DSM-5 Narcolepsy Criteria
Learn about narcolepsy and its types. Download a free DSM-5 Narcolepsy Criteria handout for your practice here.


What is narcolepsy?
Narcolepsy is a chronic neurological disorder that affects the brain's ability to regulate sleep and wakefulness. It is characterized by excessive daytime sleepiness (EDS), sudden attacks of sleep, and disrupted nocturnal sleep. People with narcolepsy may also experience other symptoms such as sleep paralysis, hallucinations, and cataplexy.
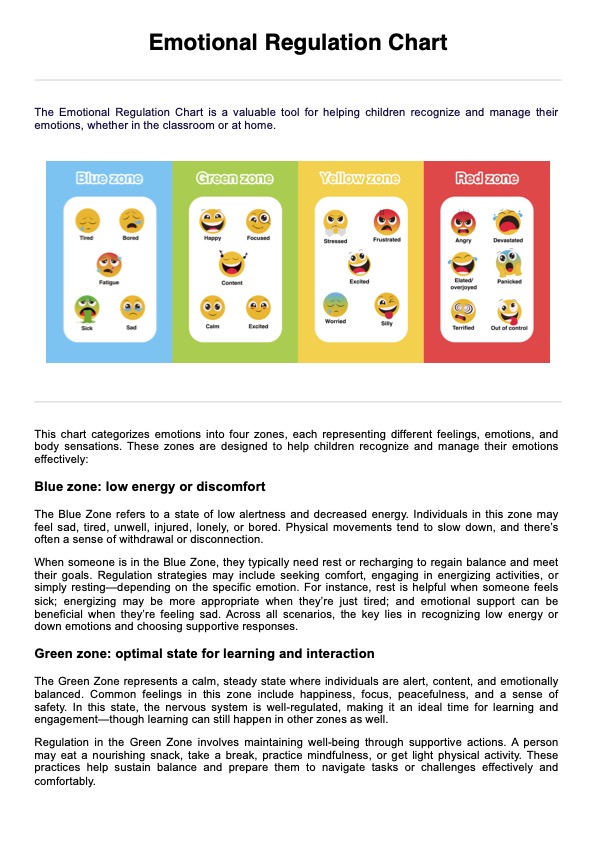
The International Classification of Sleep Disorders, 3rd Edition (ICSD-3), differentiates two subtypes of this sleep disorder (American Academy of Sleep Medicine, 2014):
- Type 1 narcolepsy (formerly known as narcolepsy with cataplexy): This diagnosis is determined either by the presence of low levels of hypocretin, a brain hormone, or by the individual experiencing cataplexy along with excessive daytime sleepiness, as confirmed by a specialized nap test.
- Type 2 narcolepsy (formerly known as narcolepsy without cataplexy): Individuals with this condition experience excessive daytime sleepiness but typically do not have muscle weakness triggered by emotions.
In addition, some rare forms of narcolepsy are autosomal dominant, meaning a person will develop the condition if they inherit a single gene from one parent. These include (MedlinePlus, 2017; Medical News Today, 2022):
- Autosomal dominant cerebral ataxia, deafness, and narcolepsy: This leads to deafness, narcolepsy, and cataplexy. This condition arises in individuals with a mutation in the DNA methyltransferase (DNMT1) gene.
- Autosomal dominant narcolepsy, type 2 diabetes, and obesity: This results in diabetes, obesity, and narcolepsy. This condition also passes from parent to child if the child inherits the single gene responsible from a parent.
