Conduct Disorder Assessment
Learn about conduct disorder assessment criteria and get Carepatron's free PDF download example for a comprehensive understanding of this mental health disorder.


What is conduct disorder?
Conduct disorder (CD) is a prevalent mental health condition typically diagnosed in childhood or adolescence, characterized by a persistent pattern of behavior that violates societal norms, rules, and the rights of others. Individuals with conduct disorder often exhibit a wide range of disruptive and aggressive behavior, which can include aggression towards people and animals, destruction of property, deceitfulness, and serious violation of rules.
This disorder is significant not only due to its disruptive impact on individuals' lives but also because it can lead to severe consequences if left untreated. Research suggests that conduct disorder is often a precursor to more severe aggressive behavior in adulthood, including antisocial personality disorder. Understanding and addressing conduct disorder early on is crucial for preventing the development of more severe mental disorders and reducing the likelihood of long-term adverse outcomes.
Antisocial behavior is a hallmark feature of conduct disorder, but it's important to recognize that not all antisocial behavior indicates the presence of conduct disorder. Conduct disorder is a complex condition influenced by various factors, including genetic predisposition, environmental influences, and neurobiological factors.
Conduct disorder symptoms
Conduct disorder manifests through a range of behaviors that consistently violate social norms and the rights of others. Understanding these symptoms is key to recognizing and addressing the condition effectively. Below are some common symptoms associated with conduct disorder:
- Persistent aggression towards people and animals
- Bullying, intimidation, or threatening behavior towards peers
- Frequent physical fights or altercations
- Deliberate destruction of property
- Deceitfulness, such as lying or stealing
- Serious violations of rules, including running away from home or skipping school
- Lack of empathy or remorse for the harm caused to others
- Persistent disregard for authority figures and rules
- Engagement in behaviors that are harmful to self or others
Conduct disorder causes
Understanding the underlying factors contributing to the development of conduct disorder is essential for effective prevention and intervention. While the exact causes of conduct disorder are complex and multifaceted, several factors have been identified through research and clinical observation. Here's an overview of some common causes associated with conduct disorder:
- Biological factors: Genetic predisposition is one such factor, where individuals with a family history of conduct disorders or other mental health conditions are more likely to develop conduct disorder themselves. Additionally, neurobiological abnormalities, such as variances in brain structure and function—particularly in areas related to impulse control and emotional regulation—can contribute to the manifestation of conduct disorder.
- Environmental factors: Adverse childhood experiences, including trauma, neglect, abuse, or chaotic family environments during early childhood, can significantly increase the risk of conduct disorder. Furthermore, parenting style is another environmental factor where inconsistent discipline, lack of supervision, and harsh or punitive parenting practices may contribute to the development of conduct disorder. Peer influences, such as association with delinquent peers or involvement in deviant peer groups, can reinforce antisocial behavior, further exacerbating conduct disorder. Additionally, socioeconomic factors like poverty, limited resources, and exposure to community violence can create stressors that increase vulnerability to conduct disorder.
- Psychological factors: Cognitive deficits, such as challenges in problem-solving, impulse control, and perspective-taking, may contribute to the manifestation of conduct disorder. Emotional dysregulation, characterized by difficulties in managing and expressing emotions appropriately, can lead to impulsive and aggressive behaviors associated with conduct disorder. Additionally, certain personality traits—such as low empathy, sensation-seeking, and a propensity for risk-taking—may increase susceptibility to conduct disorder.
Is conduct disorder dangerous?
Understanding the potential dangers of conduct disorder is crucial for individuals, families, and communities. While conduct disorder is not inherently dangerous, the behaviors and patterns characteristic of the disorder can pose significant risks to the individual affected and those around them. Here's a closer look at the potential dangers associated with conduct disorder:
- Risk of harm to self and others: This can include physical fights, assaults, and acts of vandalism or destruction of property.
- Impact on academic and social functioning: Persistent behavioral problems may result in academic failure, expulsion, or involvement with the juvenile justice system, limiting the individual's opportunities for future success and stability.
