Psychiatric Evaluation Template
Diagnose mental health problems and disorders with the help of our Psychiatric Evaluation Template. Click here for a guide and a free template copy!


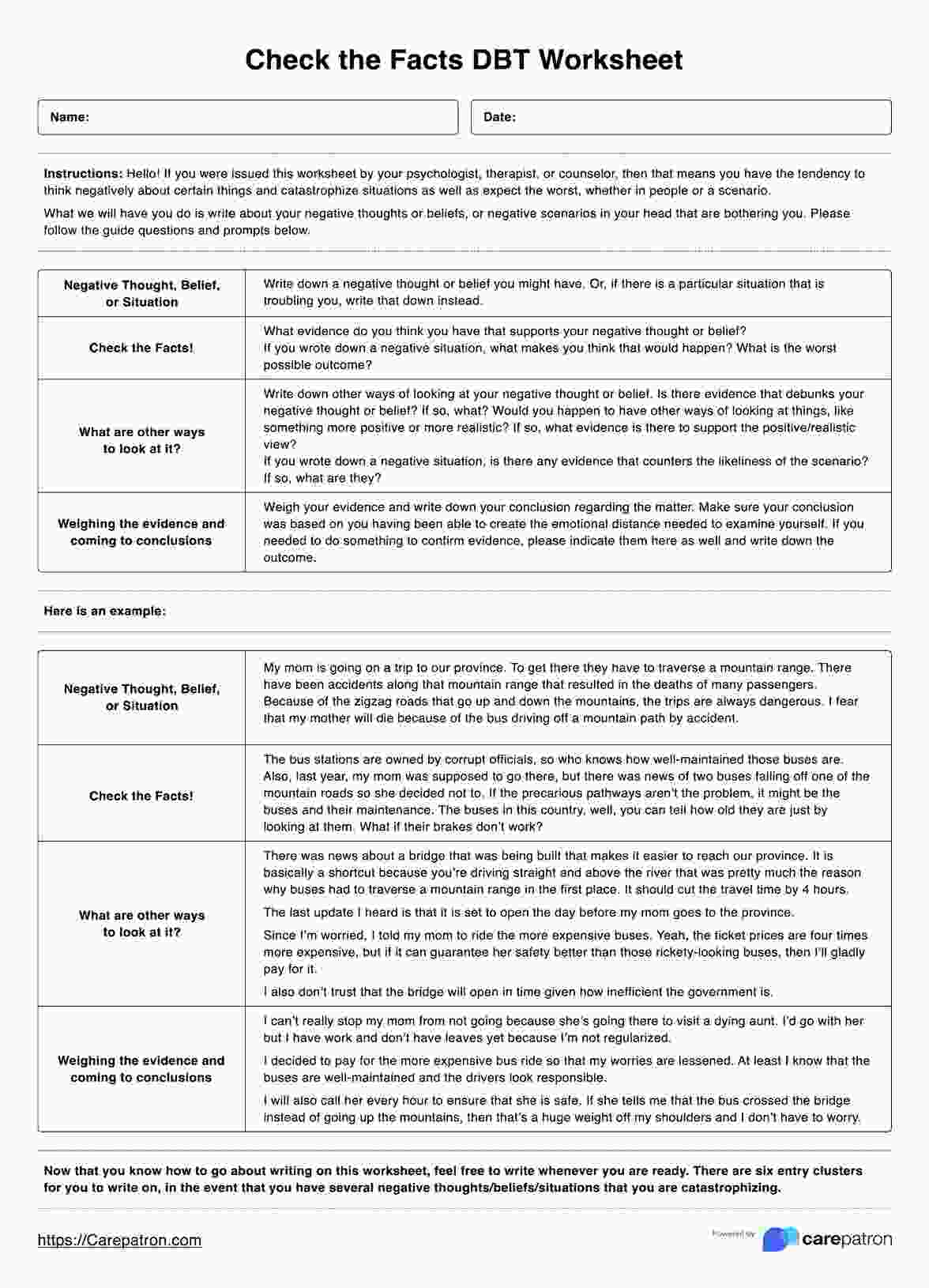
What is a psychiatric evaluation?
In the field of mental health, conducting an initial psychiatric evaluation is essential for accurate diagnosis and effective treatment planning. This is a comprehensive process conducted to evaluate an individual’s mental health status, identify any potential mental health disorders, mental health conditions, or psychiatric disorders, and develop an appropriate treatment plan. Here's an elaboration of each of the steps done during an evaluation:
Clinical interview
The mental health professional will conduct a detailed interview to gather information about the individual’s current and past symptoms, life experiences, past psychiatric history, medical history, and overall functioning to understand the person’s unique circumstances and concerns.