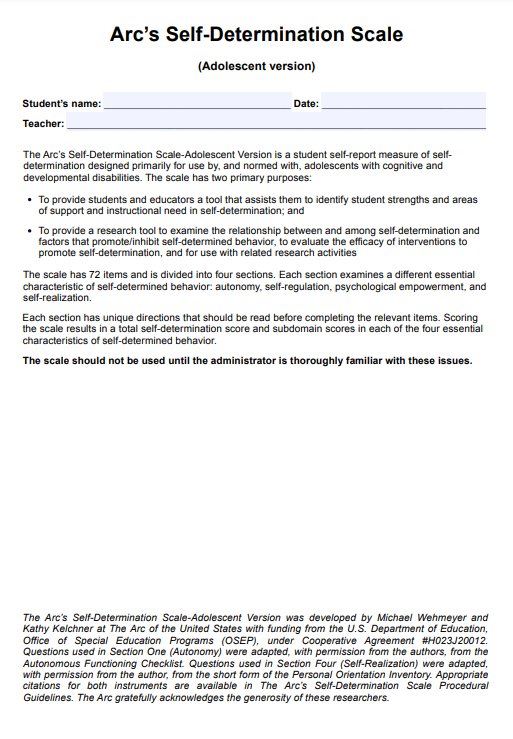
DSM-5 Narcolepsy Criteria Template
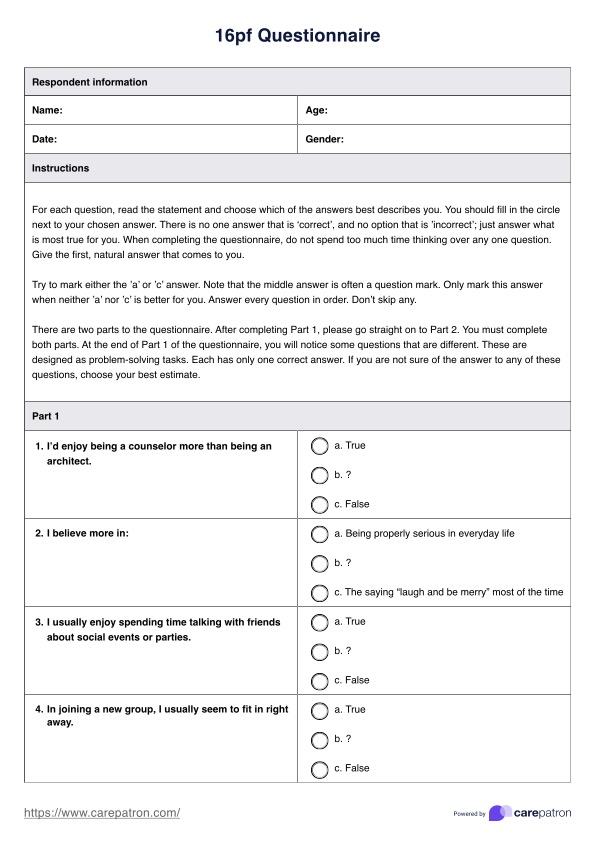
DSM-5 Narcolepsy Criteria Example
How is narcolepsy diagnosed?
Narcolepsy diagnosis can be challenging as its symptoms are similar to other sleep disorders and medical conditions. The diagnostic process involves a comprehensive evaluation:
Medical history
During a medical visit, a healthcare professional will ask about the individual's symptoms, their frequency and duration, as well as any other medical conditions or medications that could be contributing factors.
Physical examination
A physical exam may reveal signs of excessive daytime sleepiness, such as droopy eyelids or fatigue. The healthcare professional may also perform a neurological exam to look for other potential causes of the symptoms.
Sleep studies
Sleep studies are critical in diagnosing narcolepsy. These tests involve monitoring an individual's brain activity, eye movements, and muscle activity while they sleep. Two types of tests can help with the diagnosis:
- Polysomnogram (PSG): This test records an individual's brain activity, eye movements, and muscle activity while they sleep.
- Multiple sleep latency test (MSLT): This test measures how quickly someone falls asleep during the day and evaluates the tendency for REM sleep during naps.
