Substance-Induced Psychosis DSM 5
Learn about substance/medication-induced psychotic disorder, its symptoms, diagnosis, DSM-5 criteria, treatment, and how Carepatron can help.


What is substance-induced psychosis?
Substance-induced psychosis is the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV) name for what is now known as substance/medication-induced psychotic disorder in the fifth edition (DSM-5). It is characterized by the presence of delusions and/or hallucinations caused directly by the physiological effects of a substance or medication. As such, it is not a primary psychosis, but rateher a secondary or substance-induced psychosis. It also differs from substance use disorder in that substance use disorder is about the problematic pattern of use, while substance/medication-induced psychotic disorder is about the psychotic effects caused by using the substance.
The symptoms of this mental illness include seeing or hearing things that aren't there (hallucinations) and holding false beliefs despite clear evidence to the contrary (delusions). These symptoms typically develop during or soon after substance intoxication or withdrawal, or after exposure to a medication.
The disorder can be diagnosed when these symptoms arise in connection with medication use or substance abuse. The causes include a variety of substances such as alcohol, cannabis, hallucinogens, inhalants, sedatives, hypnotics, anxiolytics, stimulants, and certain medications like anticholinergics, anticonvulsants, and corticosteroids.
The consequences of substance/medication-induced psychotic disorder can be severe, often leading to significant distress and impairment in social, occupational, or other important areas of functioning. This condition is frequently comorbid with substance use disorders and other psychiatric conditions, complicating diagnosis and treatment.
Substance-Induced Psychosis DSM 5 Template
Substance-Induced Psychosis DSM 5 Sample
How to diagnose substance/medication-induced psychosis?
Diagnosing this disorder involves a comprehensive evaluation, typically during or soon after the psychosis. Here are the steps involved:
- Clinical interview: Obtain a detailed history of substance use, including type, amount, and duration. Assess the timeline of symptom onset in relation to substance use.
- Physical examination: Conduct a thorough physical examination to rule out other medical conditions that could cause psychotic symptoms.
- Laboratory tests and diagnostic markers: Perform laboratory tests to detect the presence of substances in the body and assess relevant blood levels, such as blood alcohol levels, which can help confirm substance use and its possible role in psychosis.
- DSM-5 criteria evaluation: Verify that symptoms of delusions and/or hallucinations developed during or soon after substance intoxication or withdrawal and that the substance or medication involved is capable of producing these symptoms.
- Differential diagnosis: Try to rule out other disorders:
- Substance intoxication or withdrawal: If patients know that their altered perception is a result of being intoxicated with stimulants, cannabis, the opioid meperidine, or phencyclidine or withdrawal from alcohol or sedatives, then it is not a substance-induced psychotic disorder. Instead, it is just diagnosed as substance intoxication or substance withdrawal, with perceptual disturbances. There are also caveats for flashback hallucinations, withdrawal delirium, and delusions in the context of a major or mild neurocognitive disorder; all of these are explicitly outlined in the template.
- Independent psychotic disorder: Considered if psychotic symptoms persist for a substantial period after cessation of substance use or if there is a history of recurrent psychotic episodes independent of substance use.
- Psychotic disorder due to another medical condition: Diagnosed if the psychotic symptoms are better explained by a medical condition or a primary psychosis rather than drug use.
- Other mental disorders: Includes disorders where psychotic symptoms are not limited to delusions or hallucinations, such as disorganized speech or behavior, such as bipolar disorder induced by substance use.
Differential diagnosis is essential to distinguish drug-induced psychosis from primary psychotic disorders such as schizophrenia, schizoaffective disorder, and mood disorders with psychotic features. It is also important to rule out psychotic disorder due to another medical condition and delirium to ensure accurate diagnosis and appropriate treatment.
