Bulimia Nervosa DSM-5 Criteria
Learn about Bulimia Nervosa DSM-5 Criteria in our guide, symptoms, diagnosis, and treatment options. Use our template for easy reference.


What is bulimia nervosa?
Bulimia nervosa is one of the eating disorders defined in the Diagnostic and Statistical Manual of Mental Disorders. It is characterized by recurrent episodes of binge eating followed by inappropriate compensatory behaviors to prevent weight gain. These behaviors include self-induced vomiting, misuse of laxatives, diuretics, or other medications, fasting, or excessive exercise. Individuals with bulimia nervosa often feel a lack of control over their eating during binge episodes and place an excessive emphasis on body shape and weight in their self-evaluation.
There are two subtypes of bulimia nervosa: the purging type and the non-purging type. The purging type involves regular self-induced vomiting or the misuse of laxatives, diuretics, or enemas. The non-purging type involves other inappropriate compensatory behaviors, such as fasting or excessive exercise, but does not regularly engage in purging behaviors.
Bulimia nervosa differs from anorexia nervosa in that individuals with bulimia nervosa are typically within the normal weight or overweight range, whereas individuals with anorexia nervosa are underweight. Additionally, anorexia nervosa involves a restriction of food intake leading to significantly low body weight, while bulimia nervosa involves episodes of binge eating followed by compensatory behaviors.
Bulimia Nervosa DSM-5 Criteria Template
Bulimia Nervosa DSM-5 Criteria Template
How is bulimia nervosa diagnosed?
Diagnosing bulimia nervosa involves a comprehensive assessment by a healthcare professional, including several critical steps:
- Clinical interview: The healthcare provider conducts a detailed interview to understand the patient’s eating behaviors, attitudes towards food and body image, and any compensatory behaviors. The clinician inquires about the frequency and context of binge eating episodes and inappropriate compensatory behaviors.
- Medical history and physical examination: A thorough medical history helps identify physical complications associated with bulimia nervosa, such as electrolyte imbalances, gastrointestinal issues, and dental problems. The physical examination looks for signs like dental erosion, calluses on the hands from inducing vomiting, and swelling of the parotid glands.
- Laboratory tests: Various laboratory tests identify physiological abnormalities resulting from purging behaviors. These tests may include checking electrolyte levels, renal function, and liver enzymes. Common findings include hypokalemia, hypochloremia, and hyponatremia due to vomiting, or metabolic acidosis from laxative abuse. Low serum thyroxine (T4) levels, decreased triiodothyronine (T3) levels, and elevated reverse T3 levels are also seen. Elevated blood urea nitrogen levels, hypercholesterolemia, and elevated liver enzymes might indicate dehydration and nutritional deficiencies.
- Psychological assessment: This assessment identifies co-occurring mental health disorders, such as depression, anxiety, and substance use disorders, which are crucial for developing a comprehensive treatment plan.
- Use of diagnostic criteria: The clinician uses the DSM-5 criteria to confirm the diagnosis of bulimia nervosa. These criteria include recurrent episodes of binge eating, inappropriate compensatory behaviors, and self-evaluation unduly influenced by body shape and weight.
- Differential diagnosis: The clinician considers other potential diagnoses to ensure an accurate diagnosis of bulimia nervosa. This includes differentiating it from anorexia nervosa, binge-eating/purging type, where binge-eating behaviors occur only during anorexia episodes. Binge-eating disorder involves binge eating without compensatory behaviors. Kleine-Levin syndrome features disturbed eating without the psychological features of bulimia nervosa. Major depressive disorder with atypical features involves overeating without compensatory behaviors and excessive concern with body shape and weight. Borderline personality disorder includes binge-eating behavior as part of impulsive behavior.