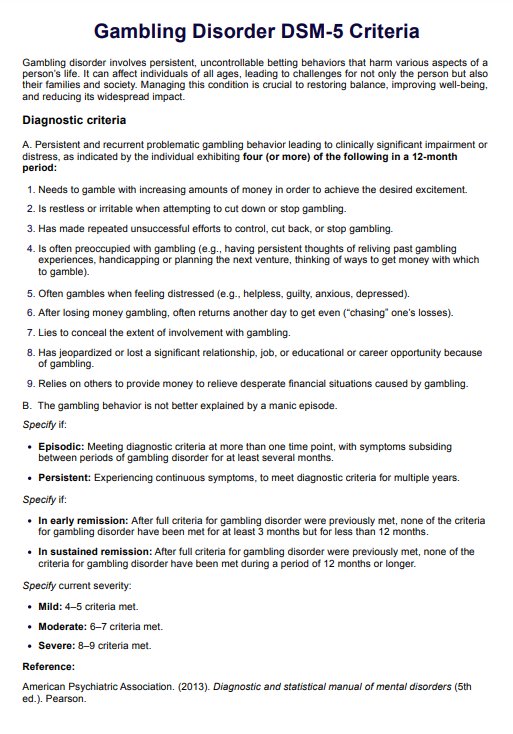
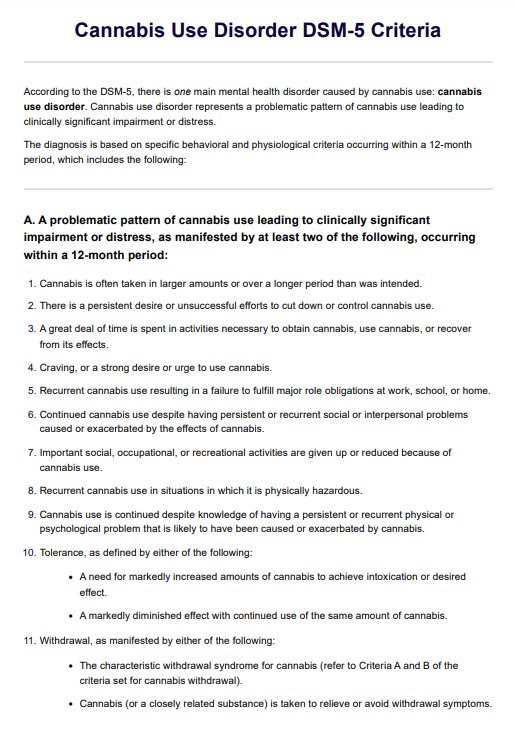
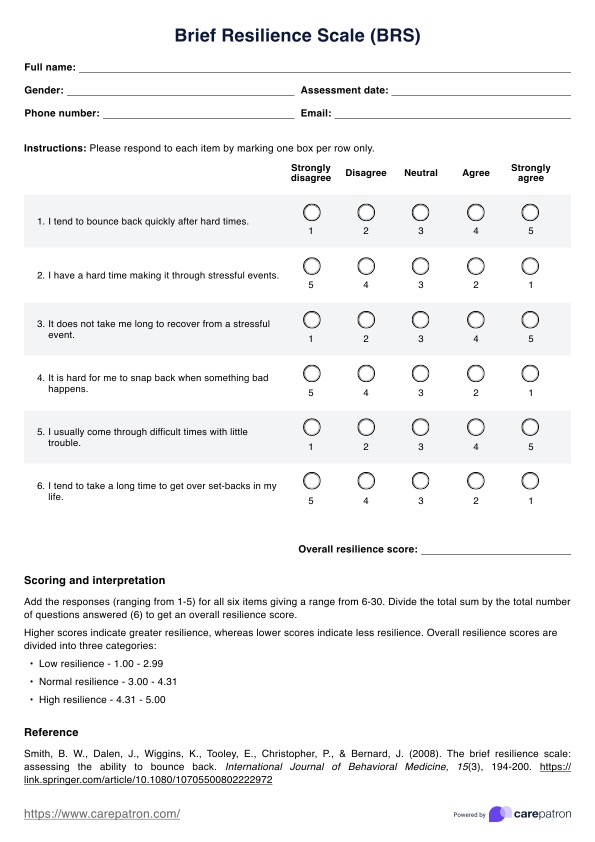
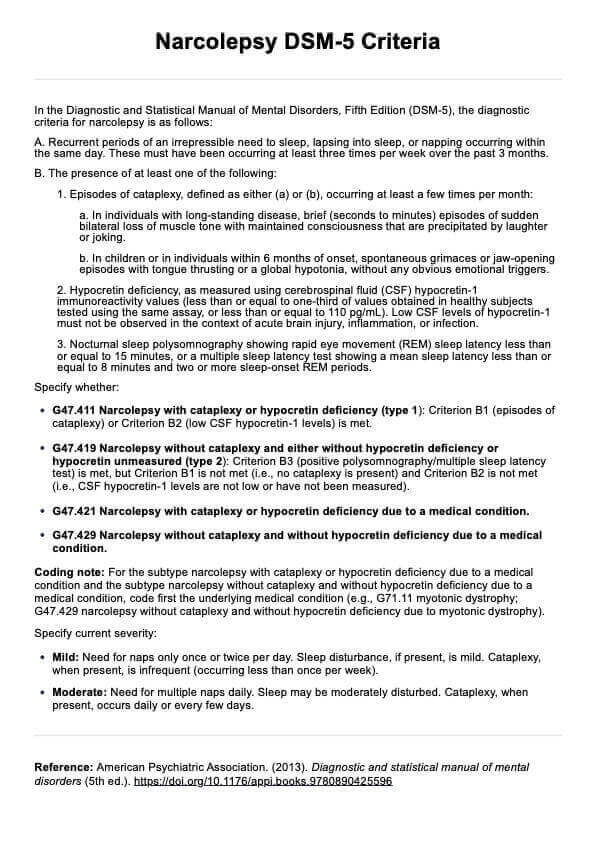
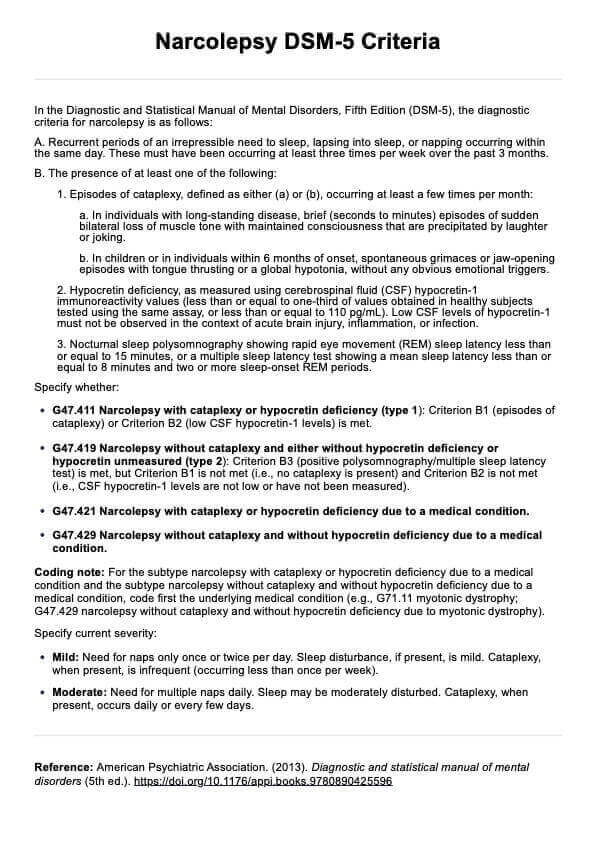
DSM-5 Narcolepsy Criteria
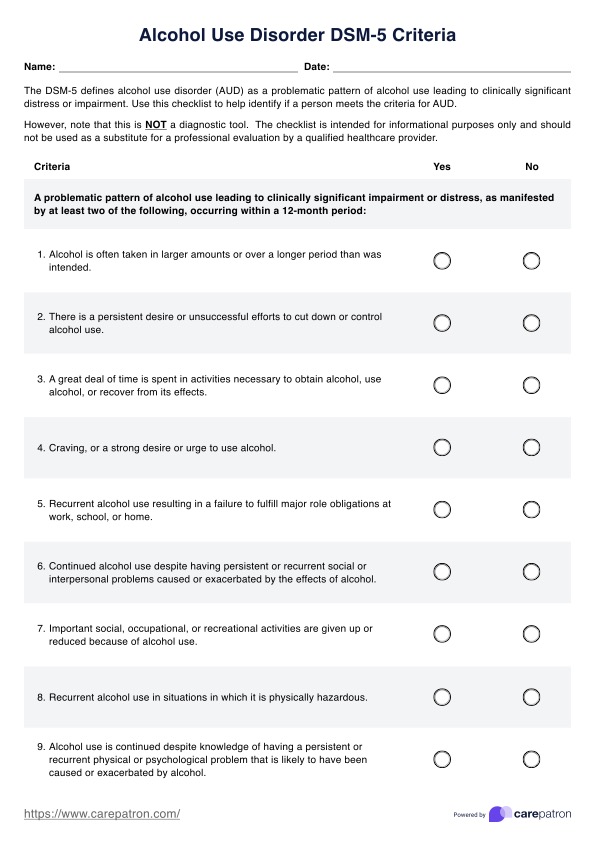
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) criteria for narcolepsy is as follows (American Psychiatric Association, 2013a):
A. Recurrent periods of an irrepressible need to sleep, lapsing into sleep, or napping occurring within the same day. These must have been occurring at least three times per week over the past 3 months.
