Psychosocial Assessment
Conduct a psychosocial assessment to gauge a patient’s mental and social well-being and create a therapy plan that restores them to a better state physically, mentally, and socially.


What is a Psychosocial Assessment?
A Psychosocial Assessment comprehensively evaluates an individual's mental health and social well-being. It involves gathering information about a person's psychological state, social circumstances, and ability to function in daily life (Moone & Trenoweth, 2017).
During the assessment, a mental health professional will typically inquire about the individual's presenting problem or symptoms, mental health history, medical conditions, family or social history, social situation, and coping strategies. This assessment might also determine if the patient has suicidal or homicidal ideation. The assessment may also involve a mental status examination to evaluate the person's appearance, mood, thought processes, cognitive function, and risk of harm to self or others (Lal & Singh, 2018).
A Psychosocial Assessment aims to develop a holistic understanding of the individual, considering their unique thoughts, feelings, behaviors, relationships, and environmental factors that may contribute to their mental health (Sadock et al., 2015). This understanding forms the basis for accurate diagnosis, personalized treatment planning, and provision of appropriate support services.
Types of Psychosocial Assessment
Mental health professionals may use various types of Psychosocial Assessments depending on the specific needs and circumstances of the individual being evaluated. Some common types include:
- Comprehensive assessment: This is a thorough evaluation that covers all major areas of a person's life, including their mental health history, physical health, current symptoms, social situation, and functioning. It is often conducted when an individual first seeks mental health services or is admitted to a psychiatric facility.
- Targeted assessments: These focus on specific aspects of psychosocial functioning, such as drug or alcohol use, trauma history, or risk of self-harm. Targeted assessments may be used when a particular concern has been identified or when a more in-depth evaluation of a certain area is needed. For instance, a good mental status examination helps evaluate executive and cognitive functioning.
- Brief assessments: Shorter evaluations can be conducted in primary care settings or other non-specialty mental health contexts. They often involve screening tools or questionnaires such as a mini-mental state examination to quickly identify potential mental health problems and determine if a more comprehensive assessment is warranted.
