Depression Self-Assessment
Explore our comprehensive guide on the Depression Self-Assessment, designed for mental health professionals to evaluate and manage depression effectively.


An introduction to clinical depression
Clinical depression, also known as major depressive disorder, is a common and serious medical illness that negatively affects how you feel, the way you think, and how you act. The American Psychiatric Association (APA) defines it in the Diagnostic and Statistical Manual of Mental Disorders (DSM) as a disorder characterized by persistent feelings of sadness and a lack of interest in external stimuli.
Clinical depression is widespread, affecting millions of people worldwide. The World Health Organization estimates it as a leading cause of disability. It's not just feeling sad; it's a debilitating condition that can significantly impair a person's ability to function in daily life.
Common symptoms of clinical depression include a persistent sad, anxious, or "empty" mood, feelings of hopelessness or pessimism, irritability, feelings of guilt, worthlessness, or helplessness, loss of interest in hobbies and activities, decreased energy or fatigue, difficulty concentrating, remembering, or making decisions, insomnia, early-morning wakefulness, or oversleeping, appetite and weight changes, thoughts of death or suicide, suicide attempts, and aches or pains, headaches, cramps, or digestive problems without a clear physical cause and that do not ease even with treatment.
The causes of clinical depression are varied and often a combination of genetic, biological, environmental, and psychological factors. Traumatic events, major life changes, certain medications, and other mental health disorders can also contribute to its development.
