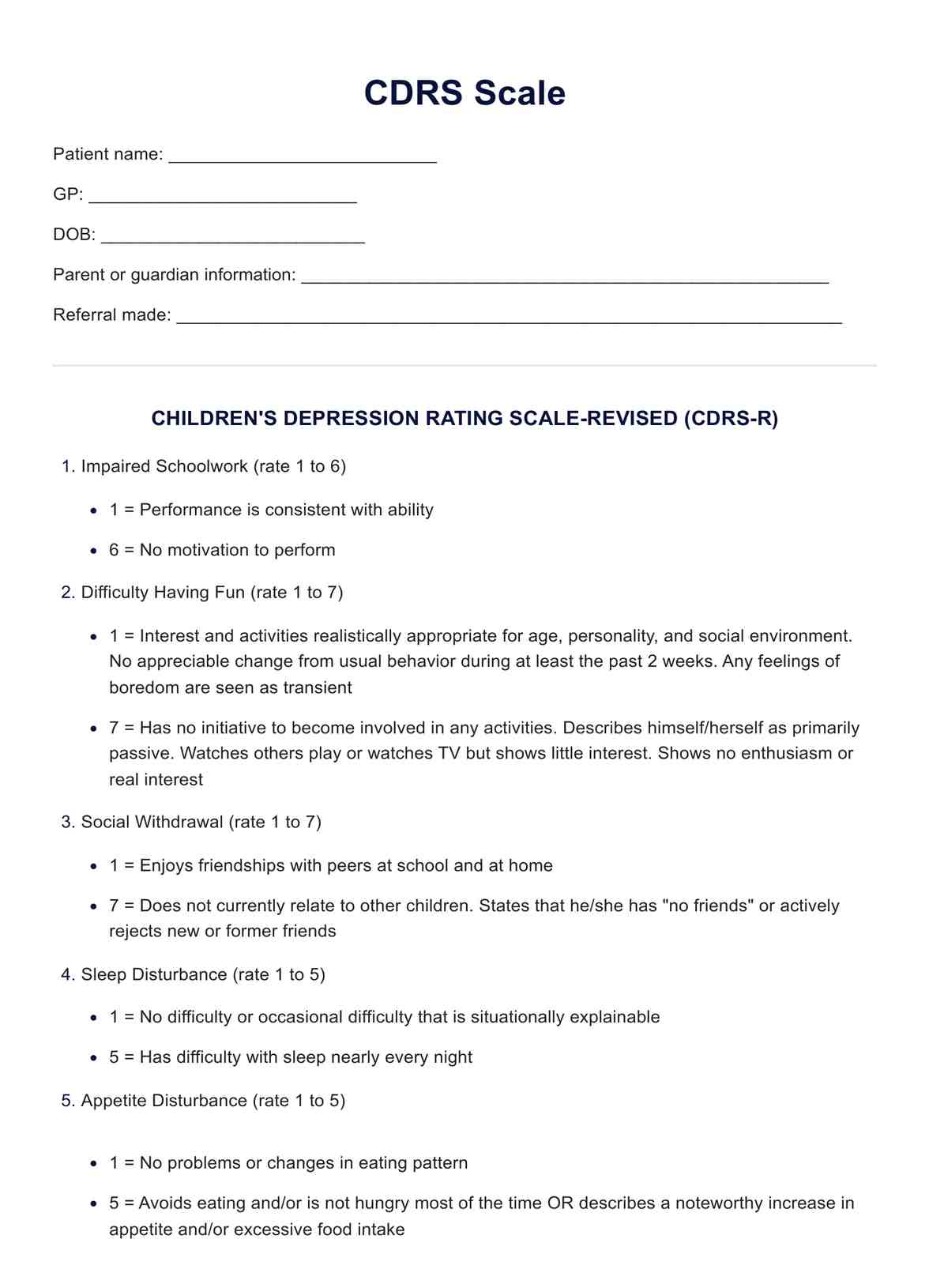
CDRS Scale
Comprehensive guide to interpreting Children's Depression Rating Scale (CDRS) scores, aiding in understanding and addressing childhood depression effectively.


What is the Children's depression rating (CDRS) scale?
The Children's Depression Rating Scale (CDRS) is a widely used clinical assessment tool designed to evaluate the severity of depressive symptoms in children and adolescents aged 6 to 12 years. Developed by Poznanski and Mokros in 1996, the scale aims to provide a systematic and structured approach for clinicians to assess the various facets of depression in this specific age group.