Mental status examination
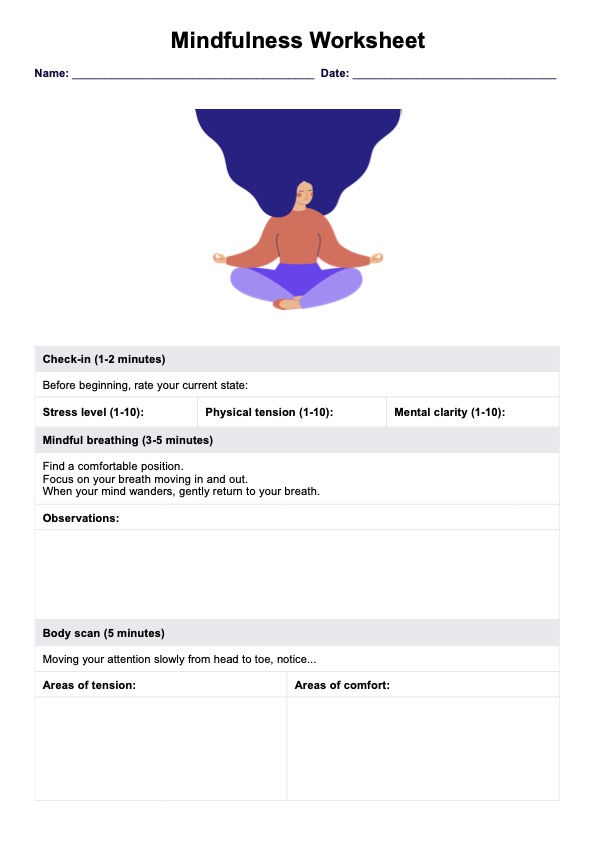
Afterward, the professional observes and assesses the individual’s appearance, behavior, speech, thought process, mood, and cognitive abilities. Observing for signs of self-harm, such as scars or injuries, is crucial as it can indicate the patient's mental state or underlying conditions like depression or anxiety.
Psychological testing
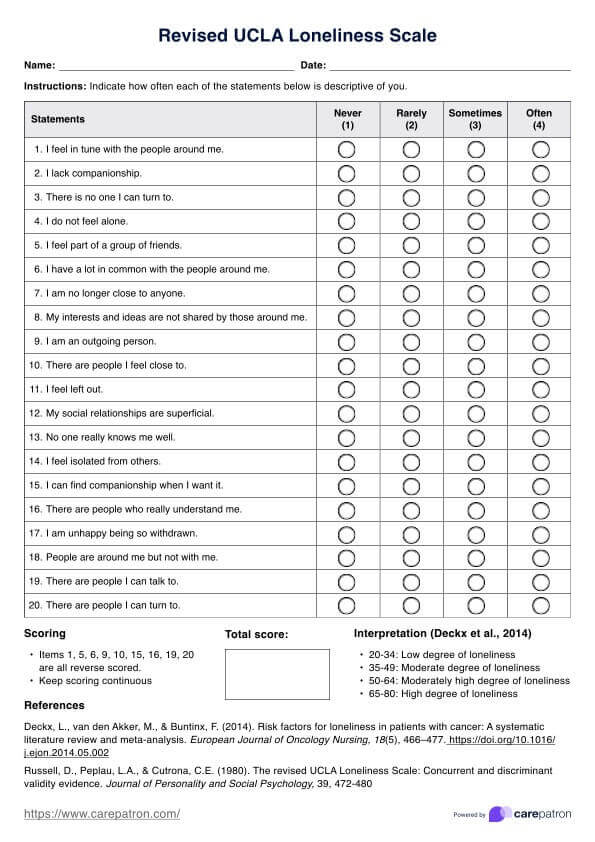
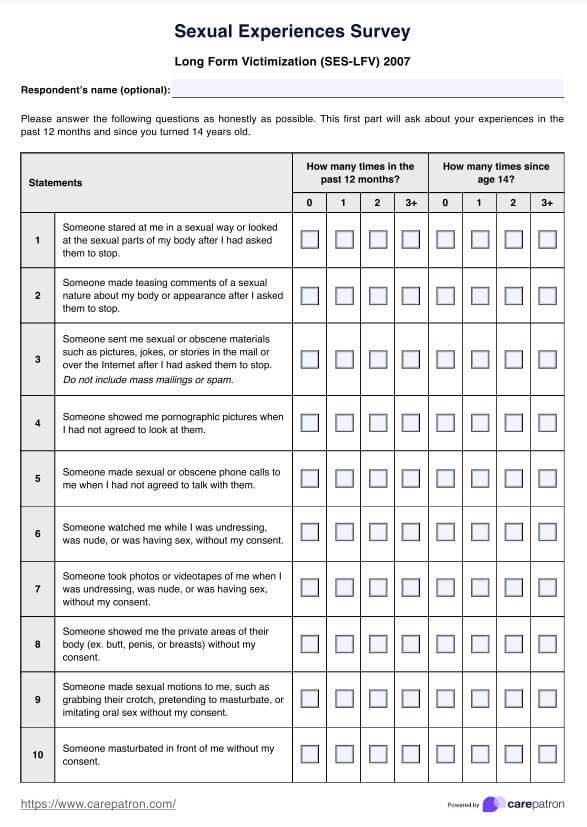
In some cases, the professional may administer standardized psychological tests or questionnaires to evaluate further specific areas of concern, such as depression, anxiety, or challenges in cognitive function, such as accomplishing activities that need sustained mental effort.
