Developmental Coordination Disorder DSM-5 Criteria
Learn about the DSM-5 criteria for developmental coordination disorder and explore examples in this informative guide. Download Carepatron's free PDF for reference.


What is developmental coordination disorder?
Developmental coordination disorder (DCD), as defined by the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), is a neurological condition affecting movement. Children with early developmental period typically exhibit a motor skills deficit in coordinated motor skills, which can manifest early in the developmental period. These motor coordination difficulties often persist into adolescence and adulthood.
Individuals with DCD may struggle with tasks requiring fine motor skills, such as writing, tying shoelaces, or using utensils. This condition is not attributable to intellectual disability or a pervasive developmental disorder but rather represents a specific impairment in coordinated motor skills.
The developmental coordination disorder questionnaire outlines specific diagnostic criteria for DCD, emphasizing that the motor skills deficits significantly interfere with academic achievement or activities of daily living. Early recognition and intervention are crucial to help affected individuals improve their motor skills and adapt to educational, prevocational, and vocational activities.
Developmental Coordination Disorder DSM-5 Criteria Template
Developmental Coordination Disorder DSM-5 Criteria Sample
How is Developmental Coordination Disorder diagnosed?
Diagnosing DCD involves a comprehensive evaluation integrating developmental coordination and medical history, physical examination, and standardized assessments in early developmental period. Clinicians rely on psychometrically validated tests that are culturally appropriate to assess impaired motor coordination skills, which may manifest differently across age groups.
For young children with developmental coordination issues like sitting, crawling, and walking may be observed, although many achieve these milestones within typical timeframes. Difficulties may persist in tasks such as using utensils, buttoning shirts, or completing puzzles, often characterized by awkward or imprecise movements. In older children and adults, challenges may affect activities requiring motor coordination, such as handwriting, sports participation, or daily tasks like dressing and using tools.
Developmental coordination disorder is diagnosed if these motor impairments significantly interfere with daily activities in family, social, educational, or community settings. It excludes conditions like visual impairment or other degenerative disorder through specific examinations. Although there are no subtypes, individuals may exhibit predominant difficulties in gross or motor skills, affecting aspects of academic and vocational performance.
This diagnostic process ensures appropriate support and intervention tailored to the individual's needs, enhancing their ability to navigate daily challenges effectively.
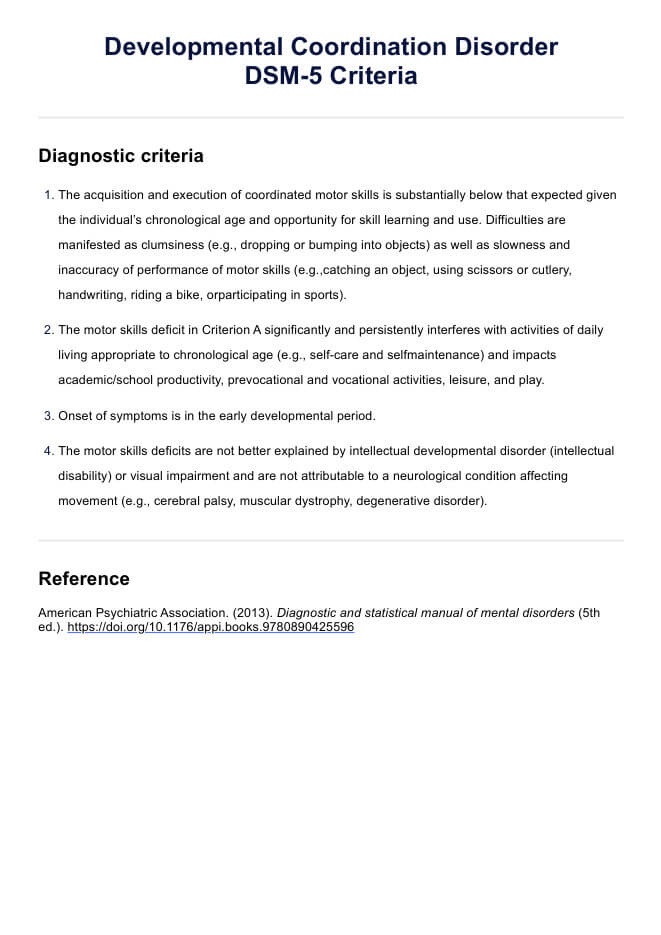
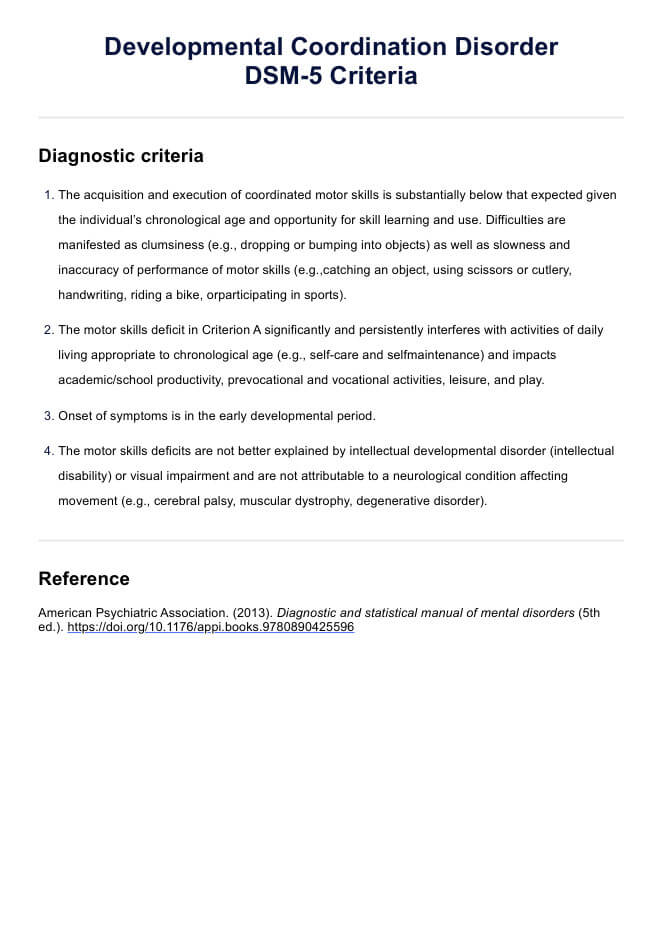
Developmental Coordination Disorder DSM-5 Criteria
According to the DSM-5, DCD is diagnosed based on specific criteria (Amercian Psychiatric Association, 2013a):
- The acquisition and execution of coordinated motor skills is substantially below that expected given the individual’s chronological age and opportunity for skill learning and use. Difficulties are manifested as clumsiness (e.g., dropping or bumping into objects) as well as slowness and inaccuracy of performance of motor skills (e.g.,catching an object, using scissors or cutlery, handwriting, riding a bike, orparticipating in sports).
- The motor skills deficit in Criterion A significantly and persistently interferes with activities of daily living appropriate to chronological age (e.g., self-care and selfmaintenance) and impacts academic/school productivity, prevocational and vocational activities, leisure, and play.