- Ongoing assessments: These are periodic evaluations conducted throughout the course of mental health treatment to monitor the individual's progress, reassess their needs, and adjust the treatment plan as necessary. Ongoing assessments help ensure that the individual is receiving appropriate and effective care.
- Crisis assessments: These are urgent evaluations conducted when an individual is in a state of acute distress or at imminent risk of harm to self or others. This usually includes administering a scale for suicide ideation. The primary goal of a crisis assessment is to ensure the person's safety and stability, which may involve immediate interventions such as hospitalization or mobilization of support services.
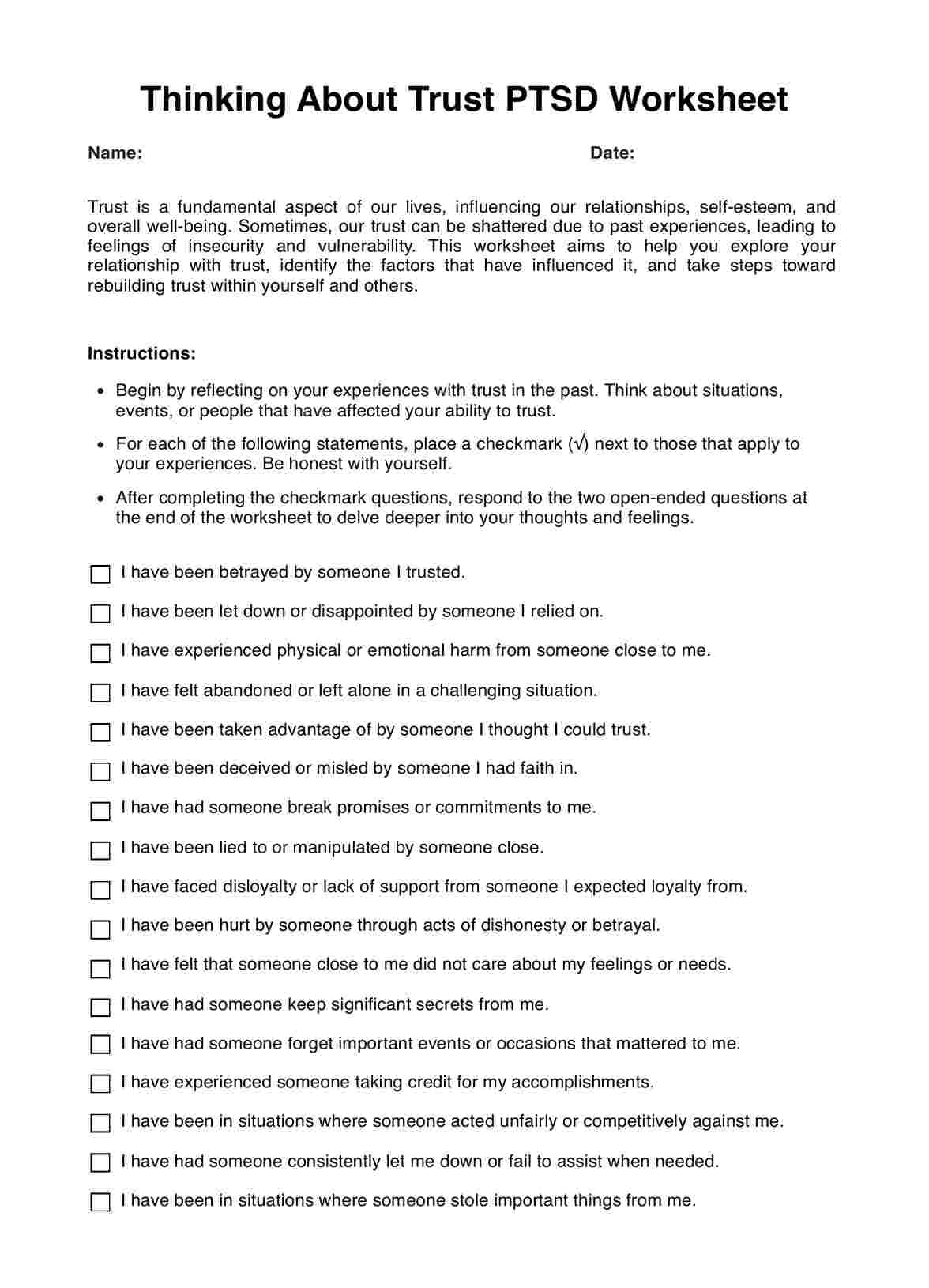
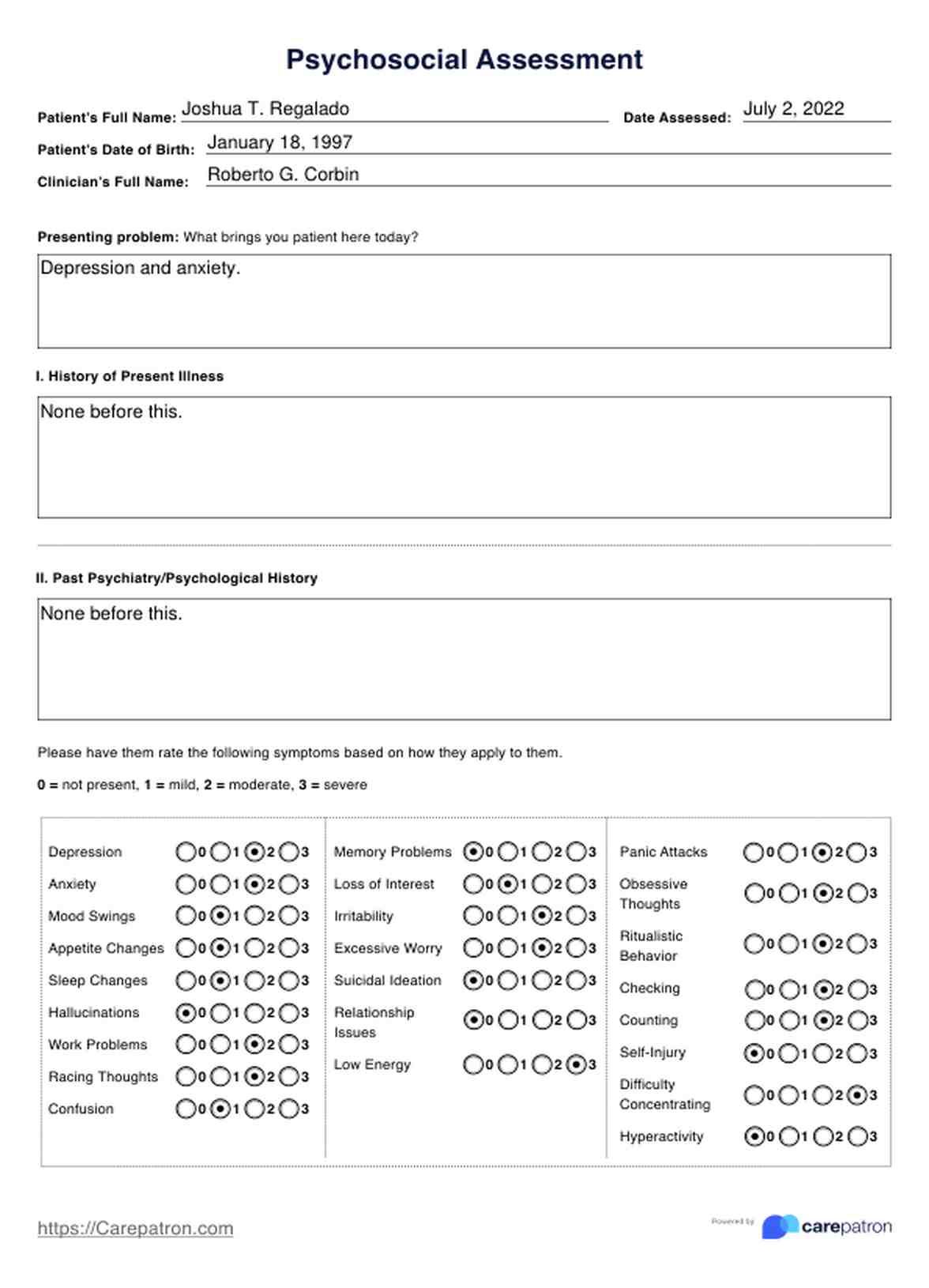
Psychosocial Assessment Template
Psychosocial Assessment Example
When do you conduct a Psychosocial Assessment?
Knowing when to conduct a Psychosocial Assessment is crucial for ensuring that patients receive the care they need promptly and effectively. Here are some key situations in which a Psychosocial Assessment is performed by mental health professionals or social workers:
Initial evaluation
When a patient first presents with mental health concerns or is referred for psychiatric evaluation, a comprehensive Psychosocial Assessment should be conducted (Sadock et al., 2015). This initial assessment gathers baseline information about the patient's symptoms, history, and current function in the community and their daily life. This serves as a foundation for further evaluation and treatment planning.
Admission to a mental health facility
A thorough Psychosocial Assessment is typically required upon admission to a psychiatric hospital, residential treatment center, or other mental health facility. This assessment helps the treatment team understand the patient's needs, develop an individualized care plan, and ensure that appropriate services are provided during the patient's stay.
Significant changes in mental health status
A Psychosocial Assessment should be conducted when a patient experiences a notable change in their mental health, such as a sudden onset of new symptoms, worsening of existing symptoms, or a crisis situation. This helps determine the nature and severity of the change and guides decisions about necessary interventions or adjustments to the treatment plan. This might screen for possible drug or alcohol abuse, poor impulse control, or the presence of mental illness.