The CDRS comprises 17 items that comprehensively cover emotional, behavioral, and physiological domains associated with depression. The assessment encompasses observable behaviors, self-reports, and clinician evaluations, offering a multi-dimensional perspective on the child's mental health. Clinicians or trained assessors administer the scale through a structured interview, considering the child's responses, self-report, and observable behaviors during the assessment session.
The scale evaluates a range of depressive symptoms, including mood disturbances, sleep difficulties, appetite changes, and feelings of guilt or worthlessness. It also considers observable signs such as facial expressions, posture, and psychomotor agitation or retardation. The child's ability to concentrate, engage in activities, and interact with others is assessed to gauge the impact of depression on daily functioning.
Each item on the CDRS is scored based on the frequency and severity of the observed symptoms, with higher scores indicating more severe depressive symptoms. The cumulative score provides an overall measure of the child's depression severity, helping clinicians make informed decisions about diagnosis, treatment planning, and monitoring the progress of depressed children over time.
One notable aspect of the CDRS is its sensitivity to changes in symptomatology, allowing clinicians to track fluctuations in depressive symptoms during treatment. This makes it a valuable tool for initial assessments and ongoing monitoring in clinical settings.
While the CDRS is a valuable instrument for assessing depression in children, clinicians need to consider the broader context of the child's life, including family dynamics, school environment, and social factors, to gain a comprehensive understanding of the child's mental health. Additionally, the scale is typically used with other assessment tools and clinical interviews to ensure a thorough and accurate evaluation of the child's psychological well-being.
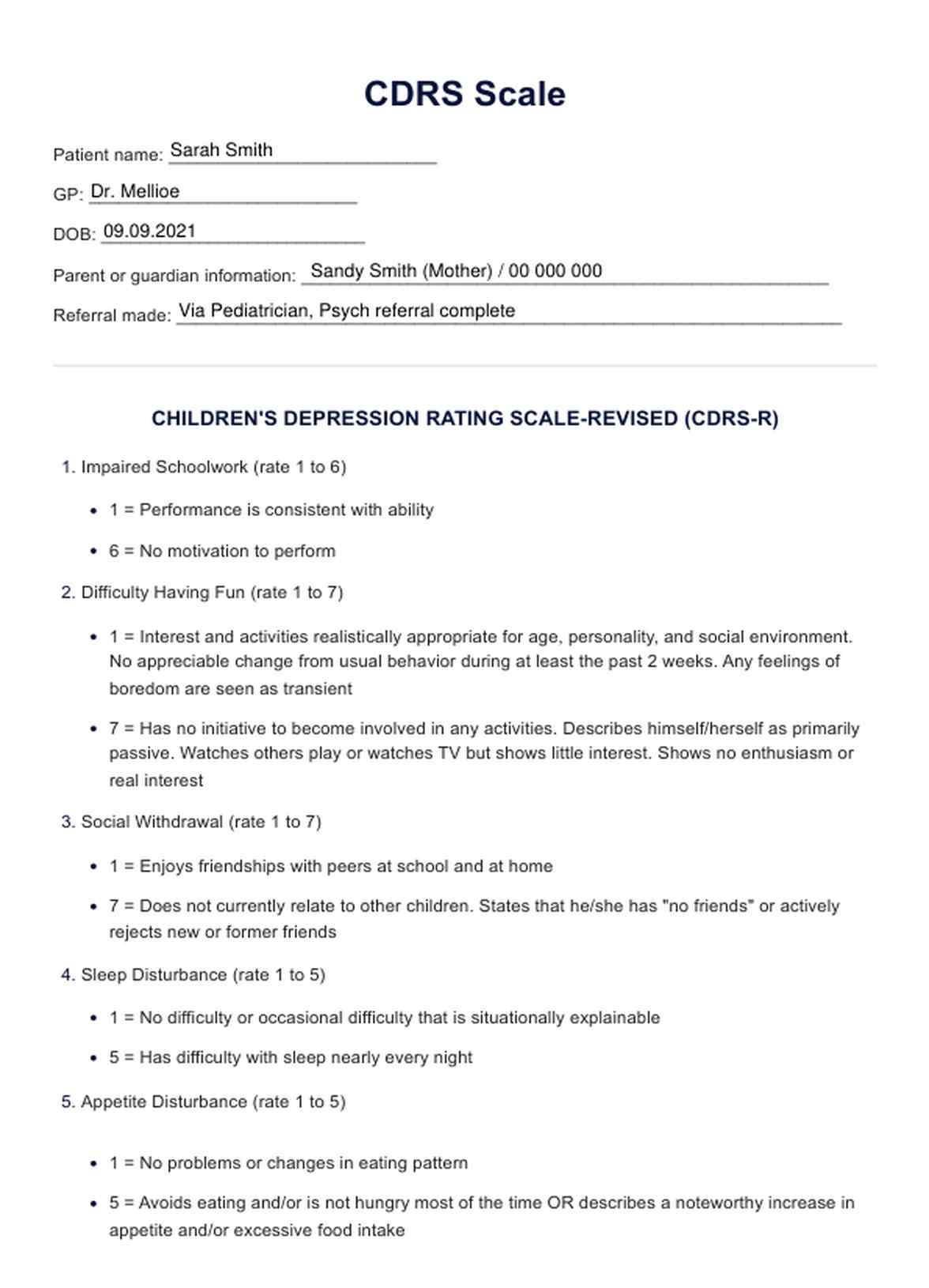
CDRS Scale Template
CDRS Scale Example
Who is this assessment for?