- Onset of symptoms is in the early developmental period.
- The motor skills deficits are not better explained by intellectual developmental disorder (intellectual disability) or visual impairment and are not attributable to a neurological condition affecting movement (e.g., cerebral palsy, muscular dystrophy, degenerative disorder).
Differences between the DSM-4 and DSM-5 criteria
In the previous edition of the manual, developmental coordination disorder was classified under the broad category of "learning disorders." In DSM-5, it has been reclassified as a motor disorder within the broader category of "neurodevelopmental disorders" (American Psychiatric Association, 2013b; Harris et al., 2015).
How is DCD treated?
Treatment for Developmental Coordination Disorder (DCD) focuses on addressing the specific challenges individuals face with motor skills deficits. Various approaches can help improve functioning and quality of life for those affected.
Occupational therapy
Occupational therapy plays a crucial role in DCD treatment, focusing on enhancing motor skills through targeted exercises and activities. Therapists use specialized techniques to improve coordination, fine motor skills, and adaptive strategies for daily tasks.
Physical therapy
Physical therapy aims to strengthen muscles, improve balance, and enhance overall physical coordination. Therapists work on specific motor tasks and activities to promote better movement patterns and reduce clumsiness.
Cognitive-behavioral therapy (CBT)
CBT can help individuals manage anxiety or frustration related to DCD challenges. It teaches coping strategies, boosts self-esteem, and addresses psychological aspects that may accompany motor skill difficulties.
Educational support
School-based interventions provide accommodations and modifications to support academic performance. This includes assistive technology, extended time for assignments, and strategies for classroom participation.
Parent and teacher education
Educating parents and teachers about DCD helps create a supportive environment. Strategies for home and school settings can enhance skill learning and participation in activities like prevocational and vocational activities, promoting independence and social inclusion.
Multidisciplinary approach
A comprehensive treatment plan often involves collaboration among occupational therapists, physical therapists, educators, and psychologists. This holistic approach addresses the diverse needs of individuals with neurodevelopmental disorders, fostering optimal development and participation in daily life and according to the individual's chronological age.
References
American Psychiatric Association. (2013a). Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596
American Psychiatric Association. (2013b). Highlights of Changes from DSM-IV-TR to DSM-5. https://www.psychiatry.org/File%20Library/Psychiatrists/Practice/DSM/APA_DSM_Changes_from_DSM-IV-TR_-to_DSM-5.pdf
Harris, S. R., Mickelson, E. C. R., & Zwicker, J. G. (2015). Diagnosis and management of developmental coordination disorder. Canadian Medical Association Journal, 187(9), 659–665. https://doi.org/10.1503/cmaj.140994
Commonly asked questions
Yes, Developmental Coordination Disorder (DCD) is included in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), providing standardized criteria for diagnosis.
The diagnostic criteria include significant impairment in motor coordination, impacting daily activities, with onset in the early developmental period, and not attributable to other conditions affecting movement or intellectual disability.
The diagnosis code for Developmental Coordination Disorder (DCD) in the International Classification of Diseases (ICD-10) is F82.
Yes, developmental coordination disorder (DCD) is often referred to as dyspraxia, although the terms are used interchangeably in many contexts to describe difficulties with motor coordination and skills.


















-template.jpg)


















































