Collateral information
The evaluator may gather additional information from family members, friends, a doctor, or other relevant sources, including the patient's social history, to better understand the individual’s condition and its impact on their daily life.
Physical examination and lab tests
In some instances, a physical examination or laboratory tests may be ordered to rule out potential medical conditions that could contribute to or mimic psychiatric symptoms.
After collecting and analyzing all relevant information, the mental health professional integrates the findings to determine the presence of any psychiatric disorders or mental health concerns.
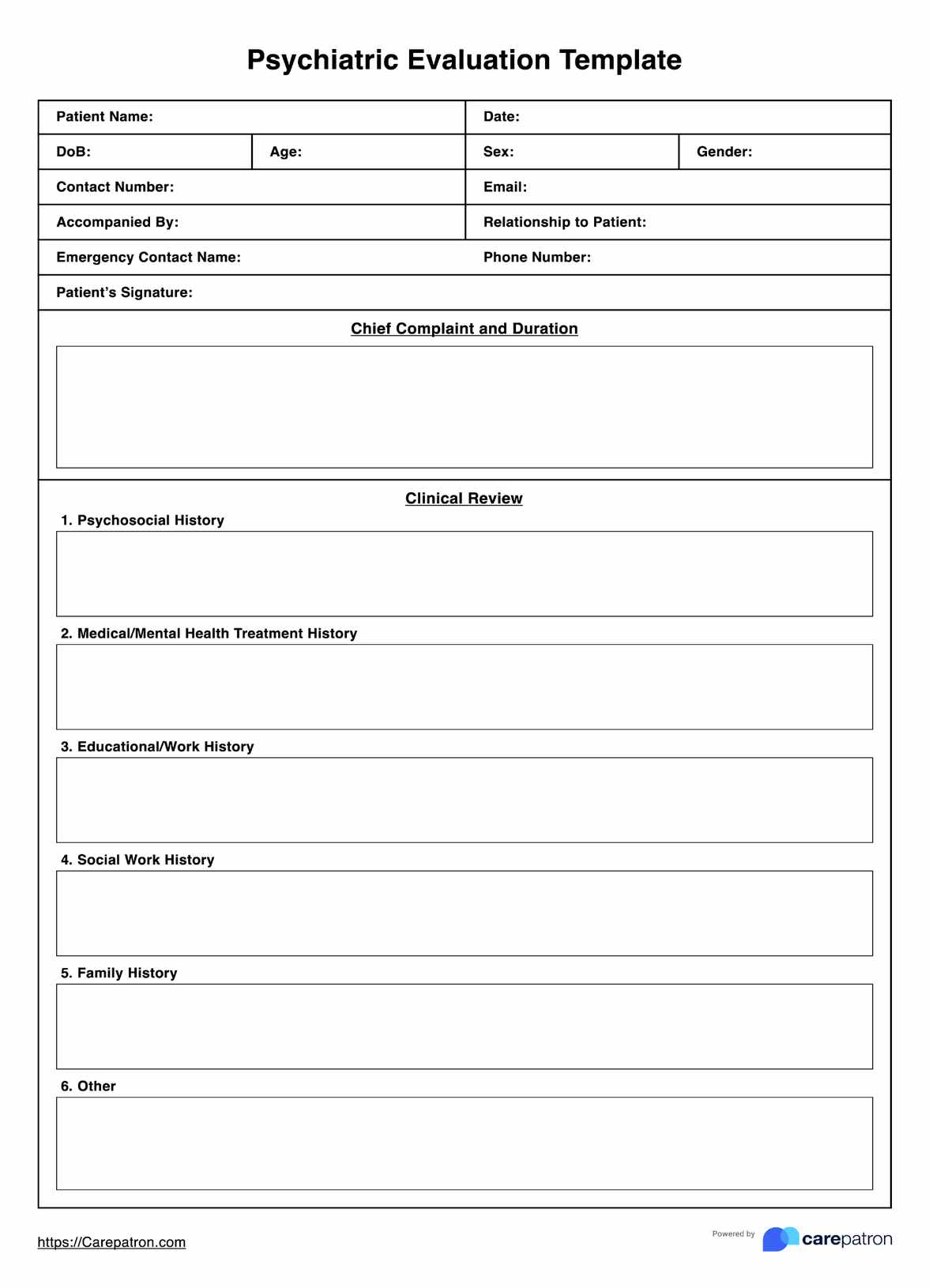
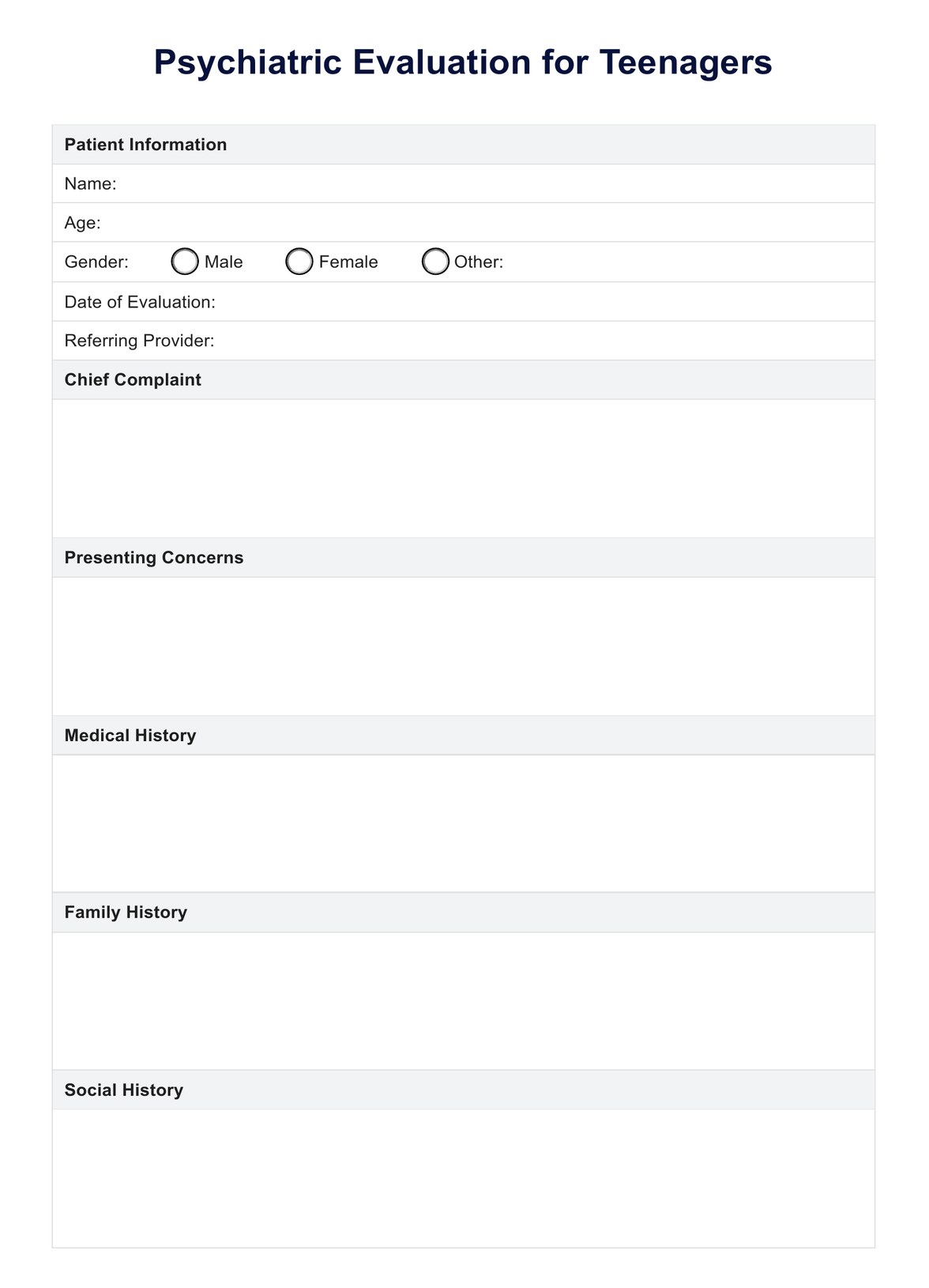
Psychiatric Evaluation Template
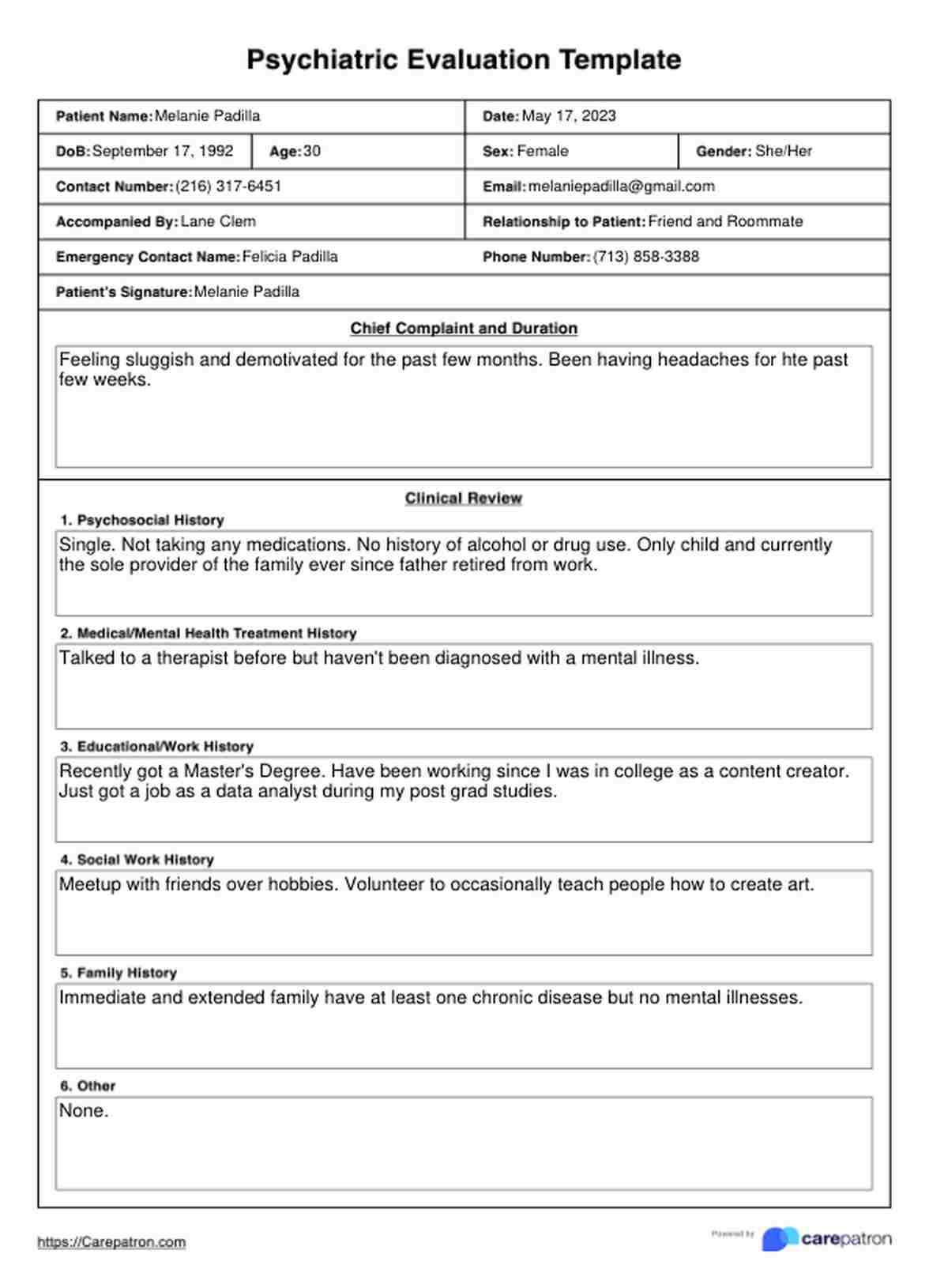
Psychiatric Evaluation Template Example
What is a Psychiatric Evaluation Template?
