The exact cause of OCD isn't known. Factors that may contribute include genetics, brain structure and functioning, and environmental influences such as stressful life events.
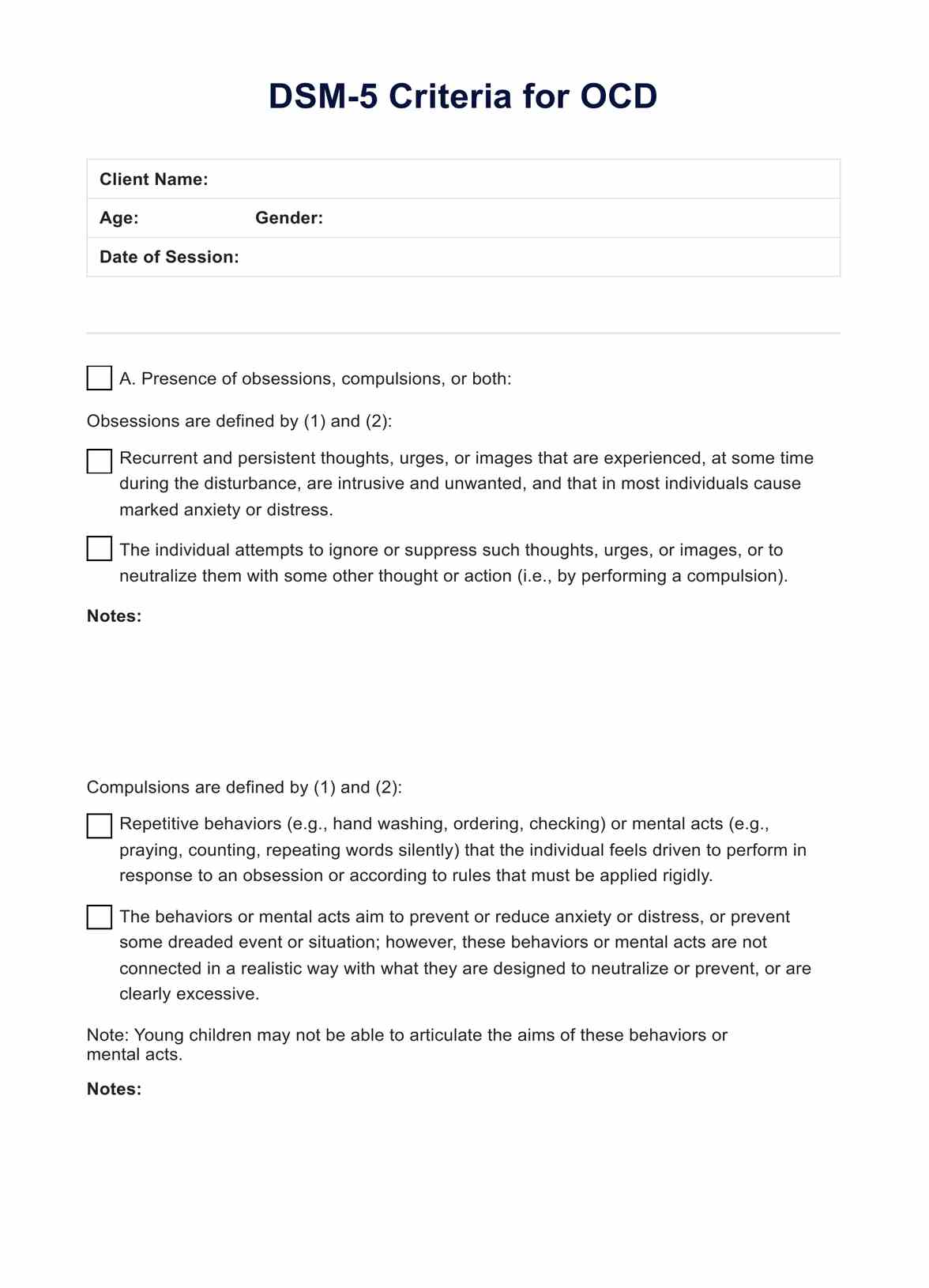
DSM 5 Criteria for OCD
Access a free resource to help you document and note possible representations of OCD when working with clients. Download your free PDF here.
Use Template
DSM 5 Criteria for OCD Template
Commonly asked questions
Yes, OCD is often concurrent with other mental health disorders, such as anxiety disorders, depression, and tic disorders.
Yes, healthy lifestyle habits such as regular exercise, a balanced diet, enough sleep, and stress management techniques can aid in managing OCD symptoms alongside traditional treatment modalities.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











