Guided Notes Template
Enhance student learning of clinical documentation skills with our Guided Notes Template, a structured format for compiling comprehensive patient records.


What are guided notes?
Guided notes are structured resource designed to guide the user through the process of comprehensive clinical note taking. These templates are used in various healthcare settings to facilitate comprehension of the various aspects of documenting case details. They are especially useful in teaching students critical note taking skills.
Also known as patient note templates or clinical note templates, guided notes provide a framework for healthcare practitioners to document all the essential information during patient encounters. By offering a clear pathway for notetaking, this template ensures that crucial details are captured accurately and comprehensively.
SOAP (subjective, objective, assessment, plan) is a standard format used within healthcare for clinical documentation. This structured approach enhances efficiency and clarity, ensuring every key aspect of a patient's presentation is communicated. This format promotes consistency in documentation, ensuring thorough assessment of patient presentation and care.
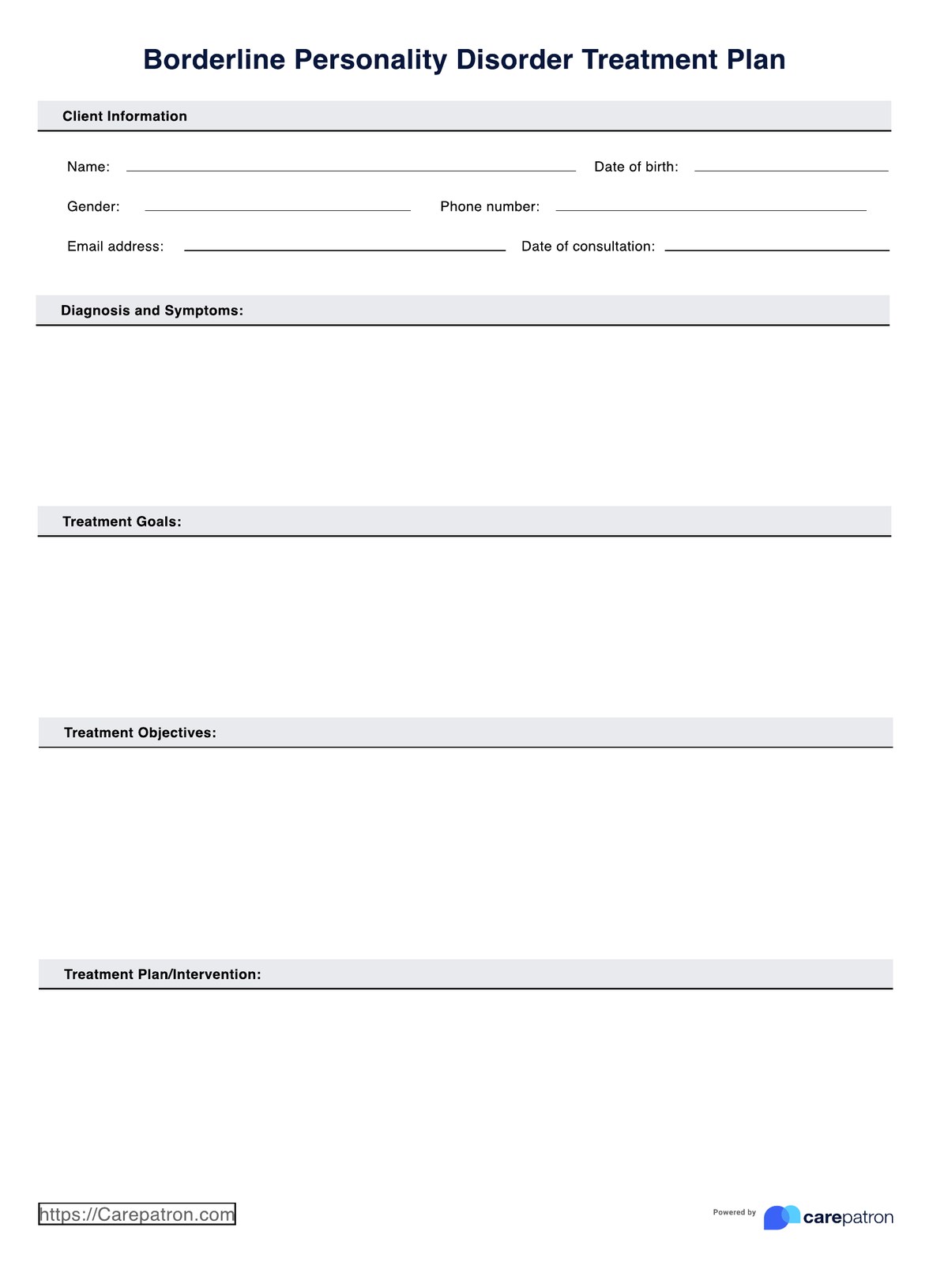
Guided Notes Template
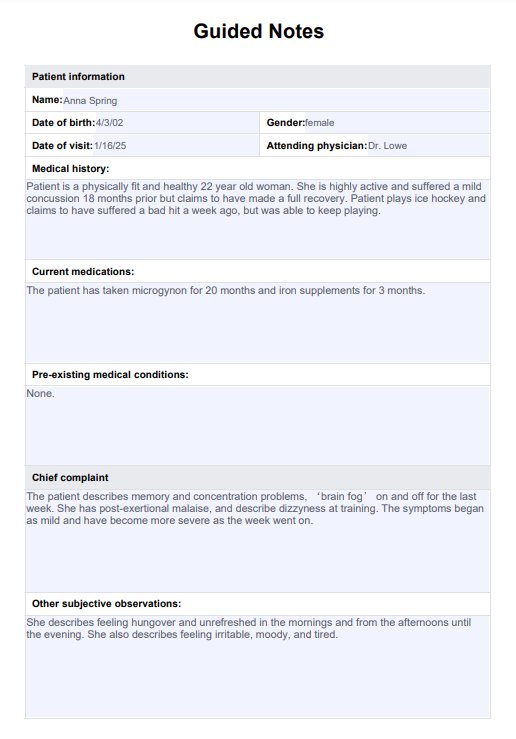
Guided Notes Template Example
How to use this template?