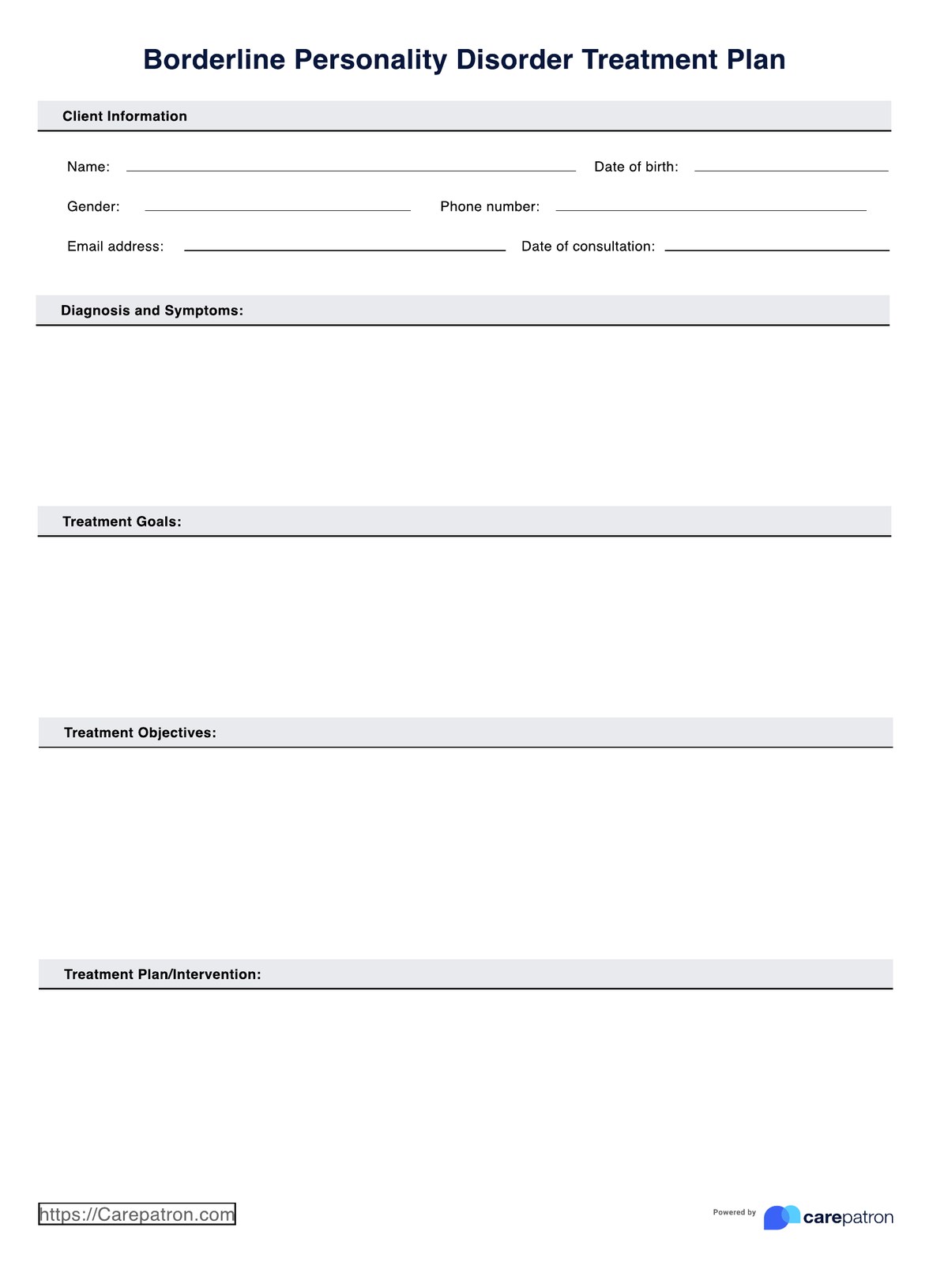
Evaluation forms like a Psychiatric Evaluation Template are crucial in the psychiatric evaluation process. A Psychiatric Evaluation Template is a structured document or form designed to guide healthcare professionals through a comprehensive assessment of an individual’s mental health status. It also serves as a tool to gather and organize relevant information.
Though the evaluation form content and interview flows vary depending on the clinician, they still require information regarding the patient. These are:
- Identifying information: This section captures the individual’s personal details, such as name, age, gender, and contact information.
- Chief complaint: Here, the healthcare professional documents the primary reasons for seeking the evaluation, including any specific symptoms of a present illness, behaviors, or concerns reported by the individual or their loved ones.
- Medical and psychiatric history: This section explores the individual’s past and current medical conditions, psychiatric diagnoses, hospitalizations, treatments, past and current medications, substance abuse history, and developmental history.
- Psychosocial history: This section covers the individual’s educational background, employment status, living situation, social support system, and any significant life events or stressors.
- Mental status examination: During the evaluation, the healthcare professional documents their observations and assessments of the individual’s appearance, behavior, speech, mood, thought processes, cognition, and insight.
How does this Psychiatric Evaluation Template work?
When conducting a psychiatric evaluation, healthcare practitioners can follow these steps:
Step 1: Review the template and prepare
Practitioners should familiarize themselves with the section, structure, and possible answers of the template before the evaluation using our psychiatric assessment example. They should also ensure that all necessary materials, such as pens, clipboards, or electronic devices for documentation, are readily available.
