patient with BPD who has a favorite person may display signs of emotional dependency on that individual. They may rely heavily on their favorite person for emotional support, validation, and reassurance, seeking constant contact or reassurance of their worth and value.
Fear of abandonment
Individuals with BPD often experience a pervasive fear of abandonment, which may be particularly pronounced in the context of their relationship with a favorite person. They may go to great lengths to avoid real or perceived rejection or abandonment by their favorite person, exhibiting clingy or possessive behaviors.
Mood instability
The presence of a favorite person can trigger intense mood swings in patients with BPD. They may experience extreme highs when in the presence of their favorite person, followed by profound lows or feelings of emptiness when separated or when the relationship encounters challenges.
Exclusion of others
Patients with BPD may prioritize their favorite person above all others, excluding or neglecting other relationships in their lives. They may become preoccupied with thoughts and fantasies about the favorite person, devoting significant time and energy to maintaining the relationship.
Emotional turmoil
The presence of a favorite person can contribute to emotional turmoil and inner conflict for a person with BPD. They may experience intense jealousy, insecurity, or anxiety in relation to the favorite person, fearing loss or rejection.
How and when to use the template?
Carepatron's BPD Favorite Person Test template is a valuable tool designed to assist medical professionals in assessing and understanding the dynamics of favorite person relationships in patients with Borderline Personality Disorder. Below are guidelines on how and when to use this template effectively:
1. Initial assessment
Medical professionals can use the borderline personality disorder favorite person test template as part of the initial assessment process when evaluating patients suspected of having BPD. By administering the test early on, clinicians can gain insight into the presence and intensity of favorite person relationships, which can inform treatment planning.
2. Ongoing monitoring
The template can also be utilized to monitor the dynamics of the favorite person throughout treatment. Regular administration of the test allows medical professionals to track changes in the patient's relationship patterns and assess the effectiveness of interventions to improve interpersonal functioning.
3. Treatment planning
The information gathered from the BPD Favorite Person Test can inform individualized treatment planning tailored to the patient's specific needs and goals. Medical professionals can use the insights obtained from the test results to develop targeted interventions aimed at addressing issues related to favorite person relationships, such as emotional dependency, fear of abandonment, and instability.
4. Collaborative care
Medical professionals can utilize the template to facilitate collaborative care and communication among multidisciplinary healthcare teams. By sharing the results of the favorite person test with other providers involved in the patient's care, such as therapists, psychiatrists, and social workers, clinicians can ensure a coordinated approach to treatment that addresses all aspects of the patient's well-being.
5. Educating patients
In addition to its clinical utility, the favorite person test can serve as a valuable educational resource for patients with BPD. Medical professionals can use the test as a starting point for discussing favorite person dynamics with patients, helping them gain insight into the impact of these relationships on their mental health and well-being.
6. Flexibility and adaptability
Carepatron's borderline personality disorder favorite person test template offers flexibility and adaptability to suit individual patients' and clinical settings' unique needs. Medical professionals can customize the administration and interpretation of the test based on factors such as the patient's age, cultural background, and presenting symptoms.