The Children's Depression Rating Scale (CDRS) is a depression scale designed for children and adolescents between the ages of 6 and 12. This specific age range is the target population for whom the scale was developed, and it is tailored to assess and measure the severity of depressive symptoms in this age group.
The CDRS is not intended for use with individuals outside the specified age range. For adolescents older than 12 years, there are other assessment tools and scales designed to evaluate depressive symptoms that may be more appropriate. Likewise, alternative measures specifically crafted for younger children below the age of 6 are typically utilized for their developmental stage.
The Children's Depression Rating Scale (CDRS) is typically utilized by mental health professionals, clinicians, and researchers with the appropriate training and qualifications. The individuals who are qualified to administer and interpret the CDRS include:
Clinical psychologists
Psychologists with expertise in child and adolescent psychology often use the CDRS as part of their diagnostic and assessment tools to evaluate depressive symptoms in children aged 6 to 12.
Child psychiatrists
Psychiatrists specializing in child and adolescent psychiatry may use the CDRS in their clinical practice to aid in the diagnosis and treatment planning for children experiencing depressive symptoms.
Licensed clinical social workers (LCSWs)
Mental health professionals, such as LCSWs, who work with children and adolescents may incorporate the CDRS into their assessments to better understand and address depressive symptoms.
Pediatricians and child health professionals
In some cases, pediatricians or other healthcare providers with expertise in child and adolescent mental health may use the CDRS as part of a broader evaluation when there are concerns about a child's mental well-being.
Clinical researchers
Researchers studying child and adolescent mental health may use the CDRS as a standardized tool to measure depressive symptoms in their research studies.
Individuals utilizing the CDRS must have a solid understanding of child development, psychopathology, and assessment techniques. The scale should be administered by trained professionals to ensure accurate and reliable results. Additionally, CDRS scores should be interpreted within the context of a comprehensive clinical assessment, considering other relevant information about the child's life, family, and social environment.
Parents and caregivers may not typically administer the CDRS themselves; instead, they would work with qualified mental health professionals who use this tool as part of a broader evaluation process.
How does the CDRS Scale work?
Step One: Gather your resources
CDRS Scales are a valuable resource and essential to keep on hand. Make sure that you have a copy of the free printable PDF when the need arises by either clicking the “Download Template” or “Use Template” button or by searching “CDRS Scale” on Carepatron’s template library’s search bar on the website or app.
Step Two: Collate essential information
Once the patient has been diagnosed and assessed for depression, utilizing the CDRS Scale Template to ensure all goals of care are met is seamless and easily accessible to relevant parties via Carepatron's centralized workspace. Assessment, symptom management, and interventions can be collated within the single care plan and safely stored on a single database. The care plan allows for individualized treatment options. It acts as a scaffolding to ensure goals of care are met, and the next steps are recorded for future reference or distribution to other healthcare specialists who are part of the patient's care team. You can use this care plan template to refine your practice and improve client success.
Step Three: Store the chart securely
After reviewing the CDRS Scale and creating a viable and individualized plan for the patient, you need to secure the plan so that access is only granted to relevant parties.
