Multidimensional Inventory of Dissociation (MID)
Use the Multidimensional Inventory of Dissociation to screen patients for potential dissociative disorders.


What are dissociative disorders?
A dissociative disorder is a disruptive mental health disorder that forms in people who have experienced traumatic events or anything seriously distressing. This kind of disorder "helps" them push away any unwanted thoughts or memories concerning such traumatic and distressing experiences.
Three types of dissociative disorders
There are three types of dissociative disorders:
Dissociative amnesia
A kind of memory loss that may last for a few minutes to even years, depending on how severe. Dissociative amnesia wipes out memories and information of oneself and others concerning a specific point in time when a traumatic/distressing event occurred.
Depersonalization disorder
Sometimes called depersonalization/derealization disorder. A person with this disorder will have either depersonalization, derealization, or both. Known depersonalization-related phenomena include the feeling of becoming separate from the body. A person with this disorder will likely feel like they're watching themselves do things from a distance. The latter will make them feel like things aren't real, that they're in a foggy dreamworld version of reality where time moves slowly.
Dissociative identity disorder
This disorder makes a person feel like they have different versions of themselves living in them, and they switch between these identities from time to time. These identities will likely have different names, mannerisms, attitudes, and histories. They might even grapple with the feeling of these identities talking to them, and they might also feel like they're not sure who they are (identity confusion).
Common dissociative symptoms
People with a dissociative disorder will experience any of the following symptoms besides the ones associated with the specific types above:
- Difficulty or inability to cope healthily or well with emotional, work, or relationship-related stress
- Depression
- Anxiety
- Self-harming/suicidal thoughts and behaviors
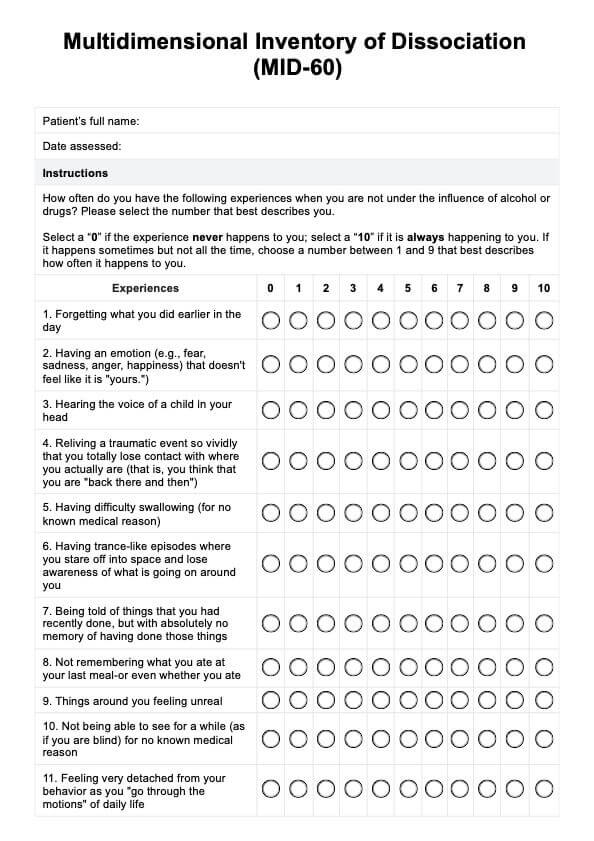
Multidimensional Inventory of Dissociation (MID) Template
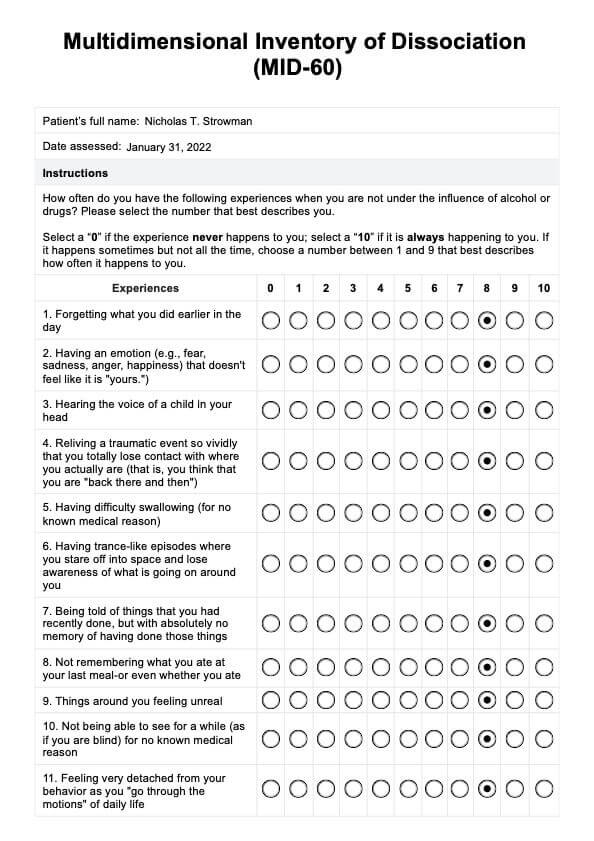
Multidimensional Inventory of Dissociation (MID) Example
What is the Multidimensional Inventory of Dissociation (MID)?