Results and next steps
After a patient completes the BPD Favorite Person Test, medical professionals need to interpret the results thoughtfully and collaboratively with the patient. Below are the recommended next steps to take:
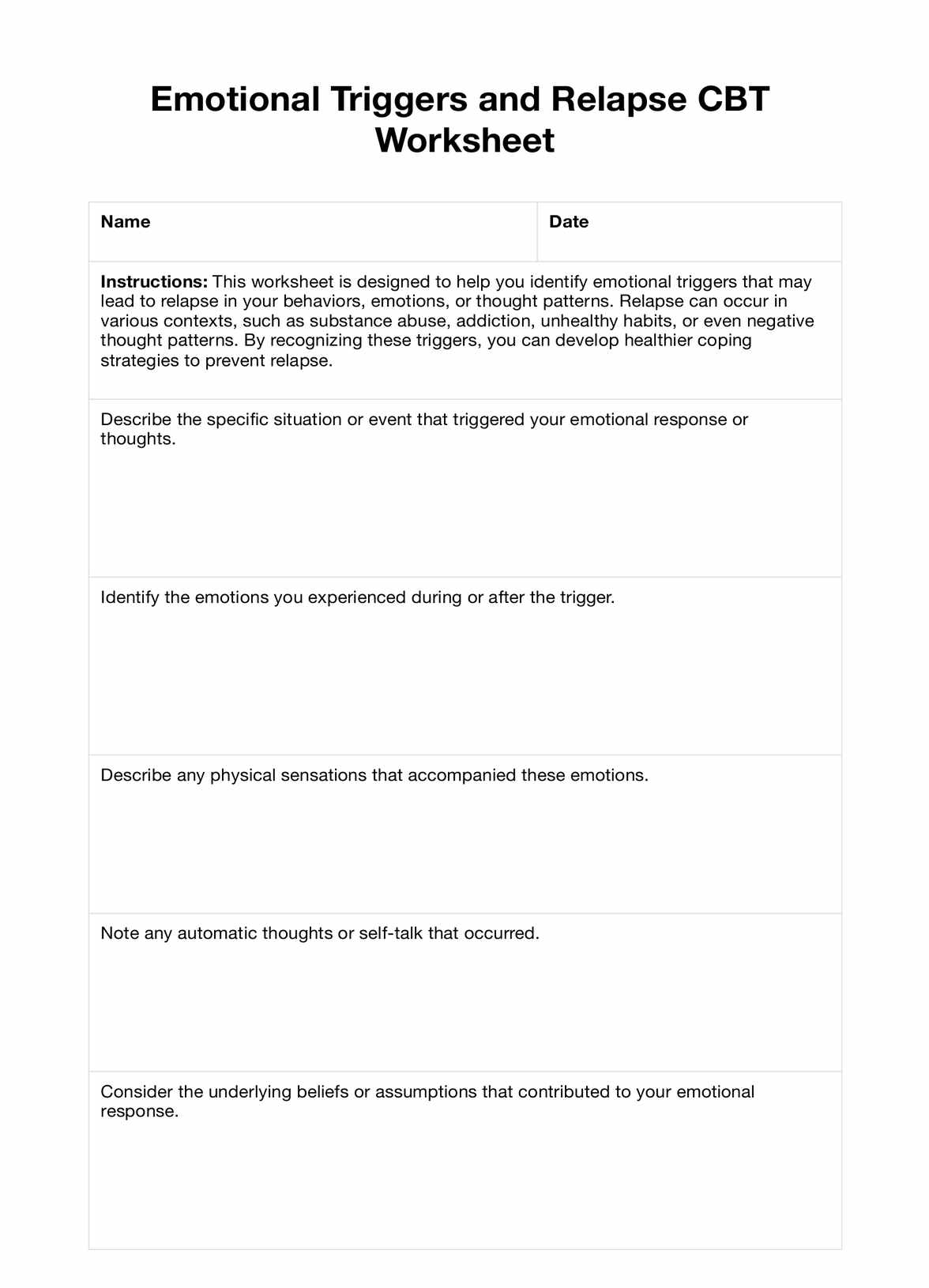
Interpretation of results
Review the test results carefully, considering the patient's responses and any patterns or themes that emerge. Assess the intensity and dynamics of the patient's relationship with their favorite person, including their level of emotional dependency, fear of abandonment, and idealization.
Psychoeducation
Provide psychoeducation to the patient about the significance of favorite person relationships in BPD. Help the patient understand how their attachment to a favorite person may contribute to emotional instability, difficulties in interpersonal relationships, and challenges in maintaining healthy boundaries.