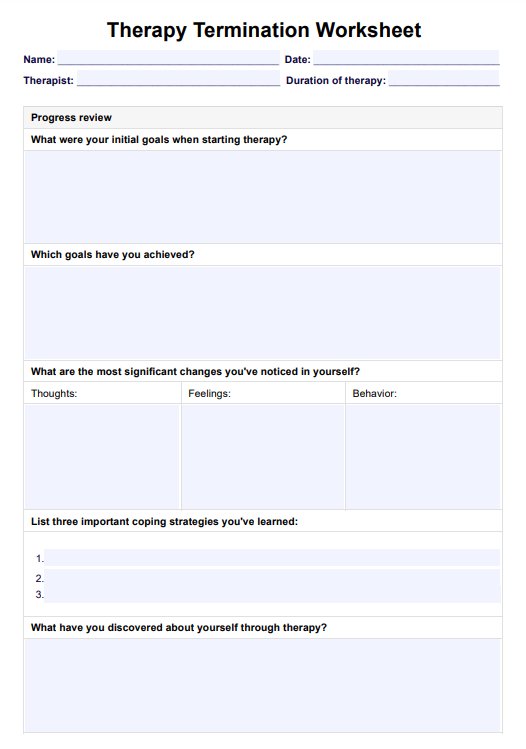
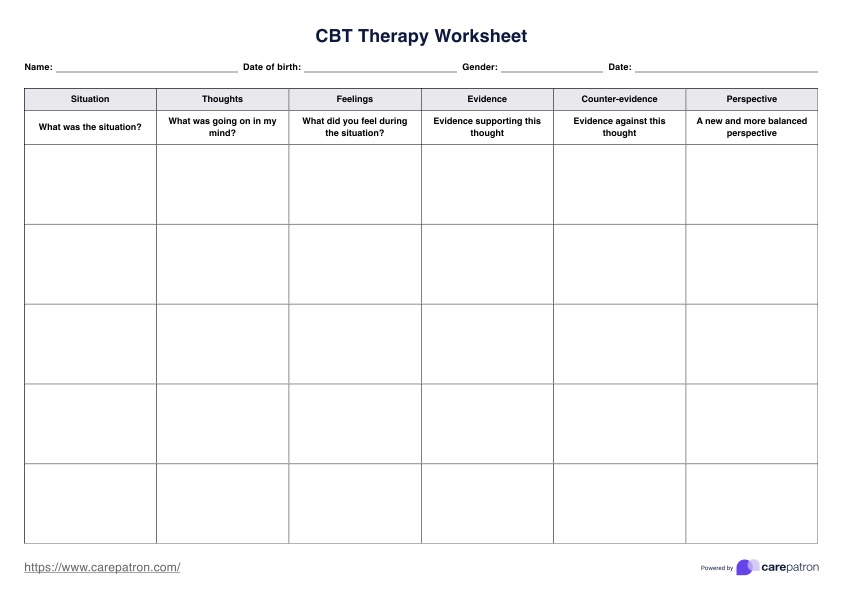
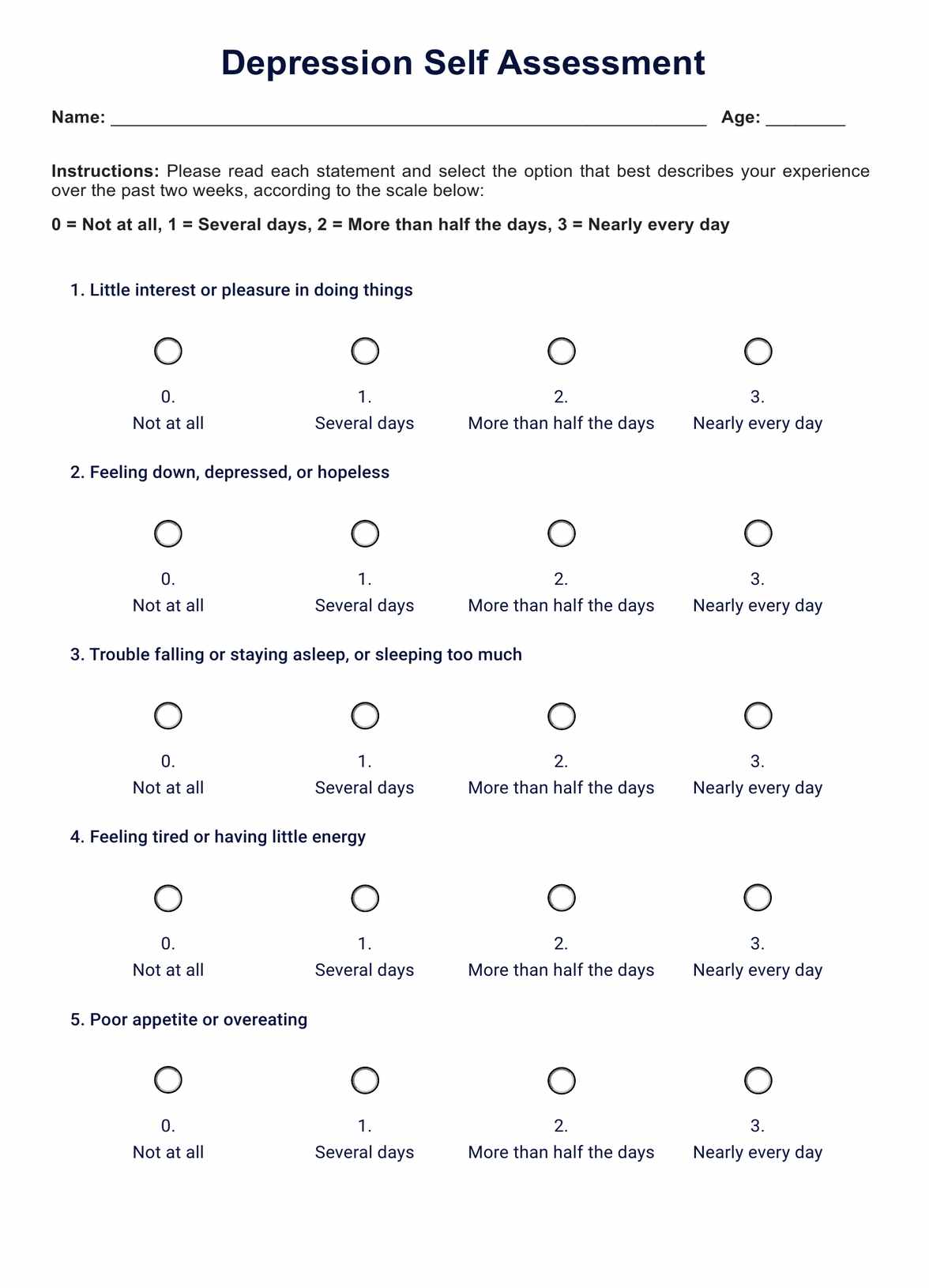
Depression Self-Assessment Template
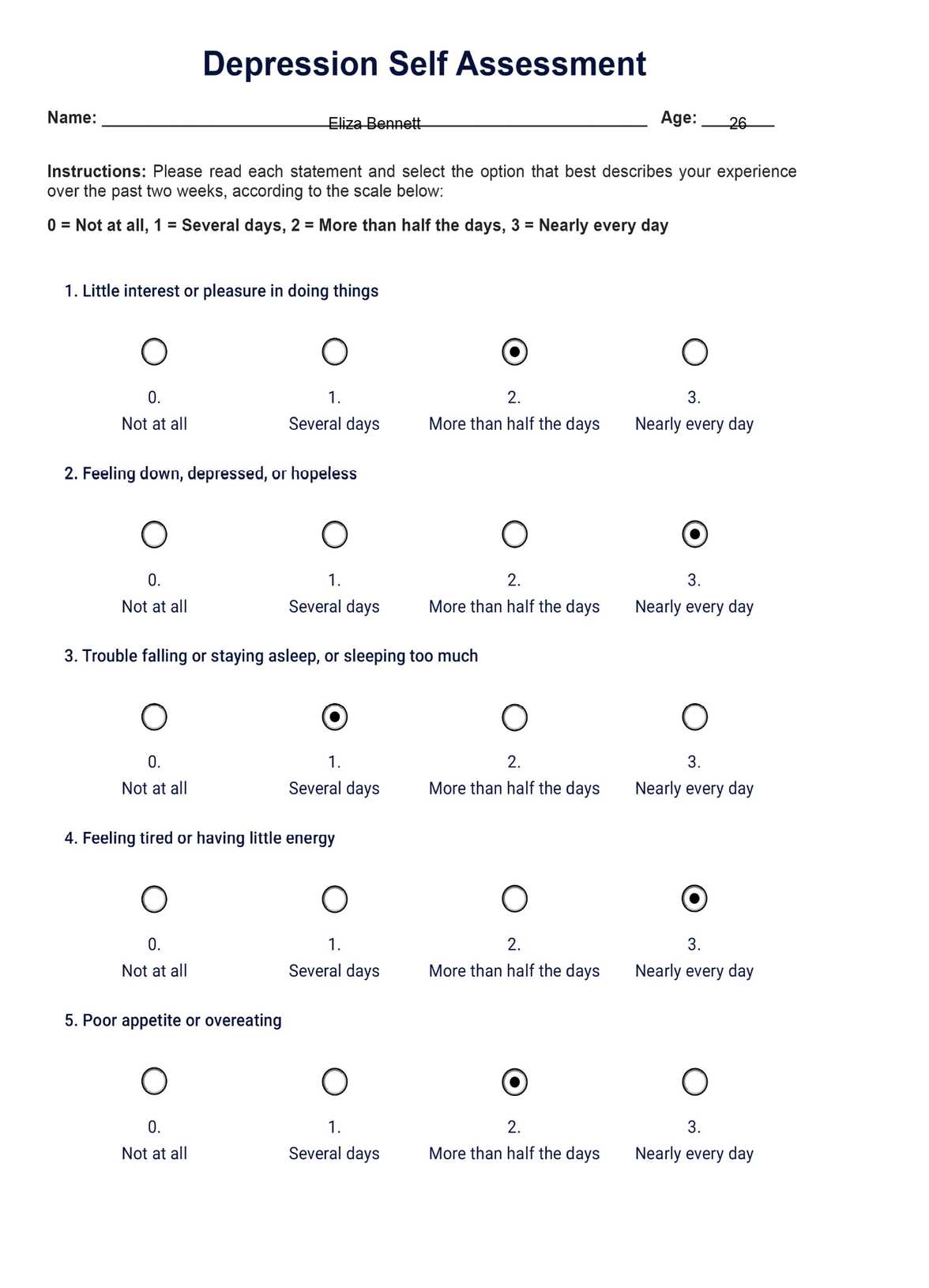
Depression Self-Assessment Example
Symptoms and signs of depression
Depression manifests through a range of symptoms that affect a person's emotional state, thought processes, and physical well-being. It's important to recognize these symptoms for early intervention and effective treatment. Here are some of the signs that also appear in the Major Depression Inventory:
- Persistent sadness or feeling of emptiness: This is more than just feeling blue; it's a deep, prolonged sense of sadness or emptiness that doesn't seem to go away.