To assess a patient for a potential dissociative disorder or pathological dissociation, one of the tools that mental health professionals can use is the Multidimensional Inventory of Dissociation (MID) created by Mary-Anne Kate, Graham Jamieson, Martin J. Dorahy, and Warwick Middleton.
This dissociative disorder assessment is a comprehensive measure meant to be answered by people aged 18+ and was created with the criteria for dissociative disorders set by The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition in mind.
How is it structured and answered?
The assessment takes the form of a 60-item index. They must rate themselves based on how much each item applies to them. Here are some examples of statements they have to rate while keeping in mind that these statements revolve around experiences that happen without the use of substances or alcohol:
- Forgetting what you did earlier in the day
- Hearing the voice of a child in your head
- Having difficulty swallowing (for no known medical reason)
- Things around you feeling unreal
- Feeling uncertain about who you really are
- Feeling that other people, objects, or the world around you are not real
To answer each item, they must rate themselves between 0 to 10, with 0 meaning "never" and 10 meaning "always."
How is it scored, and how are the results interpreted?
Once a fully accomplished index has been submitted, mental health care professionals will calculate the total mean score by averaging all 60 responses and multiplying the average by 10. To interpret the scores, they just need to refer to these score ranges:
- 0–7: Does not have dissociative experiences.
- 7–14: Has few diagnostically significant dissociative experiences.
- 15–20: Mild dissociative symptoms and experiences. Post-traumatic stress disorder (PTSD) or a mild dissociative disorder (such as dissociative amnesia, depersonalization / derealization disorder) are possible.
- 21–30: May have dissociative disorder and/or PTSD.
- 31–40: May have a dissociative disorder (such as OSDD-1 or dissociative identity disorder (DID) ) and PTSD.
- 41–64: Probably has DID or a severe dissociative disorder and PTSD.
- 64+: Severe dissociative and post-traumatic symptoms. High scores may also reflect neuroticism, attention-seeking behavior, exaggeration or malingering of symptoms, or psychosis.
How to use our Multidimensional Inventory of Dissociation template
If you believe adding the Multidimensional Inventory of Dissociation to your roster of clinical assessments will help you cover more ground with your mental health patients with potential dissociative disorders, we'd like you to know we have a template for it!
Our template simply takes the MID-60 (the 60-item version of the MID) and adds radio buttons for people to tick with a pen (if they're in print) or with a click of a mouse/tap of a screen (if digital).
There's also notes box where mental health professionals can write down their next steps.