- Association with other mental health concerns: The presence of multiple disorders can complicate treatment and increase the risk of adverse outcomes, including substance abuse, criminal behavior, and self-harm.
- Long-term impact on development: Left untreated, conduct disorder can affect an individual's growth and well-being.
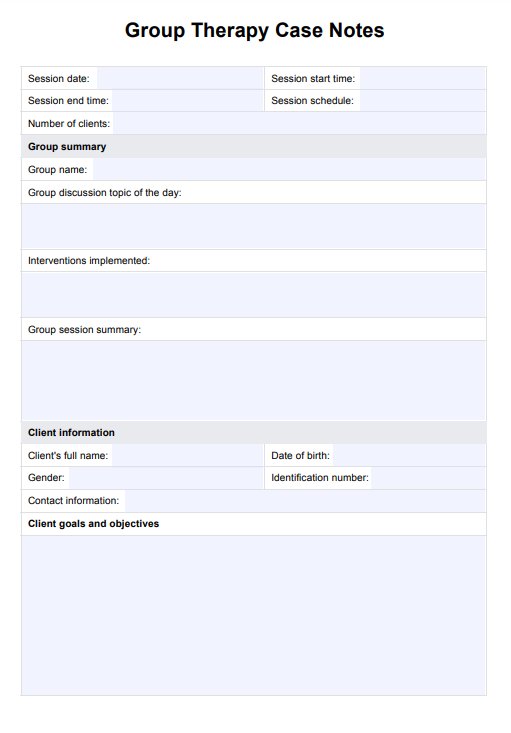
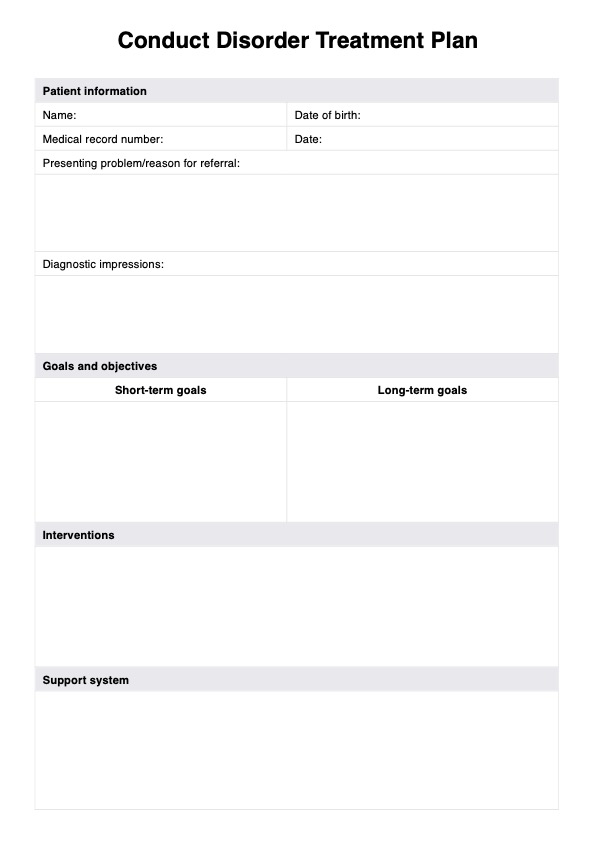
Conduct Disorder Assessment Template
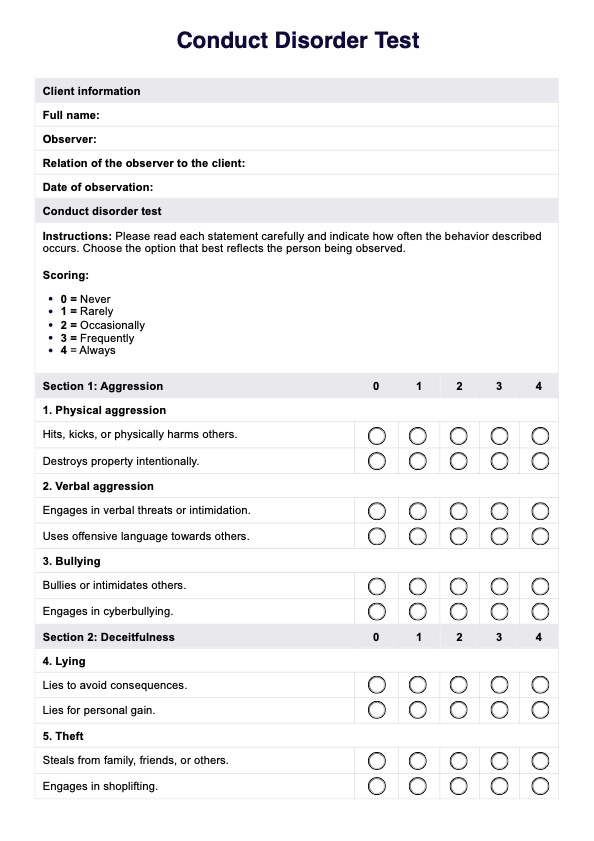
Conduct Disorder Assessment Example
What is a Conduct Disorder Assessment?