Periodic reassessment
Throughout mental health treatment, periodic psychosocial assessments should be conducted to monitor the patient's progress, reassess their needs, and modify the treatment approach as necessary. The frequency of these reassessments may vary depending on the individual's specific needs and the setting in which care is being provided.
How does a Psychosocial Assessment work?
A Psychosocial Assessment is an evaluation of an individual's mental health, social functioning, and overall well-being. It is a valuable tool for healthcare practitioners to gather information, identify areas of concern, and develop an effective treatment plan. Here's a step-by-step guide on how healthcare providers can conduct this in practice:
Step 1: Gather background information
Begin by collecting essential details about the patient, including their name, date of birth, and the reason for the assessment. Review any available medical or surgical history, previous assessments, or referral information better to understand the patient's history and current situation.
Step 2: Conduct the clinical interview
Engage the patient in a structured clinical interview, using the Psychosocial Assessment form as a guide. Start with the presenting problem and explore the history of the current illness, including the onset, duration, and severity of symptoms. Inquire about past psychiatric and medical history, psychosocial history, medications, drug or alcohol history, history of crime or legal trouble, and any relevant family history of mental health issues.
Step 3: Assess specific domains
Delve into specific areas of the patient's life that may impact their mental health and well-being. This includes the key components of a Psychosocial Assessment:
- Addictive disorders and suicide risk: Evaluate the patient's history of substance abuse and the risk of self-harm or harming others, and assess their coping skills and support system.
- Family and social history: Explore the patient's family dynamics, relationships, community resources, and social support network that can be possible protective factors.
- Educational and work history: Discuss the patient's academic background, employment status, and job satisfaction.
- Trauma and development: Inquire about any history of abuse, neglect, or traumatic experiences and assess their impact on the patient's development and current functioning.
- Cultural assessment: Consider the patient's cultural identity, beliefs, and any experiences of discrimination or marginalization.