Ensure this through Carepatrons HIPAA-compliant free patient records software. Here, all relevant medical records can be safely stored and collated for ease and security.
Scoring and results
The Children's Depression Rating Scale (CDRS) is designed to assess and quantify the severity of depressive symptoms in children aged 6 to 12. The scores obtained from the CDRS indicate the level of depressive symptomatology exhibited by the child during the assessment. Here is a general overview of how the children's depression inventory scores and results are interpreted:
Scoring system
The CDRS consists of 17 items, each rated on a scale from 1 to 7. The total score is derived by summing the scores for all items, with higher scores indicating more severe depressive symptoms.
Interpretation of total score
- Mild depression (Total Score 20-40): Scores in this range suggest the presence of mild depressive symptoms.
- Moderate depression (Total Score 41-60): Scores in this range indicate a moderate level of depressive symptoms.
- Severe Depression (Total Score 61 and above): Scores in this range suggest a high level of severity of depressive symptoms.
Individual item scores
In addition to the total score, clinicians may examine individual item scores to identify specific areas of concern. This detailed analysis can help in the treatment response and understanding of the nature and nuances of the child's depressive symptoms.
Monitoring changes
The CDRS is often used longitudinally to monitor changes in depressive symptoms over time, such as during the treatment period. A decrease in the total score may indicate improvement, while an increase in the t score may suggest worsening symptoms.
Clinical judgment
It's important to note that while the CDRS provides a quantitative measure of depressive symptoms, clinical judgment plays a crucial role in interpreting the scores. The context of the child's life, family dynamics, and overall functioning should be considered to ensure a comprehensive understanding.
Integration with other assessments
The CDRS is typically used as part of a broader clinical assessment. The psychological assessment results should be interpreted in conjunction with information gathered from interviews, observations, and other relevant assessments to comprehensively evaluate the child's mental health.
It's essential for professionals using the CDRS to be trained in its administration and interpretation to ensure accurate and meaningful results. Additionally, the CDRS is just one component of a comprehensive assessment process, and its findings should be considered within the broader context of the child's well-being.
Next steps for treating childhood depression
Treating childhood depression often involves a comprehensive and individualized approach that may include a combination of therapeutic, supportive, and, in some cases, pharmacological interventions. Here are some next steps for treating childhood and adolescent depression well:
Therapeutic interventions
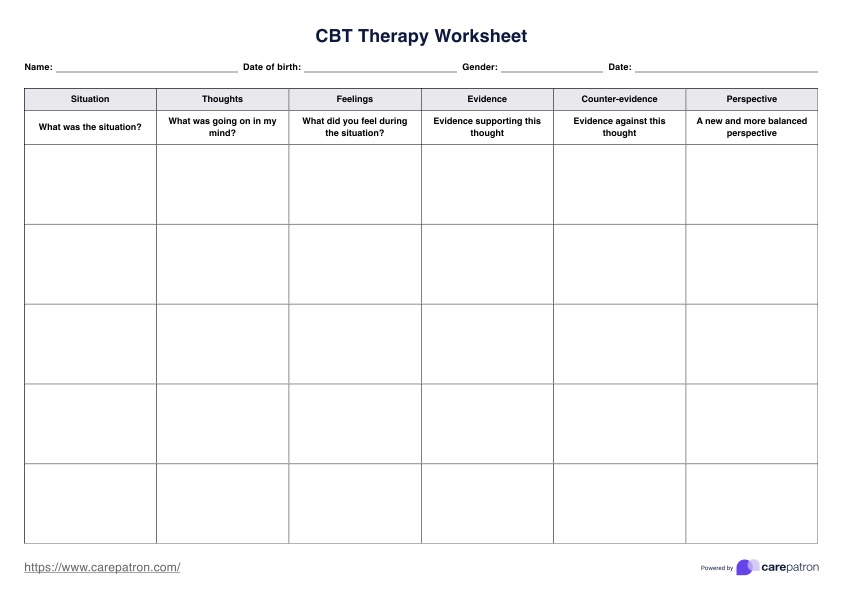
- Cognitive-behavioral therapy (CBT): CBT is an evidence-based therapeutic approach that helps children identify and change negative thought patterns and behaviors associated with depression.
- Play therapy: Especially effective for younger children, play therapy allows children to express and explore their emotions through play, aiding in the therapeutic process.
- Family therapy: Involving the family in therapy can help improve communication, address family dynamics, and support the child and their caregivers.