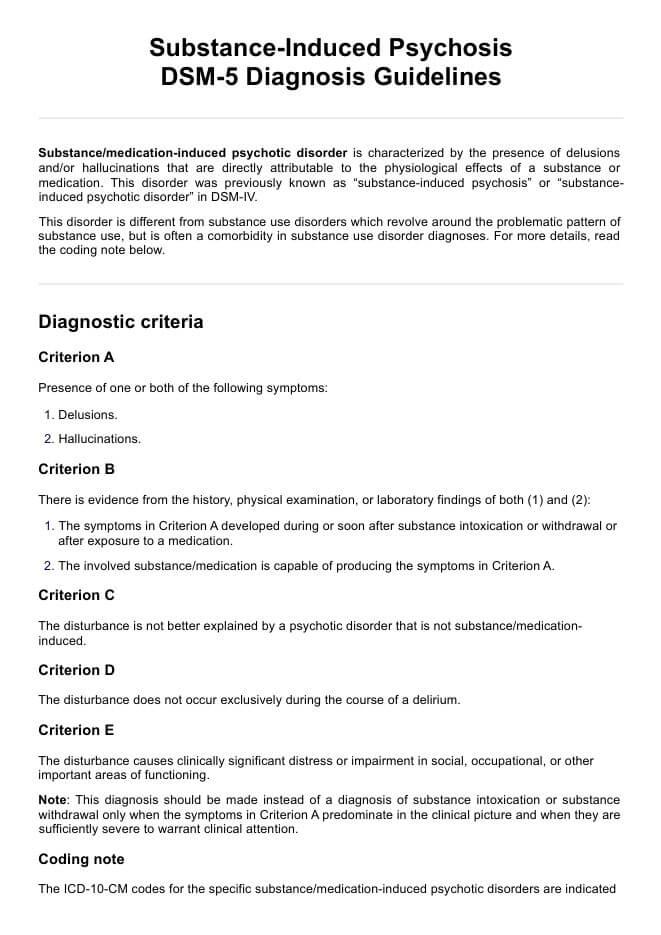
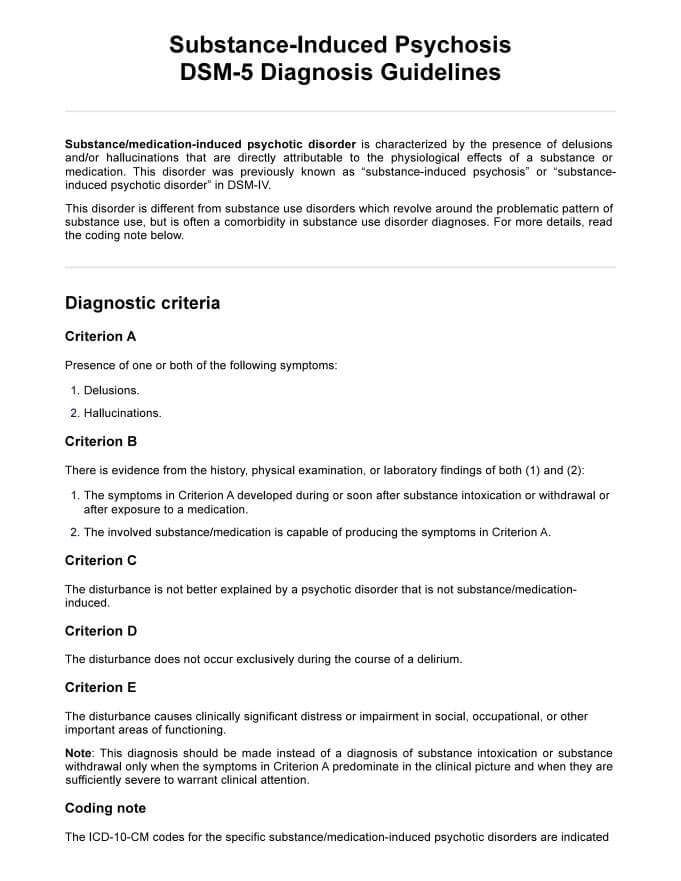
What are the DSM-5 criteria for substance-induced psychosis?