Step 4: Perform a mental status examination
Conduct a thorough mental status exam to assess executive function, the patient's appearance, behavior, mood, thought processes, cognition, visual-spatial perception, and judgment. Ensure that the patient is oriented to person, place, and time. Observe and document any deviations from normal functioning, as this information can provide valuable insights into the patient's mental state.
Step 5: Synthesize findings and develop a treatment plan
Analyze the information gathered from the Psychosocial Assessment to identify the patient's strengths, challenges, and areas of concern. Use this understanding to formulate a comprehensive, individualized treatment plan addressing the patient's needs. Collaborate with the primary healthcare provider and the patient to set realistic goals, recommend appropriate interventions, and ensure continuity of care.
Assessing suicide risk
Evaluating the risk of suicide or self-harm is a critical component of the Psychosocial Assessment. Warning signs that a patient may be at increased risk include:
- Expressions of hopelessness or intent to harm self
- Previous suicide attempts or self-harm behaviors
- Psychiatric disorders like depression, substance abuse, and personality disorders
- Stressful life events and relationship problems
- Social isolation and lack of support
- Impulsive, aggressive, or reckless behaviors
Comprehensive suicide assessment tools like the Scale for Suicide Ideation (SSI) and the Nurses' Global Assessment of Suicide Risk (NGASR) can aid in determining the level of risk. If a patient is deemed to be at high risk, immediate intervention to ensure safety is warranted, which may include referral for inpatient psychiatric treatment.
Benefits of conducting Psychosocial Assessment
Conducting a Psychosocial Assessment offers numerous benefits for healthcare practitioners, mental health professionals, social workers, and patients, which include the following:
Accurate diagnosis
A thorough Psychosocial Assessment helps practitioners gather essential information about a patient's symptoms, history, and functioning, which is crucial for making an accurate diagnosis. Considering the full context of a patient's life allows practitioners to differentiate between various mental health conditions and identify any co-occurring disorders that may require attention.
Individualized treatment planning
The insights gained from a Psychosocial Assessment enable practitioners to develop tailored treatment plans that address each patient's unique needs, strengths, and challenges. Understanding a patient's specific circumstances, such as their support system, coping skills, and cultural background, helps practitioners recommend interventions that are most likely effective and acceptable to the patient.
Improved patient engagement
Conducting a Psychosocial Assessment allows practitioners to build rapport and establish a therapeutic alliance with patients. Showing genuine interest in understanding a patient's experiences and perspectives allows practitioners to foster trust, encourage open communication, and increase the patient's motivation to engage in treatment.
Identification of risk factors
Psychosocial Assessments help practitioners identify potential risk factors that may impact a patient's mental health and well-being, such as a history of trauma, substance abuse, or suicidal ideation. Recognizing these risks early on allows for implementing appropriate safety measures and monitoring patients more closely to help an individual obtain optimal health and navigate the typical stresses of life.
References
Lal, R., & Singh, S. (2018). Assessment tools for screening and clinical evaluation of psychosocial aspects in addictive disorders. Indian Journal of Psychiatry, 60(Suppl 4), S444–S450. https://doi.org/10.4103/psychiatry.IndianJPsychiatry_12_18
Moone, N., & Trenoweth, S. (2017). Psychosocial assessment in mental health. Sage Publications Ltd. https://uk.sagepub.com/en-gb/eur/psychosocial-assessment-in-mental-health/book244423#description
Sadock, B. J., Sadock, V. A., & Ruiz, P. (2015). Kaplan and Sadock's synopsis of psychiatry: Behavioral sciences/clinical psychiatry (11th ed.). Wolters Kluwer Health.
Commonly asked questions
Examples of Psychosocial Assessment include evaluating an individual's mental health, social support system, coping mechanisms, and overall well-being. This may involve assessing factors such as mood, anxiety symptoms, stress levels, relationships, living situations, financial stability, and access to community resources. Psychosocial Assessments can also explore an individual's cultural, spiritual, and educational background, as well as any history of trauma or adverse life events.
Typical questions asked during a Psychosocial Assessment may include: How would you describe your current mood and emotional state? Do you have a support system of family and friends? How do you typically cope with stress or difficult situations? Have you experienced any significant life changes or traumatic events recently?
Psychosocial Assessments are conducted to gain a comprehensive understanding of an individual's overall well-being and identify any potential social, emotional, or environmental factors that may impact their health and functioning. This information is crucial for developing a personalized care plan that addresses the individual's unique needs and helps them achieve their desired outcomes.


















-template.jpg)