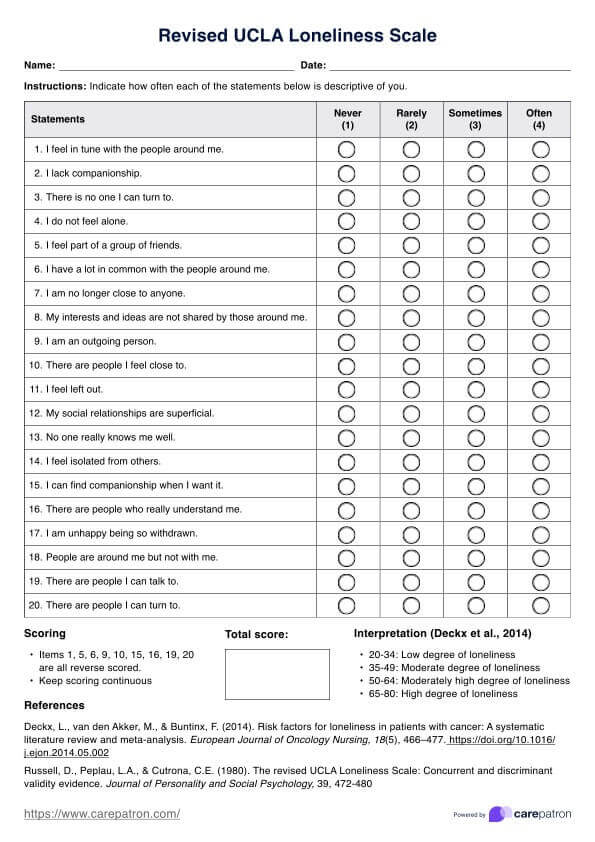
We recommend using other assessments alongside this, such as the dissociative experiences scale and identity confusion scales to cover as much ground as possible.
Benefits of using this inventory
It tackles various symptoms of dissociative disorders
The Multidimensional Inventory of Dissociation has several subscales that can help professionals determine the specific type of dissociative disorder they can zoom into when assessing patients. These subscales are:
- DID: Amnesia (for recent events) – items 42, 45, 48, 58. Clinical cutoff = 10
- DID / OSDD-1: Subjective awareness of alter personalities and self-states – items 3, 36, 39, 49, 57. Clinical cutoff = 20
- DID / OSDD-1: Angry intrusions – items 28, 33, 35, 46, 60. Clinical cutoff = 18
- DID / OSDD-1: Persecutory intrusions – items 22, 37, 44, 56, 59. Clinical cutoff = 18
- Derealisation/Depersonalisation – items 2, 7, 9, 13, 25, 47, 50, 53. Clinical cutoff = 20
- Dissociative amnesia: Distress about severe memory problems – items 1, 8, 20, 38, 43, 52. Clinical cutoff = 30
- Dissociative amnesia: Loss of autobiographical memory – items 16, 19, 24, 29, 34. Clinical cutoff = 34
- PTSD: Flashbacks – items 4, 15, 31, 40, 54. Clinical cutoff = 16
- Conversion disorder: Body symptoms – items 5, 10, 14, 18. Clinical cutoff = 10
- Conversion disorder: Pseudo-Seizures (Psychogenic non-epileptic seizures) – item 26. Clinical cutoff = 10
- General subscales: Trance – items 21, 27, 30, 32, 41, 51. Clinical cutoff = 11.7
- General subscales: Self-confusion – items 6, 11, 12, 17, 23, 55. Clinical cutoff = 33.3
These are calculated by adding the total score for all items included in the subscale, dividing them by the total number of items included in the subscale, and then multiplying it by 10. If subscale scores are past clinical cutoffs, the higher the chance that a person has specific symptoms of dissociative disorders.
It can be used to monitor patients
Let's stipulate that a patient has already been diagnosed with a dissociative disorder and treatment plans have been implemented. You can schedule follow-up appointments and use this tool again to see if their scores are getting lower or higher. If they're getting lower when compared with the initial testing, you can definitely say the treatments are working. If they're still within the same severity level or worse, you can determine the adjustments needed for the treatment.
Commonly asked questions
It can be accomplished within 5 to 10 minutes.
It is a screening tool and should not be the sole assessment during the diagnostic process. It's best to use other tools to cover all bases before cross-checking everything with the latest edition of the DSM.
Common treatments include medication for accompanying issues like depression and anxiety. Psychotherapy should help address the traumatic/distressing experience that caused a patient to develop a dissociative disorder.
There is no "cure," however, they can be managed with healthy coping mechanisms, which they can learn through therapy. Coping mechanisms and strategies will work to improve the mental well-being of a patient with a dissociative disorder to the point that the disorder doesn't or rarely becomes disruptive.

















-template.jpg)



















































































