What is conduct disorder?
Conduct Disorder is a psychiatric condition characterized by a repetitive and persistent pattern of aggressive behavior and serious violations of societal rules. It typically affects children and adolescents, impacting their social, academic, and occupational functioning. The diagnostic criteria, as outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM), involve behaviors such as physical fights, cruelty to animals, property destruction, and a disregard for rules and authority.
Children with Conduct Disorder may display various symptoms, including sudden aggressive outbursts, defiance, and a propensity for physical aggression. This disruptive behavior often leads to a diagnosis, and if left untreated, Conduct Disorder can have long-term consequences, increasing the risk of developing antisocial personality disorder and other psychiatric disorders.
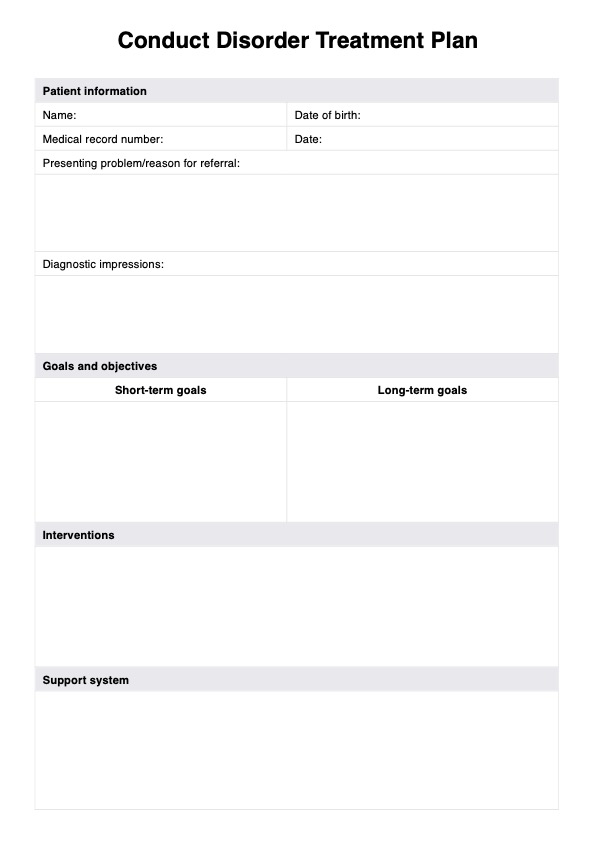
Early diagnosis and intervention are crucial. Mental health professionals may employ a comprehensive conduct disorder treatment plan, incorporating therapeutic approaches such as cognitive-behavioral therapy, family therapy, and parent management training. Addressing comorbid conditions like attention deficit hyperactivity disorder (ADHD) and mood disorders is essential for a holistic approach. Prevention and early intervention strategies, including parental monitoring and preventive research initiatives, play a vital role in reducing the risk factors associated with Conduct Disorder and promoting better mental health outcomes for affected individuals.