Step 2: Gather background information
Begin the evaluation by collecting the individual’s identifying information, such as name, age, and contact details. Then, obtain comprehensive medical, psychiatric, and substance use histories, including past history and relevant family history. This information can be gathered through interviews or by reviewing existing records.
Step 3: Conduct the clinical interview and assessment
Use the template as a guide to conduct a thorough clinical interview and assessment. Explore the reason for the evaluation, including presenting concerns, symptoms, or behaviors, and trace the history of the presenting illness. A healthcare professional may also perform a mental status examination during this step.
Step 4: Review and secure notes
Once you've completed the interview, you can review your notes to ask your patient for further clarification or to organize them. Afterward, remember to store your physical copies at a location with security measures or within Carepatron's patient record software.
What is a mental illness test?
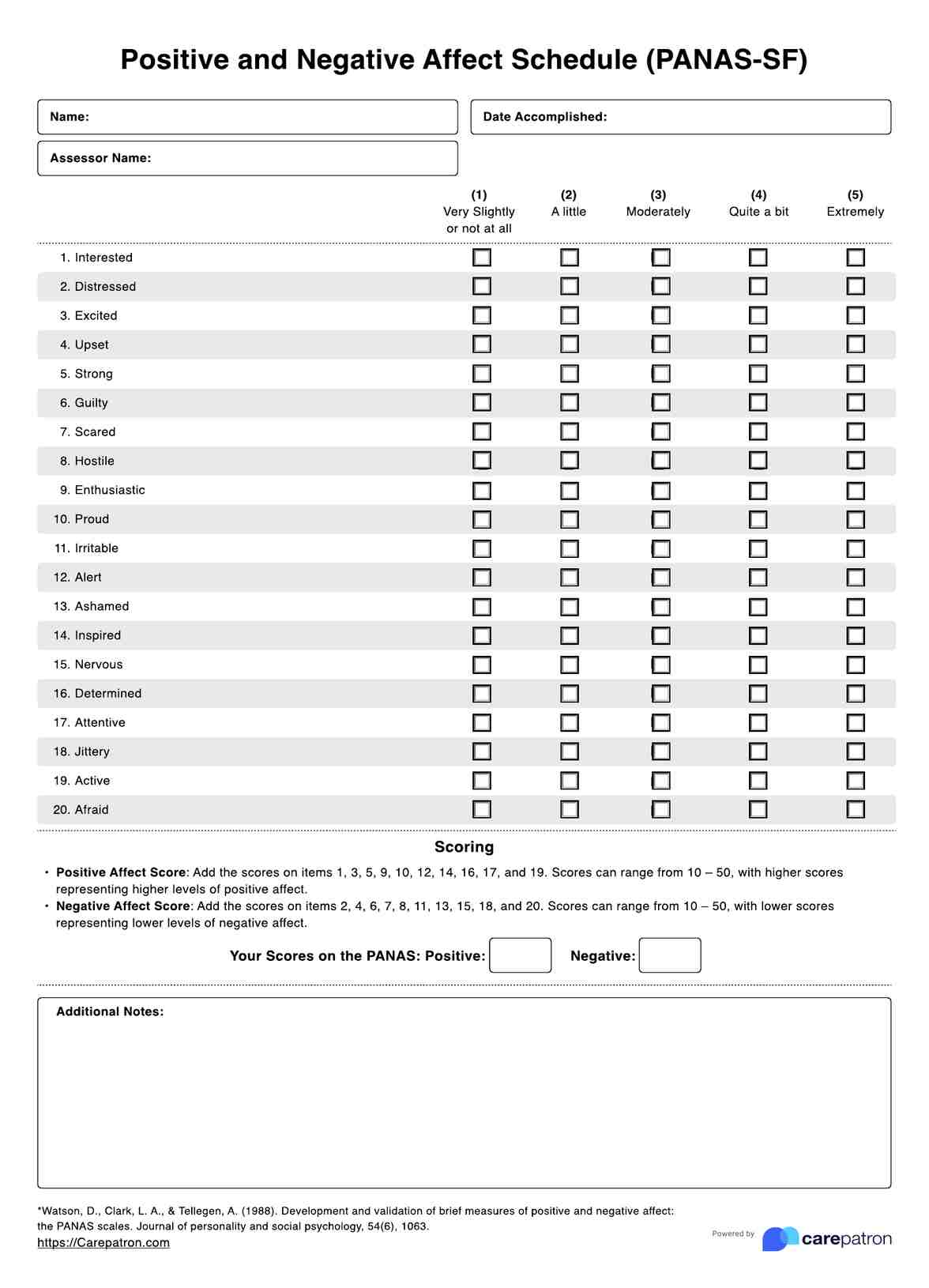
A mental illness test, also known as a mental health evaluation or psychological assessment, plays a crucial role in identifying a potential mental health condition or disorder. These tests are designed to evaluate an individual’s cognitive, emotional, and behavioral functioning through various methods, such as self-assessments, structured interviews, and performance-based tasks.
