Fear-Avoidance Beliefs Questionnaire
Our free Fear-Avoidance Beliefs Questionnaire (FABQ) example unlocks insights into fear-avoidance beliefs. Download the PDF now for reference!


What are fear-avoidance beliefs?
Fear-avoidance beliefs, which stem from both emotional fears of pain and injury and informational beliefs about the causes and consequences of pain, are critical in understanding pain-related behaviors. These beliefs lead individuals to perceive pain as threatening, resulting in fear, hypervigilance, and avoidance behaviors that can worsen and perpetuate pain and disability, especially in chronic conditions.
The fear-avoidance model explains this cycle, where the anticipation of pain triggers avoidance behaviors and emotional distress, amplifying the pain experience. Conversely, perceiving pain as non-threatening encourages confrontation and recovery. The Fear-Avoidance Beliefs Questionnaire (FABQ) assesses the extent of these beliefs, with higher scores indicating stronger fear-avoidance beliefs, highlighting the importance of addressing these beliefs in managing pain-related disability.
What causes people to develop these fears?
Several factors contribute to the development of fear-avoidance beliefs in people with pain:
- Catastrophic misinterpretation of pain: When pain is viewed as highly threatening and indicative of severe harm, it can trigger fear responses and avoidance behaviors. Catastrophic thoughts, imagining the worst possible outcomes, are critical drivers of fear-avoidance beliefs.
- Negative information and beliefs about pain: Pre-existing negative beliefs and threatening information about pain and injury can fuel catastrophic interpretations and fears. Beliefs that specific movements or activities will cause pain or further damage encourage avoidance behaviors.
- Anxiety sensitivity and negative affect: Individuals prone to anxiety and negative thinking are more likely to develop fear-avoidance beliefs when experiencing pain. Anxiety sensitivity, or the fear of anxiety symptoms themselves, can generalize to a fear of pain.
- Learning experiences: Fear of pain can develop through direct experiences of pain, observing others in pain, or receiving verbal information suggesting that pain is dangerous. These experiences shape negative beliefs about pain.
- Hypervigilance to pain sensations: Excessive attention to pain sensations and a tendency to interpret them as threatening to amplify fears and drive avoidance, creating a vicious cycle where hypervigilance reinforces the concern.
- Avoidance behaviors: Avoiding activities due to fear of pain prevents opportunities to challenge negative beliefs and extinguish the fear. Although avoidance provides temporary relief, it maintains long-term fear and reinforces avoidance behaviors.
Examples of fear-avoidance beliefs
Understanding and addressing these fear-avoidance beliefs, especially those involving psychosocial factors, is essential for managing and treating chronic pain conditions effectively. Examples of fear-avoidance beliefs include:
- Pain-related fear: An individual with chronic low back pain may avoid physical activity due to an intense fear that movement will exacerbate their condition, demonstrating elevated fear-avoidance beliefs.
- Exaggerated pain perception: Someone experiencing acute low back pain might catastrophize their pain, interpreting it as a sign of severe damage, thus developing initial fear-avoidance beliefs that can lead to chronic pain if not addressed.
- Fear-avoidance model: According to the fear-avoidance model, a person with chronic pain might stop engaging in activities they previously enjoyed because they believe these actions will cause further injury, reflecting the impact of psychosocial factors on pain perception.
- Identifying psychosocial variables: In physical therapy, patients with pain-related fear often report higher levels of disability.
- Psychosocial factors: Elevated fear-avoidance beliefs in patients receiving physical therapy for chronic low back pain can hinder recovery by perpetuating avoidance behaviors and exaggerated pain perception.