B. The presence of at least one of the following
- Episodes of cataplexy, defined as either (a) or (b), occurring at least a few times per month:
- a. In individuals with long-standing disease, brief (seconds to minutes) episodes of sudden bilateral loss of muscle tone with maintained consciousness that are precipitated by laughter or joking.
- b. In children or in individuals within 6 months of onset, spontaneous grimaces or jaw-opening episodes with tongue thrusting or a global hypotonia, without any obvious emotional triggers.
- Hypocretin deficiency, as measured using cerebrospinal fluid (CSF) hypocretin-1 immunoreactivity values (less than or equal to one-third of values obtained in healthy subjects tested using the same assay, or less than or equal to 110 pg/mL). Low CSF levels of hypocretin-1 must not be observed in the context of acute brain injury, inflammation, or infection.
- Nocturnal sleep polysomnography showing rapid eye movement (REM) sleep latency less than or equal to 15 minutes, or a multiple sleep latency test showing a mean sleep latency less than or equal to 8 minutes and two or more sleep-onset REM periods.
Specify whether:
- G47.411 Narcolepsy with cataplexy or hypocretin deficiency (type 1): Criterion B1 (episodes of cataplexy) or Criterion B2 (low CSF hypocretin-1 levels) is met.
- G47.419 Narcolepsy without cataplexy and either without hypocretin deficiency or hypocretin unmeasured (type 2): Criterion B3 (positive polysomnography/multiple sleep latency test) is met, but Criterion B1 is not met (i.e., no cataplexy is present) and Criterion B2 is not met (i.e., CSF hypocretin-1 levels are not low or have not been measured).
- G47.421 Narcolepsy with cataplexy or hypocretin deficiency due to a medical condition.
- G47.429 Narcolepsy without cataplexy and without hypocretin deficiency due to a medical condition.
Coding note: For the subtype narcolepsy with cataplexy or hypocretin deficiency due to a medical condition and the subtype narcolepsy without cataplexy and without hypocretin deficiency due to a medical condition, code first the underlying medical condition (e.g., G71.11 myotonic dystrophy; G47.429 narcolepsy without cataplexy and without hypocretin deficiency due to myotonic dystrophy).
Specify current severity:
- Mild: Need for naps only once or twice per day. Sleep disturbance, if present, is mild. Cataplexy, when present, is infrequent (occurring less than once per week).
- Moderate: Need for multiple naps daily. Sleep may be moderately disturbed. Cataplexy, when present, occurs daily or every few days.
Differences between the DSM-4 and DSM-5 criteria
The fourth edition of the manual did not differentiate narcolepsy. In the DSM-5, narcolepsy is now recognized as being associated with hypocretin deficiency, distinguishing it from other forms of hypersomnolence (American Psychiatric Association, 2013b). This reclassification is supported by neurobiological and genetic evidence, validating the update.
How is narcolepsy treated and managed?
While there is no cure for narcolepsy, the combination of medications, lifestyle changes, and supportive measures can effectively manage the symptoms and improve the quality of life for patients
Medications
Stimulants like modafinil, armodafinil, and methylphenidate are the primary treatments to manage excessive daytime sleepiness and sleep attacks in narcolepsy. These medications help improve wakefulness and reduce episodes of sudden sleep.