A conduct disorder assessment is a comprehensive evaluation conducted by mental health professionals to assess the presence and severity of conduct disorder in children and adolescents. s. Conduct disorder assessments aim to identify these behavioral patterns, understand their underlying causes, and determine appropriate interventions to address them.
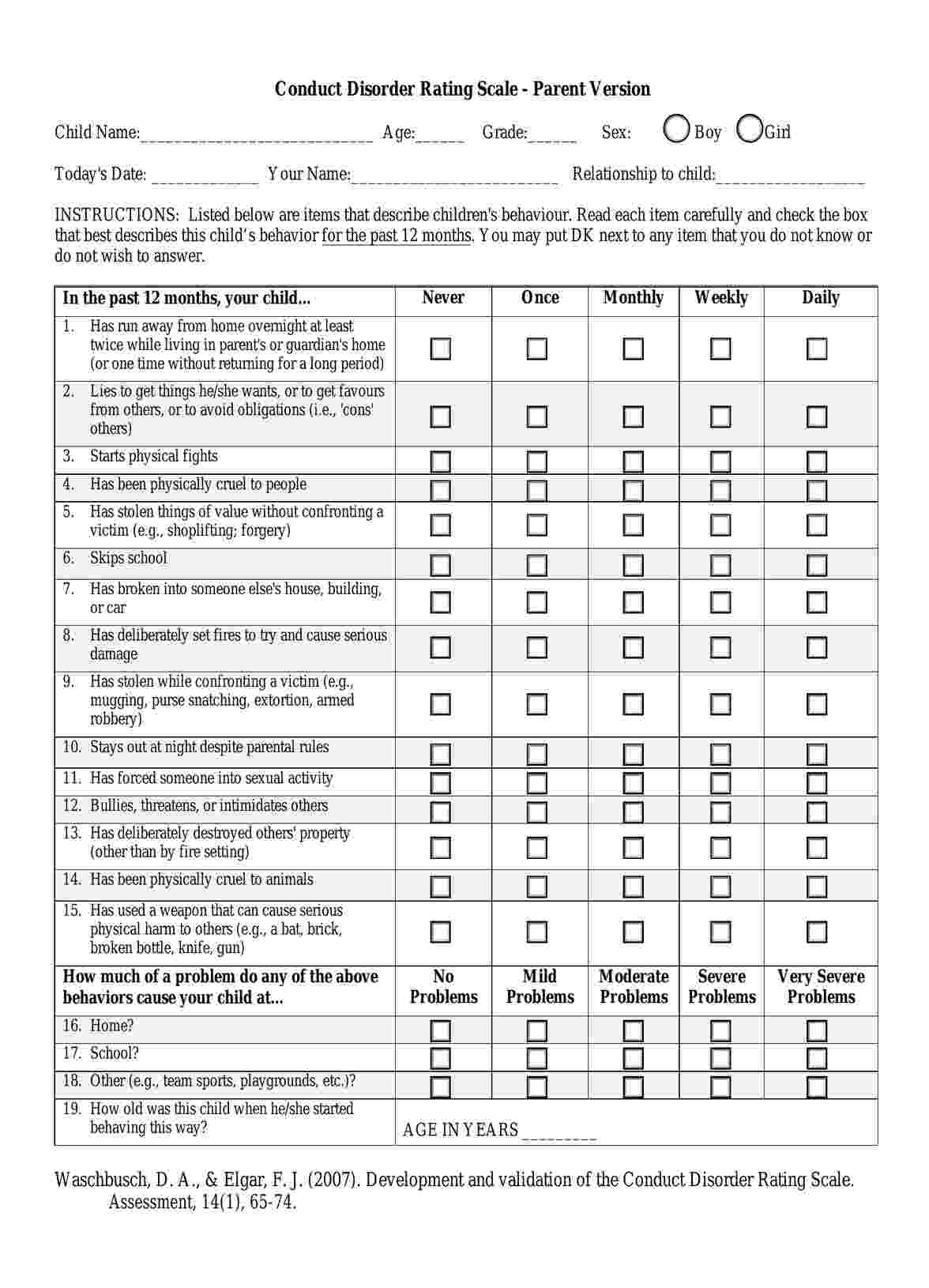
The Conduct Disorder Rating Scale (CDRS) developed by Waschbusch and Elgar in 2007 is a tool commonly used to assess conduct disorder in children and adolescents. Conduct disorder is a psychiatric condition characterized by a persistent pattern of behavior that violates the rights of others or societal norms. These behaviors may include aggression, destruction of property, deceitfulness, and rule-breaking.
The CDRS is available in different parent, teacher, and self-report versions. The parent version is designed to be completed by parents or caregivers who have regular contact with the child. It typically consists of a series of questions or statements related to the child's behavior, and respondents are asked to rate the frequency and severity of these behaviors over a specified period, such as the past six months.
The CDRS assesses various domains of conduct disorder, including aggression, deceitfulness, rule-breaking behavior, and peer relationships. It provides a comprehensive evaluation of the child's conduct-related difficulties, which can help clinicians make an accurate diagnosis and develop appropriate treatment plans.
The use of standardized rating scales like the CDRS can be valuable in clinical practice for several reasons:
- Objective assessment: The CDRS provides a structured format for evaluating conduct disorder symptoms, reducing the potential for bias in evaluation.
- Consistency: By using a standardized tool, clinicians can ensure consistency in assessment across different patients and settings.
- Treatment planning: The information obtained from the CDRS can help clinicians identify specific areas of difficulty and tailor interventions to address them effectively.
- Monitoring progress: The CDRS can be used to monitor changes in behavior over time, allowing clinicians to track the effectiveness of interventions and make adjustments as needed.
Overall, the Conduct Disorder Rating Scale (Parent Version) is a valuable tool for assessing conduct disorder in children and adolescents, providing clinicians with vital information to guide diagnosis and treatment.
Next steps
After completing a conduct disorder assessment, individuals and their families need to take proactive steps to address the findings and seek appropriate support and intervention. Here are some recommended next steps:
- Seek professional guidance: Consult with a qualified mental health professional, such as a psychologist, psychiatrist, or licensed therapist, to discuss the assessment results and develop a comprehensive treatment plan. These professionals can provide expert guidance and support tailored to the individual's needs and circumstances.