Supportive Environment
- Create a supportive home environment: Foster a supportive and understanding atmosphere at home. Encourage open communication and provide reassurance and validation for the child's feelings.
- School involvement: Collaborate with the child's school to create a supportive environment. This may involve communicating with teachers, school counselors, or administrators to ensure the child's academic and emotional needs are met.
Healthy lifestyle
- Promote physical activity: Regular physical activity can positively affect mood. Encourage the child to engage in age-appropriate physical activities.
- Healthy nutrition: Ensure the child has a balanced diet with adequate nutrition. Nutrient-rich foods can positively impact mood and overall well-being.
Medication (if necessary)
- Consultation with a psychiatrist: If the depression is severe or not responsive to therapy alone, a child psychiatrist may evaluate the need for medication. Medication is generally considered after careful assessment and when the potential benefits outweigh the potential risks.
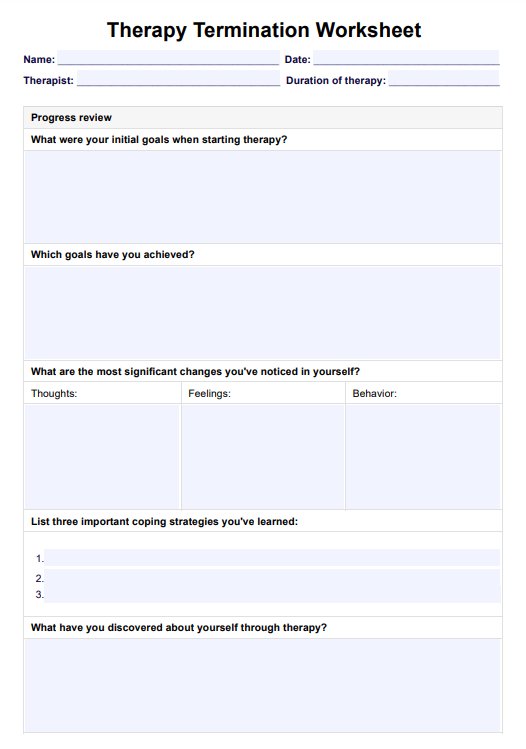
Monitoring and adjusting the treatment plan
- Regular check-ins: Schedule regular follow-up appointments with the mental health professional to monitor progress and make any necessary adjustments to the treatment plan.
- Involve caregivers: Keep caregivers informed and involved in the treatment process. Educate them about childhood depression and involve them in therapeutic activities or interventions.
Crisis intervention
- Emergency plan: Develop a crisis intervention plan in case of acute worsening of symptoms. This may involve knowing emergency contact numbers, having a safety plan, and being aware of local crisis resources.
Remember that childhood depression is a complex condition, and treatment plans should be tailored to the individual child's needs. It's essential to involve a collaborative team, including mental health professionals, caregivers, and educators, to support the child's emotional well-being. Regular communication among all involved parties contributes to a holistic and effective treatment approach.
.png)
Other useful resources
Carepatron has made a suite of effective guides and templates related to clinical and psychology needs, have a look at some of the handy related links below to assist you and your practice!
https://www.carepatron.com/templates/child-and-adolescent-trauma-screen-cats-caregiver-report-ages-7-17-years
https://www.carepatron.com/templates/spence-childrens-anxiety-scale-child-report
Research and evidence
Approximately 15% of individuals aged 10-19 worldwide grapple with a mental health disorder, contributing to 13% of the overall burden of disease within this demographic (World Health Organization, 2021). In the United States, in 2016, nearly 20% of children aged 2-8 years received a diagnosis of a mental, behavioral, or developmental disorder (Cree et al., 2018). The prevalence of mental health challenges persists among adolescents aged 12-17, with about 15% experiencing a major depressive episode in 2018-2019. Additionally, 37% reported enduring feelings of persistent sadness or hopelessness, while almost 20% acknowledged seriously contemplating suicide (Bitsko et al., 2022).
A study conducted by the Health Resources and Services Administration (HRSA) revealed a concerning trend between 2016 and 2020, indicating a 27% increase in the number of children aged 3-17 diagnosed with depression (Lebrun-Harris et al., 2022).