Lifestyle changes
Maintaining a regular sleep schedule, taking scheduled naps, avoiding alcohol and caffeine, and engaging in regular exercise can help manage narcolepsy symptoms. Patients are advised to avoid driving or operating machinery when feeling sleepy to prevent accidents and ensure safety.
Supportive measures
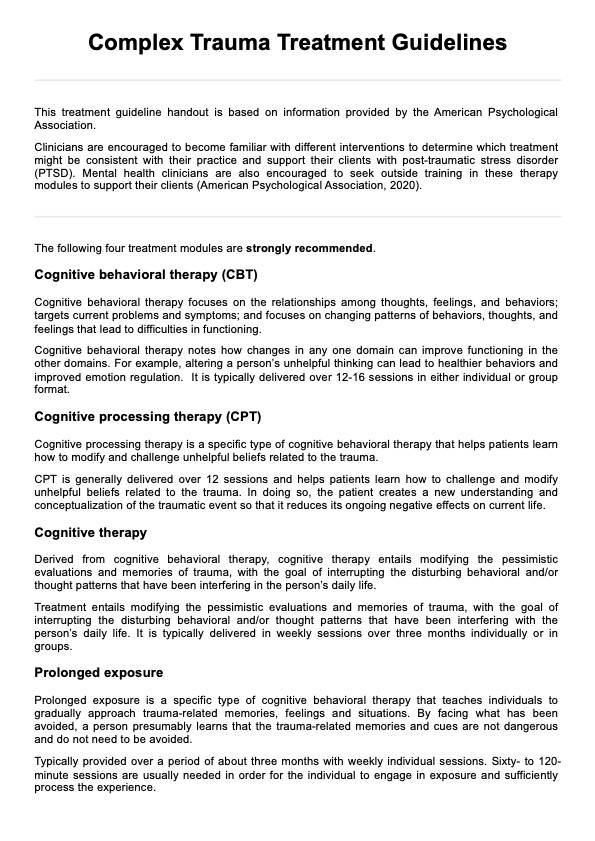
Cognitive behavioral therapy for narcolepsy (CBT-N) can complement pharmacological treatment by addressing behavioral management of symptoms. Emotional support, vocational counseling, and academic accommodations are essential to help patients cope with the psychosocial impacts of narcolepsy.
References
American Psychiatric Association. (2013a). Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596
American Psychiatric Association. (2013b). Highlights of changes from DSM-IV-TR to DSM-5. https://www.psychiatry.org/File%20Library/Psychiatrists/Practice/DSM/APA_DSM_Changes_from_DSM-IV-TR_-to_DSM-5.pdf
American Academy of Sleep Medicine. (2014). International classification of sleep disorders - third edition (ICSD-3).
Medical News Today. (2022, April 28). Is narcolepsy genetic? https://www.medicalnewstoday.com/articles/is-narcolepsy-genetic
MedlinePlus. (2017). Autosomal dominant cerebellar ataxia, deafness, and narcolepsy: MedlinePlus genetics. https://medlineplus.gov/genetics/condition/autosomal-dominant-cerebellar-ataxia-deafness-and-narcolepsy/
Commonly asked questions
Yes, narcolepsy is recognized as a Diagnostic and Statistical Manual of Mental Disorders (DSM-5) diagnosis under the category of sleep-wake disorders.
Narcolepsy consists of four classic symptoms, although not all patients experience all four: excessive daytime sleepiness (EDS), cataplexy, sleep paralysis, and hypnagogic hallucinations. Patients with narcolepsy frequently experience disturbed nocturnal sleep, meaning their nighttime sleep is often fragmented and interrupted by multiple awakenings.
Yes, narcolepsy can co-exist with other sleep-related conditions, such as obstructive sleep apnea (OSA), restless legs syndrome (RLS), and periodic limb movement disorder (PLMD). It can also be comorbid with psychiatric disorders, such as depression or anxiety.






-template.jpg)