- Loss of interest or pleasure: The patient may have little interest in daily activities. Activities or hobbies that once brought joy may no longer feel enjoyable or fulfilling.
- Changes in appetite or weight: This can include significant weight loss when not dieting, weight gain, or changes in appetite.
- Sleep disturbances: This includes trouble sleeping or sleeping too much, resulting in the person feeling like they have little energy.
- Fatigue or loss of energy: Feeling tired most of the time, even without physical exertion, is a common sign.
- Feelings of worthlessness or excessive guilt: This involves harsh criticism of oneself for perceived faults and mistakes.
- Difficulty thinking, concentrating, or making decisions: People with depression often find it hard to focus or make decisions, even about small, everyday things.
- Recurrent thoughts of death or suicide: This includes suicidal ideation without a specific plan, a suicide attempt, or a detailed plan for committing suicide.
- Irritability or restlessness: Feeling agitated, restless, or even violent; the tolerance level is low, temper short, and everything and everyone gets on the nerves.
- Physical symptoms: Unexplained aches or pains, headaches, cramps, or digestive problems that do not ease with treatment.
Recognizing these signs is the first step toward seeking help. If you or someone you know is showing several of these symptoms, it may be time to consult a mental health professional for a proper assessment and possible treatment.
When should your patients seek assessment?
Healthcare professionals must guide their patients on when to seek a depression assessment. Recognizing the right time to get help can significantly impact the effectiveness of treatment and the overall recovery process.
Prolonged negative emotions
If a patient experiences persistent sadness, hopelessness, or a lack of interest in activities for more than two weeks, it's a clear indicator that an assessment is needed.
Impact on daily life
When symptoms of depression start to affect a person's work, social life, or family responsibilities, it's important to seek professional help. This includes struggling with daily tasks, concentrating, withdrawing from social interactions, or having difficulty maintaining relationships.
Physical health concerns
Suppose a patient reports physical symptoms, such as chronic pain, sleep disturbances, or changes in appetite and weight. In that case, that cannot be attributed to other medical conditions; a depression assessment may be warranted.
Increased use of substances
Turning to alcohol, drugs, or other substances as a coping mechanism for emotional distress is a red flag. This behavior often exacerbates depressive symptoms and indicates the need for a comprehensive assessment.
Suicidal thoughts or behaviors
Any indication of suicidal thoughts or behaviors warrants immediate assessment. This is a critical situation where prompt intervention can be life-saving.
Previous mental health issues
Patients with a history of mental health issues, including prior episodes of depression, should be closely monitored for recurring symptoms and encouraged to undergo periodic assessments.
Healthcare professionals should encourage patients to be open about their symptoms and experiences. Regular check-ins and discussions about mental health can help identify when an assessment for depression is necessary. Early intervention is critical to managing depression effectively. You can start with a patient health questionnaire if your patient needs an evaluation.
How does this self-assessment work?