Notably, boys aged 2-8 were more likely than girls to have a mental, behavioral, or developmental disorder. However, adolescent girls aged 12-17 exhibited a significant and sustained surge in depression cases since 2009 (Cree et al., 2018). Additionally, more than one-fifth (22%) of children living below the poverty threshold of 100% reported having a mental, behavioral, or developmental disorder (Cree et al., 2018). The likelihood of children receiving treatment for anxiety, depression, or behavior problems was influenced by age and poverty level (Ghandour et al., 2019).
The Children's Depression Rating Scale-Revised (CDRS-R) is currently one of the most frequently employed tools for evaluating depressive symptoms in minors within the context of clinical trials. Originally designed for individuals aged 6 to 12, it is also commonly used in adolescents (Mayes et al., 2010).
Administered by clinicians through a 17-item interview, each item is rated between 1 (indicating no difficulties) and 5 or 1 and 7 (indicating clinically significant difficulties), resulting in a total score ranging from 17 to 113. A score of ≥40 is generally considered indicative of depressive symptoms, while a score ≤28 is often interpreted as a remission in trials (Plener et al., 2012).
References
Bitsko, R. H., Claussen, A. H., Lichstein, J., Black, L. I., Jones, S. E., Danielson, M. L., Hoenig, J. M., Davis Jack, S. P., Brody, D. J., Gyawali, S., Maenner, M. J., Warner, M., Holland, K. M., Perou, R., Crosby, A. E., Blumberg, S. J., Avenevoli, S., Kaminski, J. W., Ghandour, R. M., & Meyer, L. N. (2022). Mental Health Surveillance Among Children — United States, 2013–2019. MMWR Supplements, 71(2), 1–42. https://doi.org/10.15585/mmwr.su7102a1
Cree, R. A., Bitsko, R. H., Robinson, L. R., Holbrook, J. R., Danielson, M. L., Smith, C., Kaminski, J. W., Kenney, M. K., & Peacock, G. (2018). Health Care, Family, and Community Factors Associated with Mental, Behavioral, and Developmental Disorders and Poverty Among Children Aged 2–8 Years — United States, 2016. MMWR. Morbidity and Mortality Weekly Report, 67(50), 1377–1383. https://doi.org/10.15585/mmwr.mm6750a1
Ghandour, R. M., Sherman, L. J., Vladutiu, C. J., Ali, M. M., Lynch, S. E., Bitsko, R. H., & Blumberg, S. J. (2019). Prevalence and Treatment of Depression, Anxiety, and Conduct Problems in US Children. The Journal of Pediatrics, 206, 256–267. https://doi.org/10.1016/j.jpeds.2018.09.021
Lebrun-Harris, L. A., Ghandour, R. M., Kogan, M. D., & Warren, M. D. (2022). Five-Year Trends in US Children’s Health and Well-being, 2016-2020. JAMA Pediatrics, 176(7). https://doi.org/10.1001/jamapediatrics.2022.0056
Mayes, T. L., Bernstein, I. H., Haley, C. L., Kennard, B. D., & Emslie, G. J. (2010). Psychometric Properties of the Children’s Depression Rating Scale–Revised in Adolescents. Journal of Child and Adolescent Psychopharmacology, 20(6), 513–516. https://doi.org/10.1089/cap.2010.0063
Plener, P. L., Grieb, J., Sproeber, N., Straub, J., Schneider, A., Keller, F., & Koelch, M. G. (2012). Convergence of children´s depression rating scale-revised scores and clinical diagnosis in rating adolescent depressive symptomatology. Mental Illness, 4(1), 7. https://doi.org/10.4081/mi.2012.e7
World Health Organization. (2021, November 17). Mental Health of Adolescents. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health
Commonly asked questions
Clinicians use the score to assess the severity of depressive symptoms, with higher scores generally indicating more significant symptomatology. The interpretation may involve categorizing the severity as mild, moderate, or severe, helping guide treatment decisions and interventions.
Clinicians use CDRS scores as a valuable tool to guide treatment decisions. For instance, a higher score may suggest the need for more intensive interventions, including therapy or, in some cases, medication. A decreasing score over time may indicate treatment effectiveness or remission, influencing decisions about the continuation or modification of treatment strategies.
While there isn't a fixed "normal" score, lower scores generally suggest fewer depressive symptoms. Clinicians compare individual scores to established norms for the child's age and demographic, considering factors like developmental stage. Understanding the typical range can provide reassurance or prompt further investigation if scores deviate significantly.


















-template.jpg)