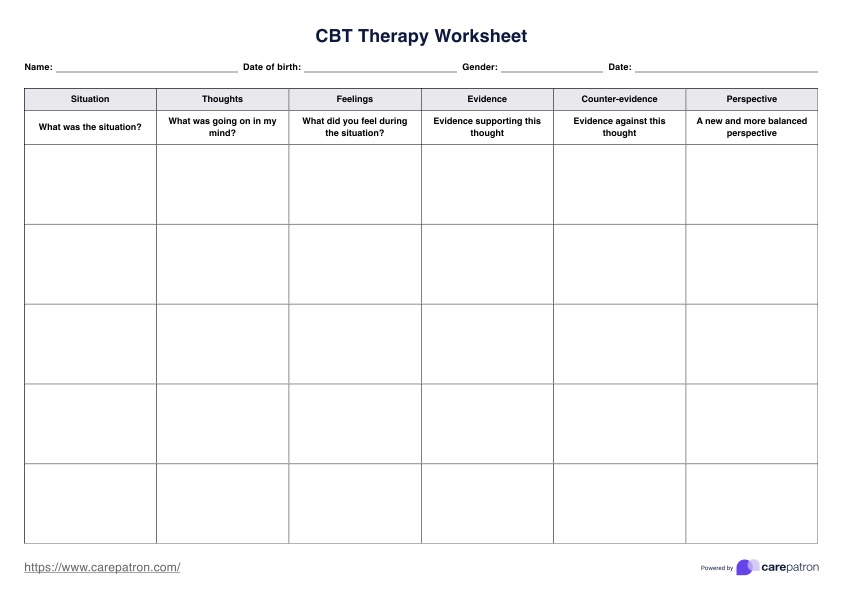
- Explore treatment options: Explore available treatment options for conduct disorder, including individual therapy, family therapy, parent management training, and medication management. Evidence-based interventions, such as cognitive-behavioral therapy (CBT) and dialectical behavior therapy (DBT), can effectively address conduct disorder symptoms and promote positive behavior change.
- Address comorbid conditions: If the assessment identifies comorbid conditions such as attention deficit hyperactivity disorder (ADHD) or oppositional defiant disorder (ODD), it's essential to address these conditions as part of the treatment plan. Addressing comorbid conditions can improve overall outcomes and reduce the risk of complications such as antisocial personality disorder.
- Educate yourself: Take the time to educate yourself and your family about conduct disorder and related mental health disorders. Understanding the symptoms, causes, and treatment options can empower individuals and families to actively participate in the treatment process and advocate for their needs.
- Implement supportive strategies: Implement supportive strategies and interventions at home, school, and in the community to promote positive behavior and enhance coping skills. This may include setting clear and consistent boundaries, providing positive reinforcement for desirable behavior, and fostering open communication within the family.
- Monitor progress: Regularly monitor progress and reassess the effectiveness of interventions over time. Keep track of changes in behavior, mood, and functioning, and communicate any concerns or challenges to the mental health professional overseeing the treatment.
- Stay engaged in treatment: Stay engaged and committed to the treatment process, attending scheduled therapy sessions, participating in recommended activities, and following through with prescribed interventions. Consistent effort and participation are essential for achieving positive outcomes and managing conduct disorder effectively.
How does our Conduct Disorder Assessment template work?
Carepatron's Conduct Disorder Assessment template provides a structured framework for evaluating conduct disorder symptoms and their severity. Built upon Waschbusch and Elgar (2007)'s Conduct Disorder Rating Scale (parent version), our template offers a user-friendly approach to conducting comprehensive assessments.
The assessment comprises a series of items that describe children's behavior over the past 12 months. Caregivers or professionals administering the assessment are instructed to read each item carefully and click the button that best describes the child's behavior frequency, ranging from "Never" to "Daily."
The assessment includes items covering a wide range of behaviors associated with conduct disorder, including running away from home, lying, physical aggression, theft, vandalism, and more. By systematically evaluating each behavior, caregivers and professionals can gain insight into the child's symptomatology and assess the severity of conduct disorder symptoms.
This assessment allows for a comprehensive assessment of the impact of conduct disorder on various areas of the child's life, including academic performance, social interactions, and family dynamics.
When do healthcare professionals conduct this assessment?
Healthcare professionals conduct assessments for conduct disorder in various situations to identify and address behavioral concerns in children and adolescents. Here are some instances when these assessments may be performed:
1. Routine mental health screening
Healthcare professionals may administer conduct disorder assessments as part of routine mental health screenings for children and adolescents. These screenings help identify early signs of conduct disorder and other disruptive behavior disorders, enabling timely intervention and support.
