Disruptive Mood Dysregulation Disorder DSM-5 Criteria
Learn about the DSM-5 criteria for disruptive mood dysregulation disorder. Download a free PDF handout for your mental health practice.


What is disruptive mood dysregulation disorder?
Disruptive mood dysregulation Disorder (DMDD) is a mental disorder that affects children and adolescents. Severe temper outbursts and chronic irritability characterize it. Introduced in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) in 2013, DMDD is a relatively new diagnosis.
Symptoms for DMDD include persistent irritability, frequent temper outbursts, and difficulty functioning in multiple settings. These symptoms must be present for at least 12 months to receive a diagnosis. Additionally, the onset of symptoms must occur before age 10.
DMDD is often misdiagnosed as bipolar disorder due to overlapping symptoms such as mood swings and irritability. However, unlike bipolar disorder, DMDD does not involve periods of elevated or manic moods.
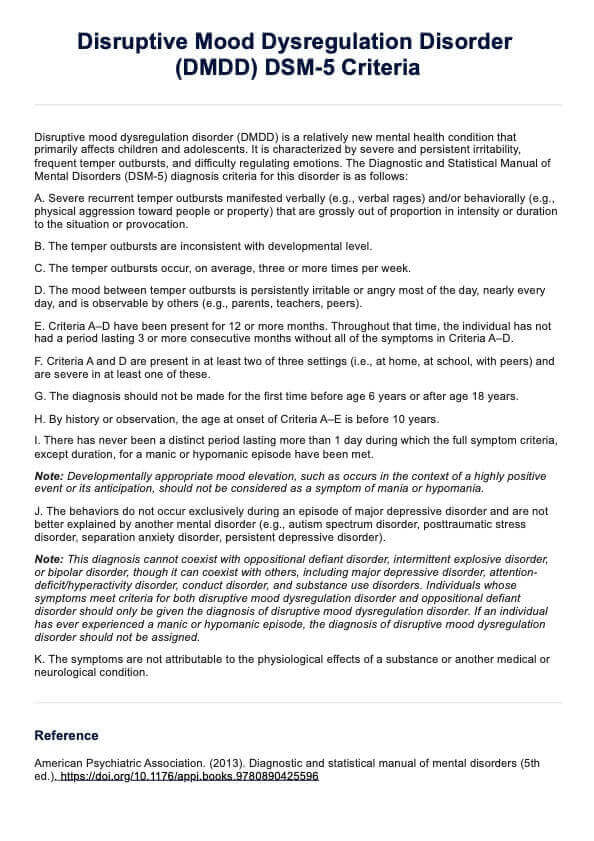
Disruptive Mood Dysregulation Disorder DSM-5 Criteria Template
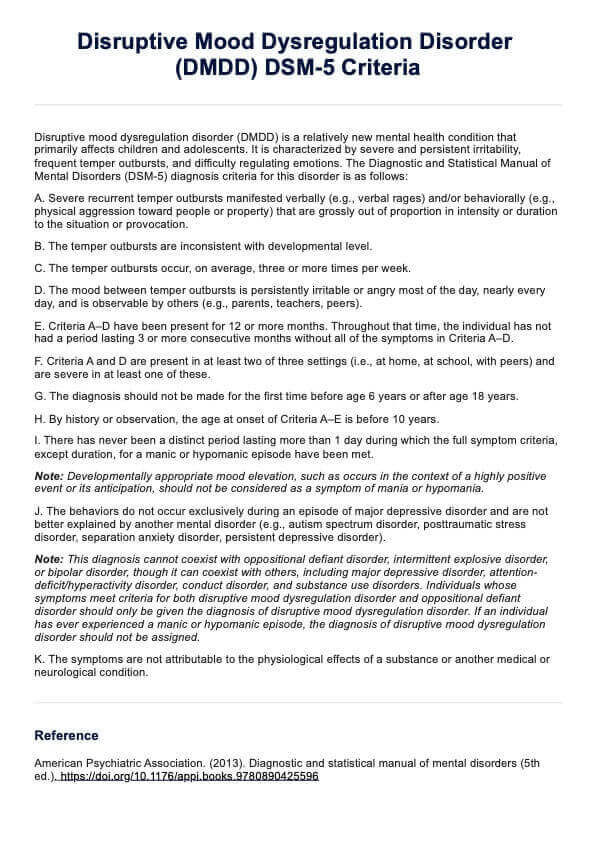
Disruptive Mood Dysregulation Disorder DSM-5 Criteria Example
How is disruptive mood dysregulation diagnosed?
DMDD involves a comprehensive evaluation by a trained mental health professional. This includes gathering information from the child, parents, teachers, and other caregivers to understand the child's symptoms and manifestation across different settings.
The professional will look for chronic irritability and severe temper outbursts disproportionate to the situation. These symptoms must be present for at least 12 months and occur in multiple settings like home and school. Additionally, it is crucial to rule out other conditions with similar symptoms, such as Autism Spectrum Disorder, Separation Anxiety Disorder, Intermittent Explosive Disorder, Posttraumatic Stress Disorder, or other mental and psychiatric disorders.
A thorough evaluation may include structured interviews, behavioral assessments, and standardized rating scales. By analyzing this information, the mental health professional can accurately diagnose and develop an effective treatment plan tailored to the child's needs.
Disruptive Mood Dysregulation Disorder DSM-5 Criteria
The DSM-5 diagnosis criteria for this disorder are as follows (American Psychiatric Association, 2013):
A. Severe recurrent temper outbursts manifested verbally (e.g., verbal rages) and/or behaviorally (e.g., physical aggression toward people or property) that are grossly out of proportion in intensity or duration to the situation or provocation.
B. The temper outbursts are inconsistent with developmental level.
C. The temper outbursts occur, on average, three or more times per week.
D. The mood between temper outbursts is persistently irritable or angry most of the day, nearly every day, and is observable by others (e.g., parents, teachers, peers).
E. Criteria A–D have been present for 12 or more months. Throughout that time, the individual has not had a period lasting 3 or more consecutive months without all of the symptoms in Criteria A–D.
F. Criteria A and D are present in at least two of three settings (i.e., at home, at school, with peers) and are severe in at least one of these.
G. The diagnosis should not be made for the first time before age 6 years or after age 18 years.
H. By history or observation, the age at onset of Criteria A–E is before 10 years.
I. There has never been a distinct period lasting more than 1 day during which the full symptom criteria, except duration, for a manic or hypomanic episode have been met.
Note: Developmentally appropriate mood elevation, such as occurs in the context of a highly positive event or its anticipation, should not be considered as a symptom of mania or hypomania.
J. The behaviors do not occur exclusively during an episode of major depressive disorder and are not better explained by another mental disorder (e.g., autism spectrum disorder, posttraumatic stress disorder, separation anxiety disorder, persistent depressive disorder).
Note: This diagnosis cannot coexist with oppositional defiant disorder, intermittent explosive disorder, or bipolar disorder, though it can coexist with others, including major depressive disorder, attention-deficit/hyperactivity disorder, conduct disorder, and substance use disorders. Individuals whose symptoms meet criteria for both disruptive mood dysregulation disorder and oppositional defiant disorder should only be given the diagnosis of disruptive mood dysregulation disorder. If an individual has ever experienced a manic or hypomanic episode, the diagnosis of disruptive mood dysregulation disorder should not be assigned.