Here, we will explore some common types of mental health tests used to screen for or assess common mental health issues:
Anxiety test
Anxiety disorders are among the most common mental health concerns. Several screening tools are used to assess the presence and severity of anxiety symptoms, including:
- Generalized Anxiety Disorder-7 (GAD-7): A self-report questionnaire that measures the frequency and severity of anxiety symptoms over the past two weeks.
- Beck Anxiety Inventory (BAI): A self-report inventory that evaluates the severity of anxiety symptoms, both physiological and cognitive (Beck et al., 1988).
Depression test
Depression is a mood disorder characterized by persistent feelings of sadness, loss of interest, and other emotional and physical symptoms. Common screening tools for depression include:
- Patient Health Questionnaire-9 (PHQ-9): This self-report questionnaire assesses the presence and severity of depressive symptoms over the past two weeks (Kroenke et al., 2001).
- Beck Depression Inventory (BDI): This is a self-report mental health test that measures the severity of depressive symptoms, including cognitive, affective, and somatic components.
Posttraumatic stress disorder (PTSD) test
Post-traumatic stress disorder (PTSD) is a mental health condition that can develop after exposure to traumatic events. Screening tools for PTSD include:
- PTSD Checklist for DSM-5 (PCL-5): A self-report measure that can point to the presence and severity of PTSD symptoms based on the diagnostic criteria in the DSM-5.
- Clinician-Administered PTSD Scale for DSM-5 (CAPS-5): A structured clinical interview conducted by a trained professional to assess PTSD symptoms and their impact (Weathers et al., 2018).
Obsessive-compulsive disorder (OCD) test
Obsessive-compulsive disorder (OCD) is characterized by intrusive thoughts, obsessions, and repetitive behaviors or compulsions. Screening tools for OCD include:
- Yale-Brown Obsessive-Compulsive Scale (Y-BOCS): A semi-structured clinician-administered interview that assesses the severity of obsessions and compulsions.
- Obsessive-Compulsive Inventory-Revised (OCI-R): A self-report questionnaire that measures the presence and severity of OCD symptoms (Foa et al., 2002).
References
Beck, A. T., Epstein, N., Brown, G., & Steer, R. A. (1988). An inventory for measuring clinical anxiety: psychometric properties. Journal of Consulting and Clinical Psychology, 56(6), 893–897. https://doi.org/10.1037//0022-006x.56.6.893
Foa, E. B., Huppert, J. D., Leiberg, S., Langner, R., Kichic, R., Hajcak, G., & Salkovskis, P. M. (2002). The Obsessive-Compulsive Inventory: development and validation of a short version. Psychological Assessment, 14(4), 485–496.
Kroenke, K., Spitzer, R. L., & Williams, J. B. (2001). The PHQ-9: validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
Weathers, F. W., Bovin, M. J., Lee, D. J., Sloan, D. M., Schnurr, P. P., Kaloupek, D. G., Keane, T. M., & Marx, B. P. (2018). The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5): Development and initial psychometric evaluation in military veterans. Psychological assessment, 30(3), 383–395. https://doi.org/10.1037/pas0000486
Commonly asked questions
Individuals can start by scheduling an appointment with a mental health professional, such as a psychiatrist, psychologist, or licensed therapist. During the assessment, the clinician will comprehensively evaluate the individual's mental health history, symptoms, and current concerns. They may use standardized assessments, interviews, and observations to formulate a diagnosis and develop a treatment plan tailored to the individual's needs.
The perception of the hardest mental illness to live with can vary among individuals, as mental health conditions affect people differently. Conditions like schizophrenia, bipolar disorder, and severe depression can be particularly challenging due to their impact on daily functioning, relationships, and overall quality of life. Each person's experience with mental illness is unique, and the level of difficulty can depend on various factors, including symptom severity, access to treatment, and social support.
While some mental illnesses can be effectively managed and symptoms reduced with treatment, there is no universal cure for mental illness. Mental health conditions are often chronic and may require ongoing treatment, such as therapy, medication, lifestyle changes, and support services. Recovery is possible, and many individuals can lead fulfilling lives with proper management and support.
















-template.jpg)