2. Diagnostic evaluation
When healthcare professionals suspect conduct disorder based on symptoms such as aggression, deceitfulness, and rule violations, they may conduct a formal diagnostic evaluation. This evaluation involves assessing the child's behavior, gathering information from multiple sources, and using standardized assessment tools to determine whether the criteria for conduct disorder are met.
3. Treatment planning
Conduct disorder assessments play a crucial role in treatment planning for affected individuals. Healthcare professionals use assessment results to tailor interventions to the child's specific needs and circumstances. This may include implementing evidence-based treatments such as parent management training, cognitive-behavioral therapy, and family therapy.
4. Monitoring treatment progress
Healthcare professionals may conduct follow-up assessments to monitor the child's progress in treatment and evaluate the effectiveness of interventions. Regular assessments allow for adjustments to treatment plans as needed and ensure that the child receives appropriate support in managing conduct disorder symptoms.
5. Differential diagnosis
Conduct disorder assessments help healthcare professionals differentiate between conduct disorder and other conditions that may present with similar symptoms, such as oppositional defiant disorder (ODD) or attention deficit hyperactivity disorder (ADHD). Accurate diagnosis is essential for developing targeted treatment strategies and optimizing outcomes for affected individuals.
Benefits of this assessment
Conduct disorder assessments offer several benefits in identifying and addressing behavioral concerns in children and adolescents. Here are some key benefits:
1. Early identification and intervention
Early identification of conduct disorder through assessments allows for timely intervention and support. By recognizing symptoms early on, healthcare professionals can implement targeted interventions to address behavioral concerns before they escalate. Early intervention has been shown to improve outcomes and reduce the risk of long-term complications.
2. Accurate diagnosis
Conduct disorder assessments follow the Diagnostic and Statistical Manual of Mental Disorders (DSM) criteria, ensuring accurate diagnosis. Proper diagnosis is essential for distinguishing conduct disorder from other conditions that may present with similar symptoms, such as oppositional defiant disorder (ODD) or bipolar disorder. Accurate diagnosis guides treatment planning and intervention strategies tailored to the child's specific needs.
3. Tailored treatment planning
Assessment results inform treatment planning by identifying the severity and nature of conduct disorder symptoms. Healthcare professionals can use this information to develop personalized treatment plans that address the child's unique challenges and strengths. Tailored interventions may include cognitive-behavioral therapy, parent management training, and family therapy.
4. Prevention of long-term complications
Early intervention and targeted treatment can help prevent the escalation of conduct disorder symptoms and reduce the risk of long-term complications. Untreated conduct disorder may increase the likelihood of developing other mental health conditions, such as substance use disorders or personality disorders, later in life. Addressing conduct disorder early can mitigate these risks and promote positive outcomes.
5. Improved functioning and well-being:
Effective assessment and intervention can improve the child's functioning and overall well-being. Individuals can better manage their behavior and navigate social interactions by addressing conduct disorder symptoms and teaching coping skills. Improved functioning enhances the child's quality of life and promotes positive relationships with family, peers, and community members.
Reference
Waschbusch, D. A., & Elgar, F. J. (2007). Conduct Disorder Rating Scale - Parent Version. Retrieved March 27, 2024, from https://img1.wsimg.com/blobby/go/73dc20c0-1bdd-4f61-9d40-97e669c52c8b/downloads/cdrs_parentv%20Conduct%20disorder%20questionaire.pdf?ver=1650956965417
Commonly asked questions
Assessment for conduct disorders typically involves conducting interviews, using standardized assessment tools, and gathering information from multiple sources, such as parents, teachers, and the child themselves.
Common symptoms of conduct disorder include aggression towards people or animals, destruction of property, deceitfulness or theft, and serious violations of rules.
The best assessment for conduct disorder often involves using validated tools such as the Diagnostic Interview Schedule for Children (DISC) or the Child Behavior Checklist (CBCL) to evaluate behavior patterns and severity.




















-template.jpg)