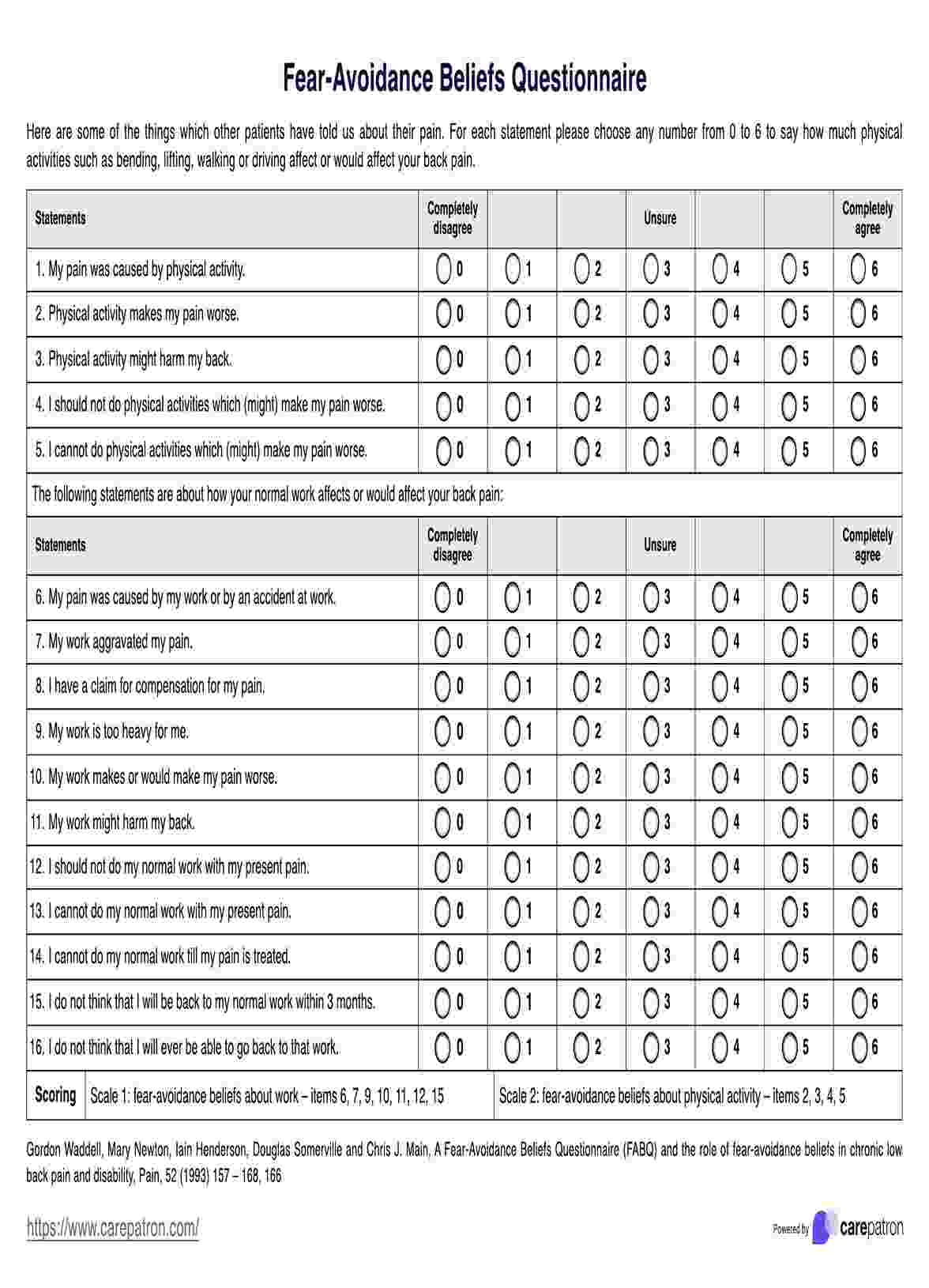
Fear-Avoidance Beliefs Questionnaire Template
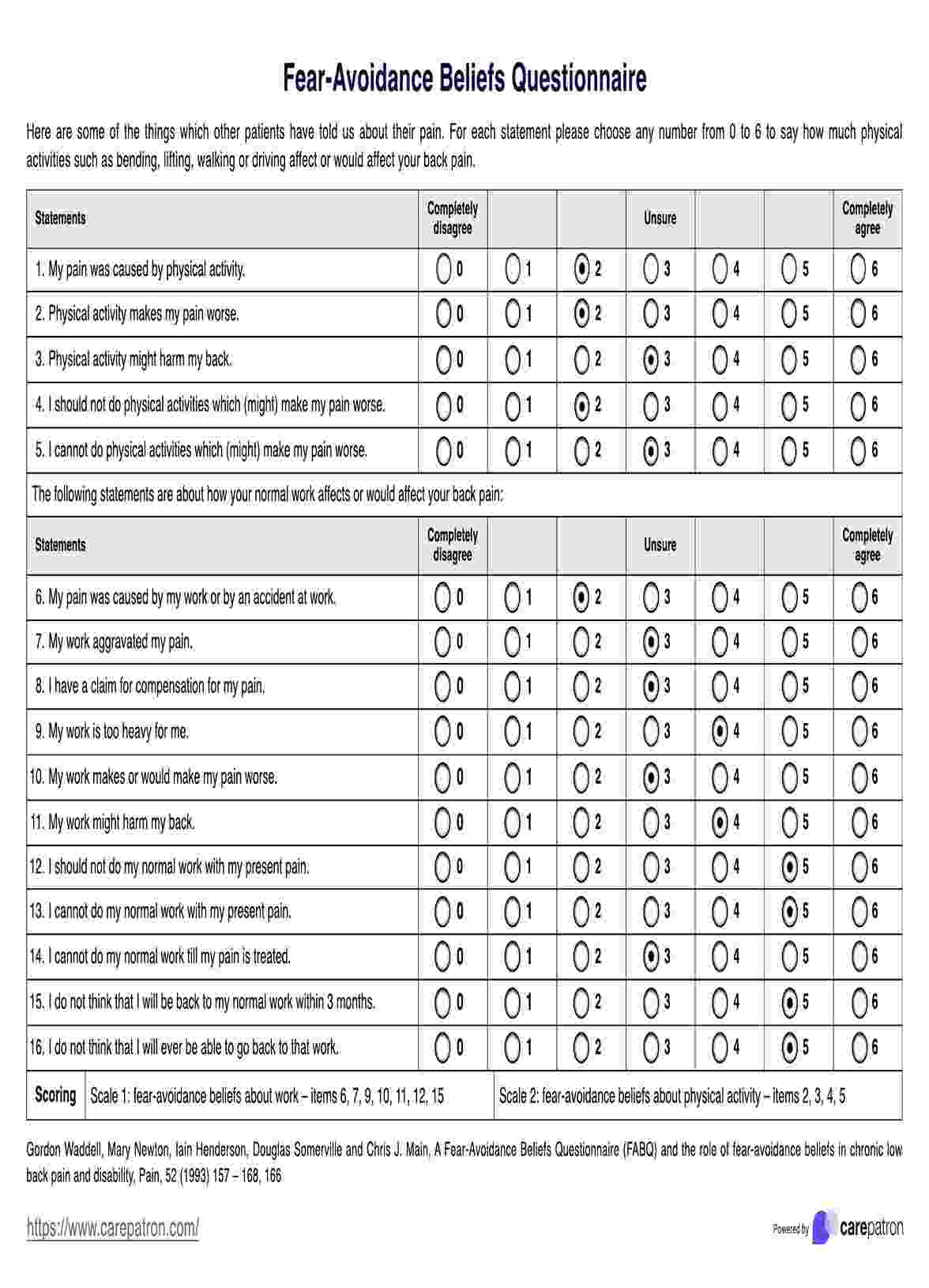
Fear-Avoidance Beliefs Questionnaire Example
What is the Fear-Avoidance Beliefs Questionnaire (FABQ)?