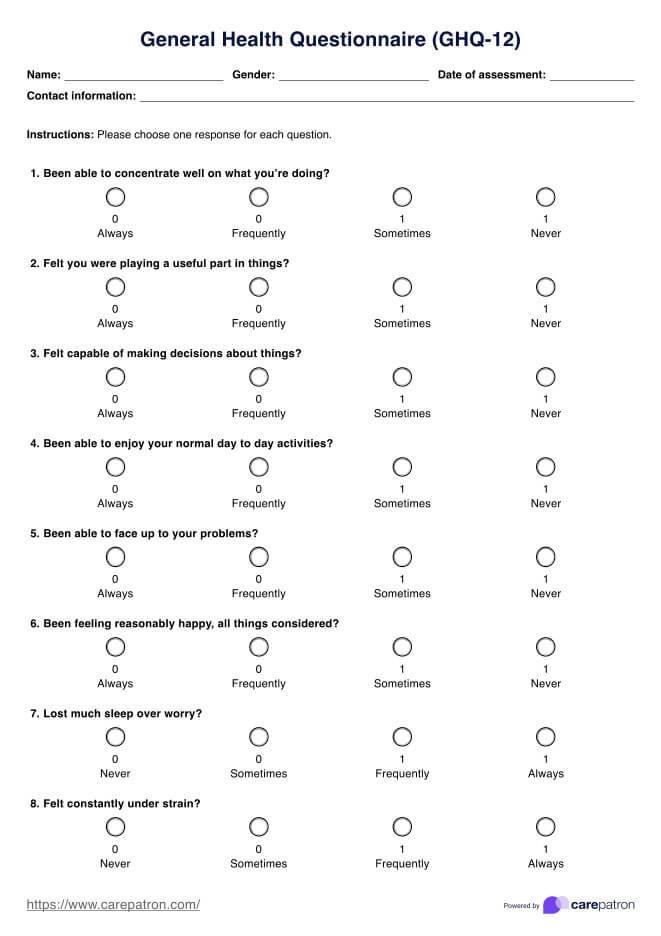
For healthcare professionals, guiding patients through the depression self-assessment process is an essential step in recognizing and addressing mental health concerns. Here's how you can effectively use our free template, which combines elements from the Beck Depression Inventory, Mental Health America's depression self-assessment test, and the WHO's depression self-assessment test:
Step 1: Access our template
Access the printable Depression Self-Assessment Template through the Carepatron app. It's designed to be comprehensive yet straightforward, ensuring ease of use for healthcare professionals and patients. You can share it with your patients by printing it or sending it to them via the app.
Step 2: Explain the template to the patient
Clearly explain the purpose and method of the self-assessment. Emphasize the importance of honesty in responses to reflect their mental state accurately. Ensure they understand the rating scale from "Not at all" to "Nearly every day."
Step 3: Patient completes the assessment
Ask the patient to complete the assessment, marking the frequency of their symptoms over the past two weeks. Encourage them to reflect on each question and consider their experiences carefully.
Step 4: Review and interpret the results
Once completed, review the results with the patient. Discuss the total score and what it may suggest about their mental health. The interpretation should be a starting point for a deeper conversation about their well-being.
Step 5: Discuss the next steps based on the assessment
Depending on the outcome of the assessment, discuss possible next steps. This might include further evaluation, therapy options, or strategies to manage symptoms.
Step 6: Regular follow-up
Schedule regular follow-ups to monitor any changes in their symptoms or overall mental health. This ongoing support is crucial in managing depression effectively.
By incorporating this self-assessment into your practice, you can help patients gain insight into their mental health and take proactive steps toward managing depression.
Understanding the results
Understanding the results of the Depression Self-Assessment is crucial for both healthcare professionals and patients. This assessment quantifies the severity of depressive symptoms, offering guidance on the potential level of clinical depression. Scores range from minimal to severe depression, providing a preliminary gauge of the patient's mental state.
For instance, a score between 5-9 suggests mild depression, while a score above 20 indicates severe depression. It's important to note that this self-assessment is not a definitive diagnosis but a starting point for further exploration and conversation about mental health.
Healthcare professionals should use these results to guide discussions with their patients about their emotional well-being and possible treatment options or referrals for a more in-depth evaluation.
