Depersonalization Disorder Test
Access a free Depersonalization Disorder Test to screen for the possible presence of symptoms and the disorder among clients.


What is depersonalization-derealization disorder (DPDR)?
Depersonalization-derealization disorder (DPDR) is a complex mental health condition characterized by persistent or recurrent feelings of detachment from one's thoughts, emotions, body, or surroundings. Individuals with DPDR often describe feeling as if they're observing themselves from outside their body or perceiving the world around them as unreal or dreamlike.
Depersonalization-derealization symptoms
DPDR is classified as a dissociative disorder in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) (American Psychiatric Association, 2013). Symptoms of this disorder can be broadly categorized into two main types:
Depersonalization symptoms include the following:
- One may feel detached from one's thoughts or body
- Sense of being an outside observer of one's thoughts, feelings, or actions
- Feeling emotionally or physically numb
- Distorted sense of time
- One may feel disconnected, like one's body or parts of it are unreal or don't belong to oneself
On the other hand, derealization symptoms are as follows:
- Feeling as if the world around is unreal, dreamlike, or foggy
- Perception of objects as changed in size, shape, or color
- Feeling emotionally disconnected from familiar people
- A sense that the environment is artificial or lacking in spontaneity
These symptoms can vary in intensity, may fluctuate over time, and can also co-occur with other mental health conditions.
How does this disorder develop?
The exact causes of depersonalization and derealization, along with other dissociative disorders, are not fully understood, but several factors are thought to contribute to its development:
- Trauma: Severe or significant distress or traumatic experiences, particularly in childhood, can trigger dissociative symptoms as a coping mechanism. Symptoms of this disorder can also be present in post-traumatic stress disorder.
- Neurobiological factors: Research suggests that alterations in brain areas involved in sensory integration and emotional processing may play a role in DPDR.
- Anxiety and depression: These conditions often co-occur with DPDR and may exacerbate symptoms.
- Substance use: Certain drugs, particularly cannabis, can induce depersonalization or derealization experiences in some individuals.
- Personality traits: Some studies have found associations between DPDR and traits such as emotional vulnerability and tendency towards introspection.
Understanding these potential contributing factors can help in developing targeted treatment approaches and providing comprehensive care for individuals with these mental health conditions.
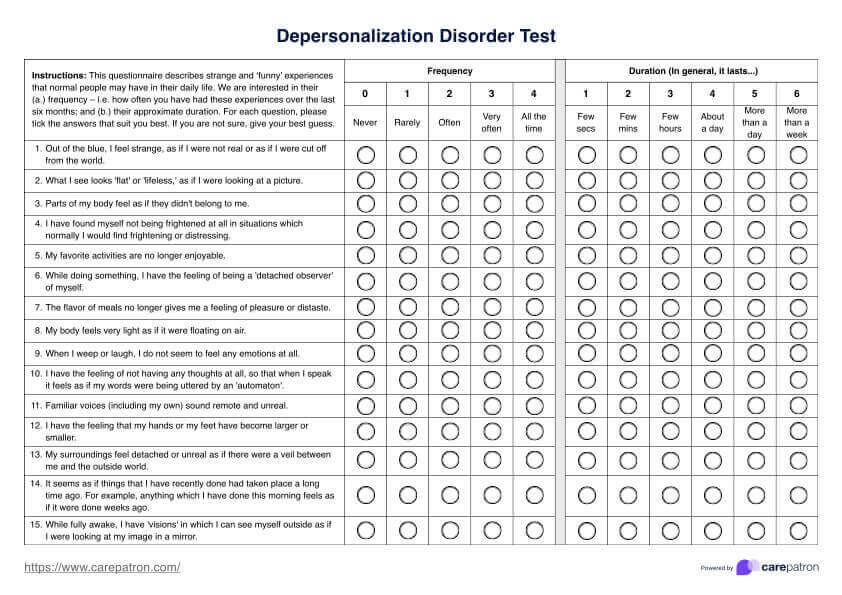
Depersonalization Disorder Test Template
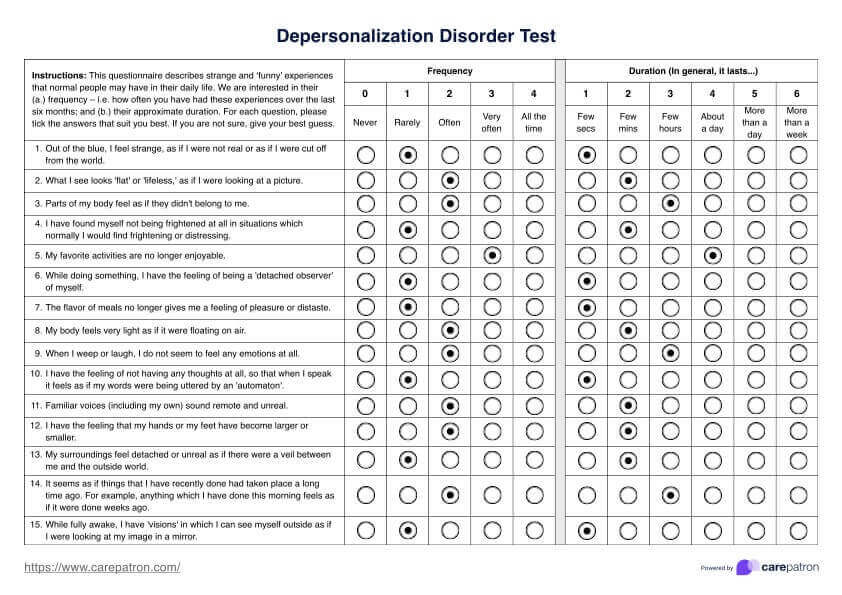
Depersonalization Disorder Test Example
What is a Depersonalization Disorder Test?