There are several steps to using the Guided Notes Template effectively. To ensure comprehensive and organized documentation of patient encounters, follow these guidelines:
Step 1: Access the template
Click the "Use template" button to access and customize the template via the Carepatron app. For a free printable PDF copy, choose "Download."
Step 2: Familiarize yourself
Take a moment to review the structure and sections of the Guided Notes Template. Become familiar with the components (such as patient information, chief complaint, assessment, plan, and additional notes) prior to creating your notes. Understanding the layout will help streamline the documentation process.
Step 3: Gather patient information
Begin by filling in the template's patient demographics and medical history sections. Input relevant details such as the patient's name, age, gender, date of visit, and pertinent medical conditions or medications.
Step 4: Document chief complaint
Record the patient's primary reason for the visit in the chief complaint section. Include details regarding the symptom duration, severity, aggravating factors, and alleviating factors associated with the presenting problem. The patient's perspective on their symptoms, feelings and condition are the 'subjective' part of the notes.
Step 5: Conduct assessment
Proceed to document the findings from your assessment, including vital signs, physical examination results, and any diagnostic tests ordered. Use the designated sections of the template to organize this information systematically. These are the 'objective' components of the format.
Step 6: Develop a plan
Based on your assessment, outline the treatment plan, patient education, referrals, and follow-up instructions in the appropriate sections of the template. Ensure the plan addresses the patient's needs and aligns with clinical guidelines.
Step 7: Set patient goals
Collaborate with the patient to establish short-term and long-term goals for their care. Document these goals, actionable steps, and expected outcomes in the patient goals section of the template.
Step 8: Review and save
Review the completed Guided Notes Template to verify accuracy and completeness. Make any necessary revisions or additions before saving the document. Ensure the finalized notes are securely stored in the patient's medical record.
Benefits of using guided notes in clinical documentation
Utilizing a note-taking template allows healthcare practitioners to focus on the assessment quality instead of grappling with formatting or forgetting critical details. Here are some of the key benefits for healthcare professionals and students:
Enhanced efficiency and accuracy
Guided notes provide a structured framework for documenting patient encounters, reducing the time spent on note-taking and ensuring thorough documentation. The predefined format helps capture essential information efficiently and accurately.
Standardization of documentation practices
Utilizing guided notes promotes consistency in clinical documentation. With predefined sections for demographics, assessments, plans, and follow-up instructions, this template facilitates seamless communication and information sharing among multidisciplinary teams.
Improved communication and continuity of care
Guided notes facilitate clear and concise communication of relevant clinical details, treatment plans, and patient goals to colleagues involved in patient care. This ensures continuity of care and ensures that all team members are informed of the patient's healthcare needs.
Facilitated compliance with regulatory requirements
Guided notes help healthcare organizations maintain quality standards of documentation. By providing a structured format, guided notes assist practitioners in meeting guidelines set forth by regulatory bodies and accrediting agencies, reducing the risk of compliance errors.
Support for teaching and training
Guided notes are valuable educational tools for teaching and training healthcare students and trainees. Hands-on experience with guided notes supports students to develop essential documentation skills, reinforcing clinical knowledge and competencies.
Tips on writing concise and comprehensive clinical notes
Writing concise and comprehensive clinical notes is essential for effective communication in healthcare settings. Here are some tips to utilize guided notes templates to create high-quality clinical records, while saving time and ensuring accuracy:
- Focus on essential information: Prioritize critical details relevant to the patient's condition, treatment plan, and progress. Avoid including extraneous information to maintain clarity and conciseness.
- Use Cornell or scaffolded notes formats: Incorporate formats like Cornell or scaffolded notes to divide your clinical notes into sections for objectives, summaries, and reflections. This organization can help to streamline information retrieval and review.
- Engage students in note-taking: Encourage active participation from students by providing instructor-prepared handouts or by demonstrating how to complete the template during lessons. This promotes a deeper understanding and greater retention.
- Provide examples and references: Include relevant examples and references within your notes to illustrate concepts and provide additional context. This enriches the learning experience and reinforces understanding.
- Ensure clarity and organization: Maintain a clear and organized structure throughout your notes, using headings, bullet points, and formatting to facilitate readability and comprehension.
- Regularly update and review notes: Continuously update your notes with new content and revisions to reflect the latest information and guidelines. Regular review ensures accuracy and relevance.
Commonly asked questions
The Guided Notes Template is essential because it helps students focus, understand key concepts, and organize information during lessons.
The guided notes note-taking method is a structured approach where key points or questions are provided in advance, guiding students or learners to focus on essential information during lectures or readings.
To structure guided notes, organize information into sections such as objectives, key concepts, summaries, and questions. Use bullet points or fill-in-the-blank formats to prompt engagement and comprehension.



















-template.jpg)