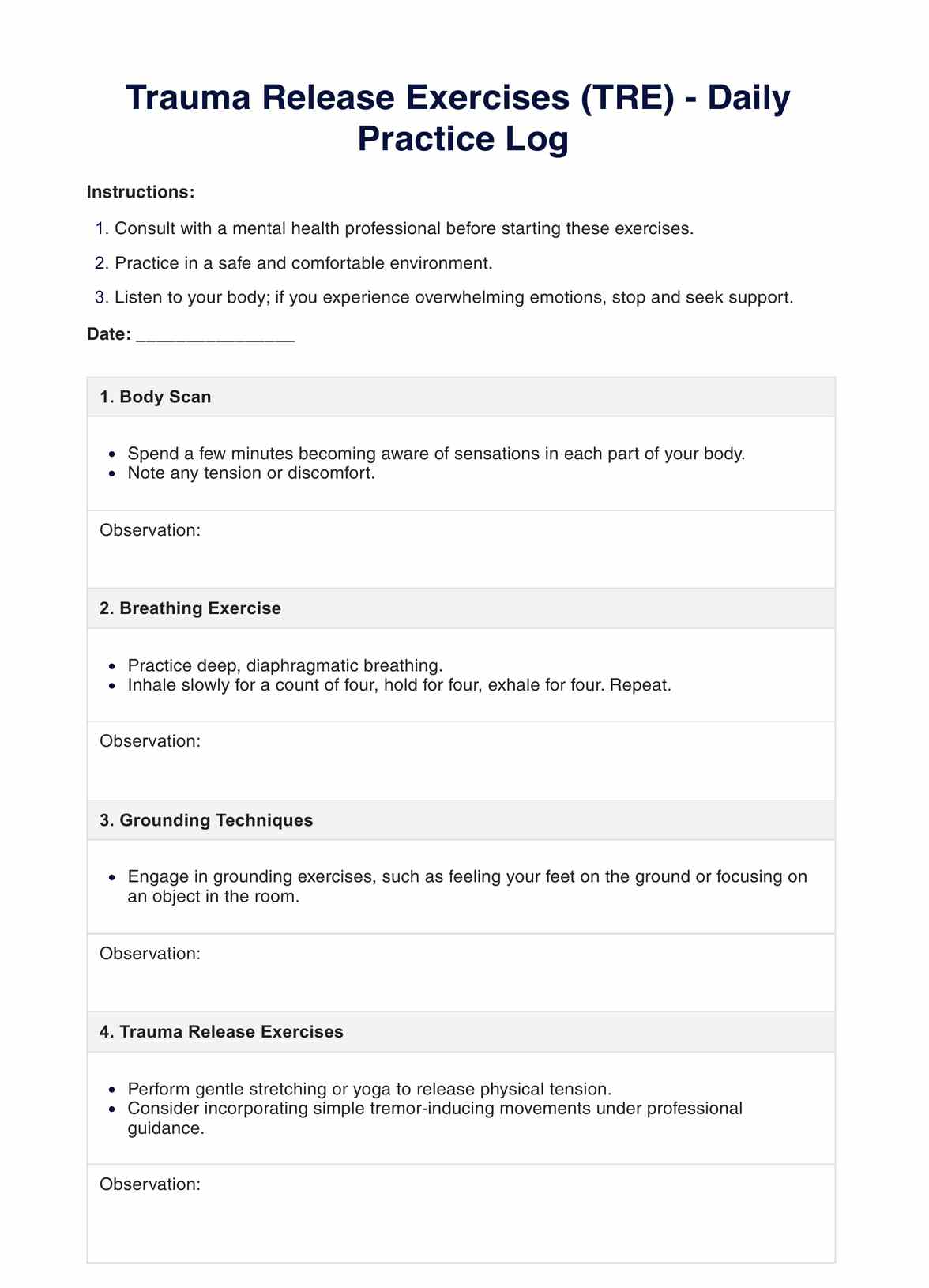
Therapy referral
Refer the patient to individual therapy, ideally with a therapist experienced in treating BPD using evidence-based approaches such as dialectical behavior therapy (DBT). Therapy can help the patient develop coping strategies, regulate emotions, and build healthier relationships, including setting and maintaining boundaries with their favorite person.
Family involvement
If appropriate, involve family members or loved ones in the treatment process, particularly if they play a significant role in the patient's favorite person relationship. Educate family members about BPD and guide how to support the patient in building healthier relationships and improving self-esteem.
Setting boundaries
Collaborate with the patient to establish and maintain healthy boundaries within their relationship with their favorite person. Help patients recognize and communicate their needs and limits effectively, fostering autonomy and self-advocacy.
Developing self-esteem
Work with the patient to address underlying issues contributing to low self-esteem and reliance on external validation. Encourage the patient to engage in activities and practices that promote self-care, self-compassion, and self-empowerment.
How to maintain a healthy BPD favorite person relationship
Maintaining a healthy relationship with their favorite person for someone with BPD requires awareness, communication, and boundary-setting. Here are five key strategies:
1. Establish clear communication
Open and honest communication is vital for maintaining a healthy favorite person relationship. Encourage transparent dialogue about feelings, needs, and boundaries. Foster a supportive environment where both parties feel comfortable expressing themselves without fear of judgment or rejection.
2. Set boundaries
Establishing and respecting boundaries is essential for preserving the integrity of the relationship with their favorite person. Clearly define acceptable and unacceptable behavior, and communicate these boundaries assertively. Encourage the person with BPD to recognize and respect the boundaries of their favorite person, promoting mutual respect and understanding.