Treatment and next steps
After identifying potential depression through self-assessment or other ways such as the Depression Screening Test, it's vital to consider the next steps for treatment and management. Here are some guidelines:
Seek professional help
If the self-assessment indicates mild to severe depression, it's essential to consult a mental health care professional. They can provide a more comprehensive evaluation and confirm a diagnosis. For example, a healthcare provider might use additional tools like the Hamilton Depression Rating Scale or conduct an in-depth interview to understand the patient's condition better.
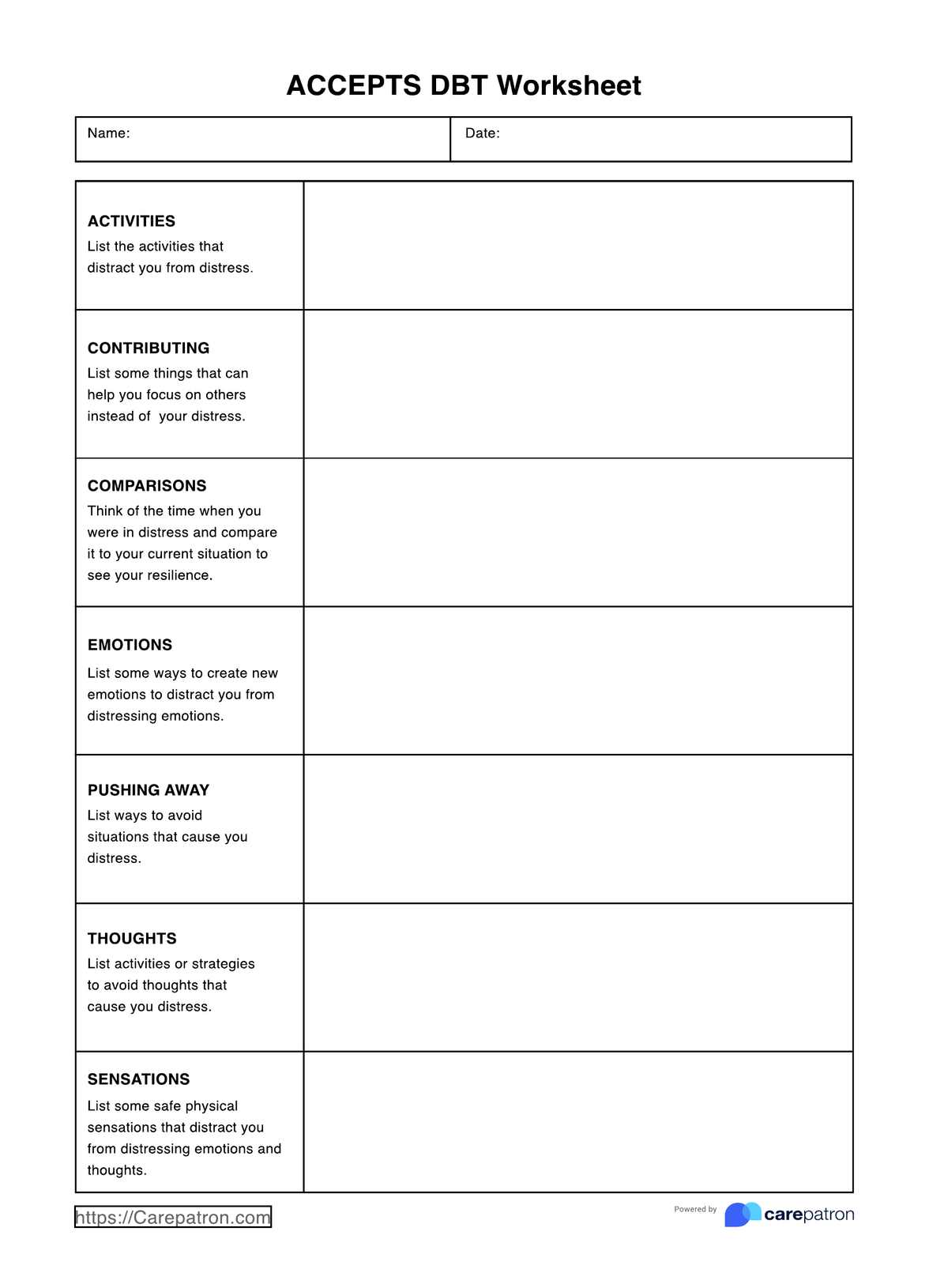
Consider therapy options
Various types of therapy, such as cognitive-behavioral therapy (CBT) or interpersonal therapy, can be effective in treating depression. These therapies help patients understand and change negative thought patterns and develop coping strategies. For instance, CBT can assist a patient in challenging irrational beliefs contributing to their depression.