The FABQ was developed by Waddell et al. in 1993. It is a self-report tool designed to assess a patient's beliefs about how physical activity and work influence their low back pain (Waddell et al., 1993). It consists of 16 items, each rated on a 7-point Likert scale from 0 (completely disagree) to 6 (completely agree). Patients rate their agreement with statements regarding the impact of physical activities (items 1-5) and work (items 6-16) on their back pain.
The FABQ includes two subscales:
- FABQ-Physical Activity (FABQ-PA): This subscale consists of items 2-5 and measures fear-avoidance beliefs related to physical activity. Scores range from 0 to 24, with higher scores indicating greater fear-avoidance beliefs about physical activity.
- FABQ-Work (FABQ-W): This subscale consists of items 6, 7, 9-12, and 15, measuring fear-avoidance beliefs related to work. Scores range from 0 to 42, with higher scores indicating greater fear-avoidance beliefs about work.
Scoring and interpretation
Each item is scored on a 7-point Likert scale from 0 (completely disagree) to 6 (completely agree). The patient circles the number that best represents their agreement with each statement. To calculate the score for each subscale:
- FABQ-PA: Sum the responses for items 2-5. The score range is 0-24, with higher scores indicating higher levels of fear-avoidance beliefs related to physical activity. FABQ-PA scores >15 suggest high fear-avoidance beliefs related to physical activity.
- FABQ-W: Sum the responses for items 6,7,9-12, and 15. The score range is 0-42, with higher scores indicating higher levels of fear-avoidance beliefs related to work. FABQ-W scores >34 suggest high fear-avoidance beliefs related to work, which are associated with an increased risk of not returning to work.
Here are the next steps after scoring:
- Identify at-risk patients: Use scores to identify patients with excessive fear-avoidance beliefs who may be at risk for chronic pain and disability.
- Monitor progress: Track changes in FABQ scores over treatment to assess belief shifts, as score reductions are associated with functional improvements.
- Tailor treatment: Target problematic beliefs through interventions such as cognitive-behavioral therapy, graded exposure to feared activities, and education to reduce catastrophizing.
- Prognosis and plan return-to-work: Screen for fear-avoidance to inform prognosis and planning, mainly using the FABQ-W score.
Benefits of using this questionnaire
There are several key benefits of using the FABQ:
Identifying patients at risk
High scores on the FABQ are linked to a greater risk of chronic disability due to low back pain. This allows healthcare providers to identify patients who may be at risk of developing chronic pain and require tailored interventions.
Guiding treatment
FABQ scores can be used to inform prognosis and guide treatment planning. Patients with high fear-avoidance beliefs may benefit from targeted therapies, such as cognitive-behavioral therapy and graded exposure to physical activity. Tracking FABQ scores over time can also help monitor changes in these beliefs and adjust treatment accordingly.
Validated measure
The FABQ has proven to be a reliable and valid tool in assessing fear-avoidance beliefs in chronic low back pain populations. It correlates with other established measures of pain-related fear and disability, enhancing its credibility and utility in clinical practice.
Ease of use
The FABQ is a brief, 16-item questionnaire that takes about 10 minutes to complete. It is easy to administer and score, making it a practical and efficient tool for use in clinical settings.
References
Waddell, G., Newton, M., Henderson, I., Somerville, D., & Main, C. J. (1993). A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability.
Commonly asked questions
Fear-avoidance beliefs are prevalent among individuals with chronic pain, but the extent varies depending on factors such as pain severity, previous experiences, and psychological factors.
Yes, elevated fear-avoidance beliefs are associated with poorer treatment outcomes, including increased disability and reduced effectiveness of pain management interventions.
Patients can cope with fear-avoidance beliefs by seeking support from healthcare professionals, engaging in physical activity gradually and safely, practicing relaxation techniques, and challenging negative thoughts about pain and activity.



















-template.jpg)


















































