3. Practice self-care
Both individuals in the favorite person relationship should prioritize self-care to maintain their emotional well-being. Encourage activities that promote relaxation, stress reduction, and self-compassion. Remind the person with BPD that self-care is essential for maintaining stability and resilience in their relationships.
4. Seek support
Encourage the person with BPD to seek support from a therapist or support group specializing in personality disorders. Therapy can provide valuable skills and strategies for managing emotions and maintaining healthy relationships. Family members or loved ones can also seek support to better understand and support their loved one with BPD in the favorite person relationship.
5. Focus on mutual growth
Foster an environment of mutual growth and development within the favorite person relationship. Encourage both parties to support each other's personal and emotional growth. Emphasize the importance of learning from challenges and conflicts in the relationship, using them as opportunities for growth and understanding.
Why use Carepatron as your mental health software?
Carepatron offers a comprehensive suite of tools and resources tailored to the unique needs of mental health professionals and their clients. With features ranging from mental health software to psychologist practice management tools, Carepatron stands out as the premier platform for those working in mental health. Here's why:
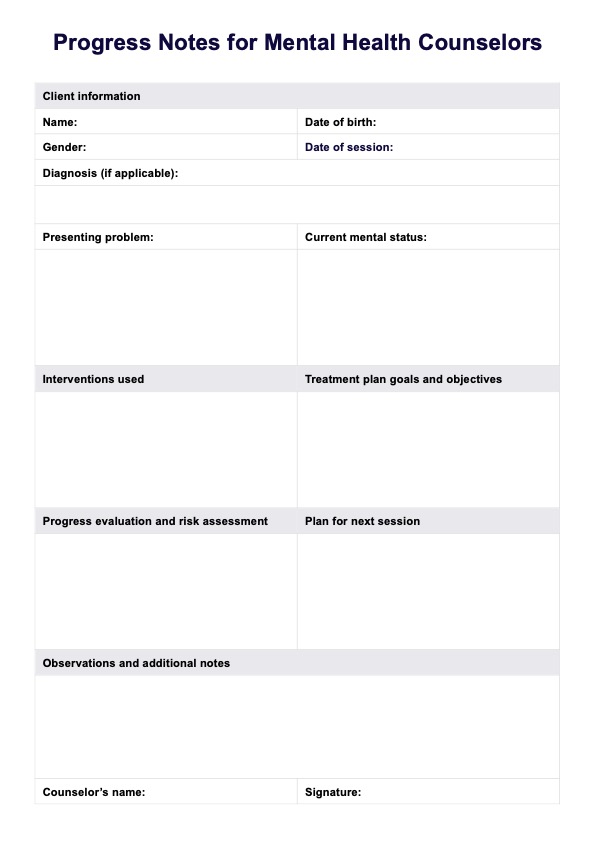
Mental health software
Carepatron's mental health software provides a user-friendly and intuitive platform for managing patient records, scheduling appointments, and documenting treatment progress. With customizable templates and secure data storage, mental health professionals can streamline their workflow and focus on providing quality care to their clients.
Mental health resources
In addition to software solutions, Carepatron offers a wealth of mental health resources to support clinicians and clients. From educational materials and self-help guides to therapeutic tools and exercises like checklists and worksheets, Carepatron empowers individuals to take control of their mental well-being and access the resources they need to thrive.
Psychologist practice management software
Carepatron's psychologist practice management software simplifies the administrative tasks of running a mental health practice. From billing and invoicing to client communication and progress tracking, Carepatron helps psychologists and therapists efficiently manage their practice while maintaining compliance with industry standards and regulations.
Let us help you with the administrative processes, so you can focus on the work that matters. Download Carepatron today for free!
.png)
Commonly asked questions
Losing their favorite person can trigger intense emotional distress, including feelings of abandonment, emptiness, and despair. They may experience heightened mood swings, impulsivity, and a sense of identity disturbance.
BPD symptoms typically peak in early adulthood, with most individuals experiencing the highest intensity of symptoms in their late teens to early twenties.
The notion of a life expectancy of 27 for individuals with BPD is a myth. While BPD can impact the quality of life and increase risk factors for certain health conditions, there is no specific life expectancy associated with the disorder.


















-template.jpg)