A Depersonalization Disorder Test is a structured assessment tool designed to evaluate the presence and severity of depersonalization and derealization symptoms.
In this context, we'll focus on the Cambridge Depersonalization Scale (CDS), one of the most widely used and validated instruments for assessing depersonalization symptoms (Sierra & Berrios, 2000). The CDS is a self-report questionnaire consisting of 29 items. Each item describes a specific depersonalization experience, such as feeling detached from one's body or perceiving the environment as unreal.
How is it scored and how are the results interpreted?
The scoring of the Cambridge Depersonalization Scale is designed to provide a comprehensive assessment of depersonalization symptoms. Each item is scored on frequency (0-4) and duration (1-6). The frequency and duration scores are multiplied for each item.
These items are then summed across all 29 to yield a total score ranging from 0 to 290.
A cut-off score of 70 is typically used to differentiate between individuals with clinically significant depersonalization symptoms and those without. Scores above 70 suggest the presence of depersonalization disorder, with higher scores indicating greater symptom severity.
How a mental health professional treats depersonalization
While there is no one-size-fits-all treatment for depersonalization, several evidence-based strategies have shown promise in managing symptoms and improving quality of life:
Psychotherapy
Psychotherapy forms the cornerstone of treatment for depersonalization. Cognitive behavioral therapy (CBT) is often the first-line approach, helping individuals identify and challenge distorted thoughts related to their depersonalization experiences. CBT and other forms of talk therapy can also provide coping strategies to manage anxiety and stress, which are often closely linked to depersonalization symptoms.
Medication
While no medications are specifically approved for treating depersonalization, pharmacotherapy may be used to address co-occurring conditions such as anxiety or depression.
Education
Education about depersonalization is a crucial component of treatment. Understanding that these experiences, while distressing, are not indicative of "going crazy" or permanent brain damage can significantly reduce anxiety and improve coping.
Grounding techniques
Grounding techniques are often taught in therapy to help individuals reconnect with their body and environment during episodes of depersonalization. These may include sensory exercises, such as focusing on physical sensations or engaging with the immediate surroundings.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Pearson.
Sierra, M., & Berrios, G. E. (2000). The Cambridge Depersonalization Scale: A new instrument for the measurement of depersonalization. Psychiatry Research, 93(2), 153–164. https://doi.org/10.1016/s0165-1781(00)00100-1
Commonly asked questions
The duration of depersonalization episodes can vary greatly. Depersonalization/derealization disorder is characterized by persistent or recurrent feelings of detachment, which may last for hours, days, weeks, months, or even years. The intensity of symptoms often fluctuates, with periods of more severe experiences alternating with milder ones. In some cases, the disorder can be chronic, with symptoms present continuously for decades.
No, depersonalization is not the same as psychosis. While both involve a sense of detachment from one's surroundings or self, the key difference is that individuals with depersonalization remain aware that their experiences are not reality. They know that feelings of unreality are just a subjective experience, not an objective reality.
There is no simple way to "snap out of" depersonalization, as it is a complex mental health condition that requires professional treatment and coping strategies. Individuals experiencing persistent or severe depersonalization/derealization should seek help from a mental health provider, as this is not something that can be easily resolved on one's own.


















-template.jpg)



















































