Explore medication
In some cases, antidepressants may be prescribed to help manage symptoms. These medications can balance chemicals in the brain that affect mood. However, they should be taken under the guidance of a healthcare professional, considering potential side effects and interactions.
Lifestyle changes
Incorporating healthy lifestyle choices can significantly impact mental health. Regular exercise, a balanced diet, adequate sleep, and stress-reducing activities can improve overall well-being. For example, engaging in physical activities like yoga or mindfulness meditation can help alleviate symptoms of depression.
Social support
Building a strong support system is crucial. Encourage patients to stay connected with family and friends and consider joining support groups where they can share experiences and coping strategies with others facing similar challenges.
Ongoing monitoring
Depression can be a recurring condition, so ongoing monitoring and treatment adjustments are essential. Regular check-ins with a mental health professional can ensure that the treatment plan remains effective and is adjusted as needed.
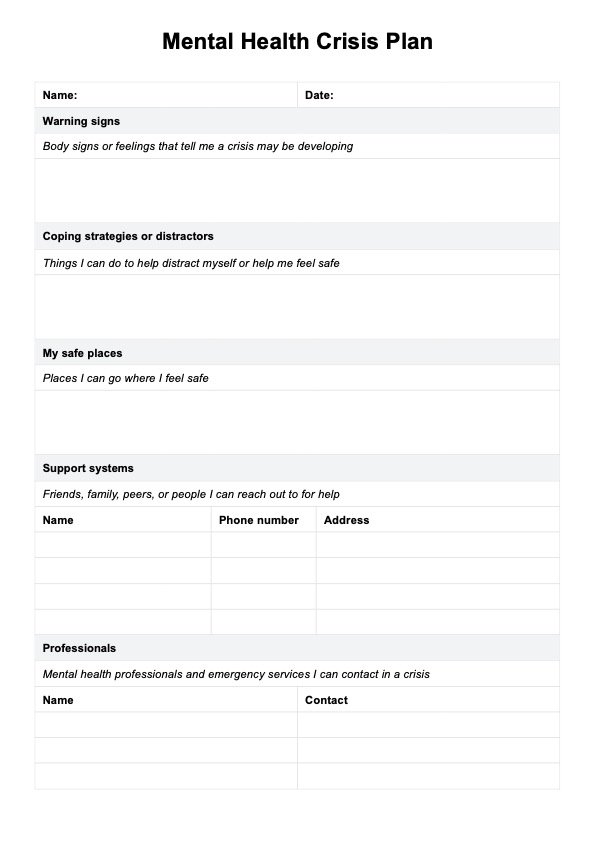
Emergency planning
In cases of severe depression, especially if there are thoughts of self-harm or suicide, it's crucial to have an emergency plan in place. This may include crisis hotline numbers, emergency contact information, and a safety plan.
These steps provide a roadmap for individuals who may be experiencing depression, guiding them toward appropriate treatment and support. It's important to remember that recovery from depression is a journey, often requiring patience and a combination of different treatment methods, even necessitating the use of a Depression Nursing Care Plan.
Commonly asked questions
Critical questions for depression assessment include inquiries about mood, interest in activities, sleep patterns, appetite, energy levels, and thoughts of self-harm.
Depression often leads to reduced social interaction, trouble falling or staying asleep, poor appetite, difficulty focusing, and diminished motivation.
Depression can change how a person feels and behaves, often resulting in increased sadness, withdrawal, and a negative outlook, but it doesn't permanently alter personality.


















-template.jpg)