The DSM-5 diagnostic criteria for substance/medication-induced psychotic disorder are as follows:
Criterion A: Presence of one or both of the following symptoms: Delusions, hallucinations.
Criterion B: There is evidence from the history, physical examination, or laboratory findings of both (1) and (2):
- The symptoms in Criterion A developed during or soon after substance intoxication or withdrawal or after exposure to a medication.
- The involved substance/medication is capable of producing the symptoms in Criterion A.
Criterion C: The disturbance is not better explained by a psychotic disorder that is not substance/medication-induced.
Criterion D: The disturbance does not occur exclusively during the course of a delirium.
Criterion E: The disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning.
Specify current severity: Severity is rated by a quantitative assessment of the primary symptoms of psychosis, including delusions, hallucinations, abnormal psychomotor behavior, and negative symptoms. Each of these symptoms may be rated for its current severity (most severe in the last 7 days) on a 5-point scale ranging from 0 (not present) to 4 (present and severe).
Specify onset: Add the below specifiers accordingly:
- With onset during intoxication: If criteria are met for intoxication with the substance and the symptoms develop during intoxication.
- With onset during withdrawal: If criteria are met for withdrawal from the substance and the symptoms develop during, or shortly after, withdrawal.
- With onset after medication use: If symptoms developed at initiation of medication, with a change in use of medication, or during withdrawal of medication.
This diagnosis should be made instead of substance intoxication or withdrawal only when the symptoms in Criterion A predominate and are severe enough to warrant clinical attention.
Also, the table of ICD-10-CM codes for the specific substance/medication-induced psychotic disorder are indicated in the template. Note that the ICD-10-CM code depends on whether or not there is a comorbid substance use disorder present for the same class of substance. For more details about the ICD codes, applicable substances, and their specifiers, refer to our template.
Differences between DSM-IV and DSM-5 criteria
As mentioned, the terminology was updated from "substance-induced psychotic disorder" (DSM-IV) to "substance/medication-induced psychotic disorder" (DSM-5) to include medication-induced cases. The criteria were slightly reworded for clarity, such as specifying that symptoms should develop during or soon after substance intoxication or withdrawal, or after exposure to a medication. Also, Criterion E was added, which requires that the disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning.
Despite these changes, the overall diagnostic framework remained largely similar between the two editions.
How is this disorder treated?
Treating substance/medication-induced psychotic disorder focuses on managing symptoms and addressing the underlying substance use. While there is no cure, several treatment options can help improve the patient's quality of life:
- Detoxification: Medically supervised detoxification can safely manage withdrawal symptoms and alcohol-induced psychosis, reducing the risk of further psychotic episodes.
- Medications: Antipsychotics (e.g., risperidone or olanzapine) can reduce hallucinations and delusions, while benzodiazepines can manage acute agitation and anxiety.
- Behavioral therapy: Cognitive Behavioral Therapy (CBT) helps patients develop coping strategies, and contingency management uses positive reinforcement to encourage abstinence and manage related anxiety symptoms.
- Supportive care and education: Family, community support, peer groups, and education/counseling can provide emotional and practical support to aid in recovery.
Commonly asked questions
Substance/medication-induced psychotic disorder is a condition where delusions and/or hallucinations are directly caused by the physiological effects of a substance or medication.
The Diagnostic and Statistical Manual has ICD-10-CM codes for substance/medication-induced psychotic disorder, but they vary depending on the substance and the presence of a comorbid substance use disorder. Refer to our template for a detailed table of codes.
Schizophrenia is a primary psychotic disorder with no direct link to substance use, while Substance-Induced Psychosis is directly caused by the physiological effects of a substance. The DSM-5 has since updated the term to substance/medication-induced psychotic disorder to include medication-induced symptoms.


















-template.jpg)


















































