K. The symptoms are not attributable to the physiological effects of a substance or another medical or neurological condition.
Differences between the DSM-4 and DSM-5 criteria
DMDD, or Disruptive Mood Dysregulation Disorder, was not included in the DSM-IV and was introduced in the DSM-5 to address growing concerns about the misdiagnosis of pediatric bipolar disorder.
The DSM-IV often categorized children who exhibited chronic irritability and frequent temper outbursts under pediatric bipolar disorder, even when they did not meet the specific diagnostic criteria for bipolar disorder. This misdiagnosis led to inappropriate treatments that may not have addressed the actual needs of these children.
In response, the DSM-5 introduced specific criteria for DMDD to ensure more accurate diagnosis and effective treatment. The criteria for DMDD focus on the frequency, intensity, and duration of temper outbursts and the presence of a consistently irritable or angry mood between these outbursts.
By providing a clearer diagnostic category, the DSM-5 helps clinicians differentiate between DMDD and other mood disorders, thereby improving the quality of care for affected children and reducing the risk of misdiagnosis and inappropriate interventions.
How is disruptive mood dysregulation disorder treated?
Treating DMDD typically involves a combination of psychotherapy and medication. The treatment approach is tailored to the individual child's needs and the severity of their symptoms.
Treatment options
Psychotherapy (talk therapy) includes cognitive-behavioral therapy (CBT), which helps children learn to manage their emotions and behaviors more effectively. Family therapy involves working with the child and their family to improve communication and problem-solving skills, and individual therapy focuses on helping the child develop coping strategies and improve their emotional regulation.
Medications include stimulants, used to treat symptoms of attention deficit hyperactivity disorder (ADHD) if present. Antidepressants may be prescribed to help manage irritability and mood symptoms, and antipsychotics are sometimes used to manage severe symptoms, but their use is generally limited due to potential side effects.
Treatment goals
The goals include improving emotional regulation by helping children learn to manage their emotions and behaviors more effectively, reducing irritability and anger by addressing the chronic irritability and anger that is a hallmark of DMDD and enhancing functioning by improving the child's ability to function well in various settings, such as at home, school, and with peers.
Treatment challenges
Challenges include differentiating DMDD from other disorders, as it can be difficult to distinguish from conditions like ADHD, oppositional defiant disorder (ODD), anxiety disorders, and childhood bipolar disorder, and the lack of specific treatments since DMDD is a relatively new diagnosis, leading to treatments often being adapted from those used for other conditions.
Prognosis
With proper treatment, children with DMDD can improve their symptoms and function better. Many children with DMDD tend to outgrow their symptoms by adulthood, although some may continue to experience some residual symptoms.
Reference
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596
Commonly asked questions
Children with DMDD often present with comorbid conditions such as ADHD, anxiety disorders, and major depressive disorder. Assessing and addressing these comorbidities is essential for providing comprehensive care.
Effective treatment for DMDD typically involves a combination of Cognitive Behavioral Therapy (CBT), parent management training, and possibly pharmacological interventions such as stimulants, SSRIs, or antipsychotics.
Providing psychoeducation about DMDD, guiding parents in implementing consistent behavioral strategies, and connecting families to support groups and resources can significantly aid in managing the disorder.
DMDD was introduced to address the need for a more accurate diagnosis for children with chronic irritability and frequent temper outbursts, reducing the misdiagnosis of pediatric bipolar disorder. This change has helped clinicians tailor interventions more appropriately.

.jpg)
















-template.jpg)



















































