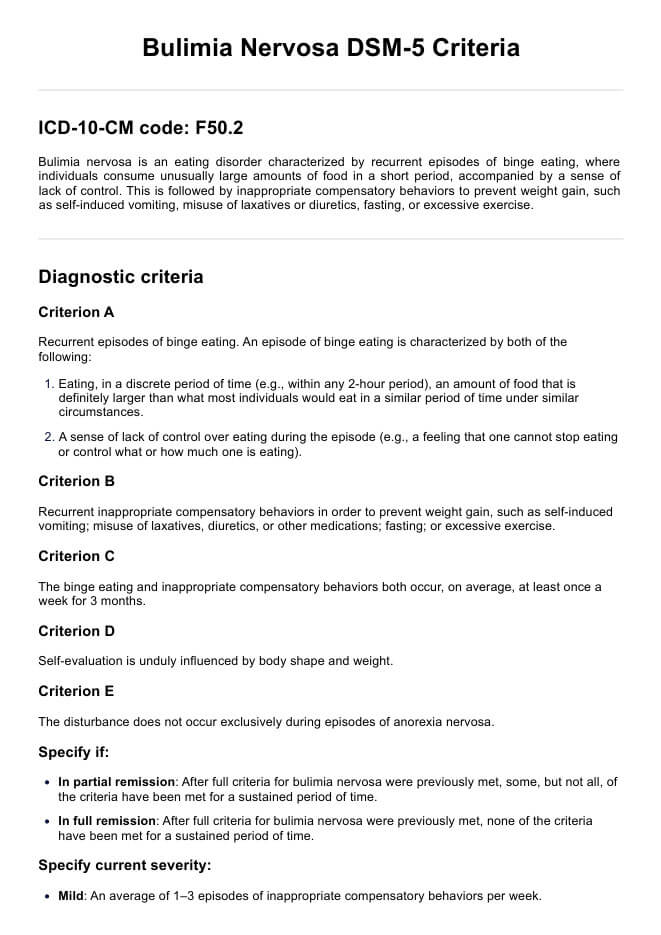
Bulimia nervosa DSM-5 diagnosis criteria
The DSM-5 outlines specific criteria for diagnosing bulimia nervosa. Here is an abridged version:
- Criterion A: Recurrent episodes of binge eating, characterized by eating an excessive amount of food in a discrete period and a sense of lack of control over eating during the episode.
- Criterion B: Recurrent inappropriate compensatory behaviors occur to prevent weight gain, such as self-induced vomiting, misuse of laxatives, diuretics, fasting, or excessive exercise.
- Criterion C: These behaviors occur, on average, at least once a week for 3 months.
- Criterion D: Self-evaluation is unduly influenced by body shape and weight.
- Criterion E: The disturbance does not occur exclusively during episodes of anorexia nervosa.
When making a diagnosis, you should also specify whether the patient is in partial remission or in full remission. You must also specify the current severity, ranging from mild to extreme, based on the frequency of inappropriate compensatory behaviors.
For a more detailed version of the diagnostic criteria, please refer to our template.
Differences between the DSM-4 and DSM-5 criteria
The DSM-5 criteria for bulimia nervosa include several significant changes from the DSM-IV. One major difference is the reduction in the binge eating frequency threshold from twice per week to once per week. Additionally, the DSM-5 removed the distinction between purging and non-purging subtypes of bulimia nervosa, simplifying the diagnosis. The requirement that self-evaluation is unduly influenced by body shape and weight was retained in the DSM-5.
Furthermore, the DSM-5 specifies that binge eating or purging behaviors do not occur exclusively during episodes of anorexia nervosa, ensuring clear differentiation between these disorders. Another important update is the formal recognition of binge eating disorder as a distinct diagnosis, which was previously classified as eating disorder not otherwise specified (EDNOS) in the DSM-IV.
How is bulimia nervosa treated and managed?
Treating and managing bulimia nervosa involves a multifaceted approach, as there is no single cure for the disorder. Here are common treatment and management strategies:
- Cognitive-behavioral therapy (CBT): CBT is the gold standard treatment, focusing on changing distorted thoughts and behaviors related to eating, body image, and weight.
- Medications: Antidepressants, particularly selective serotonin reuptake inhibitors (SSRIs) like fluoxetine, have been shown to be effective in reducing binge eating and purging behaviors. These medications can help alleviate symptoms of depression and anxiety that often co-occur with bulimia nervosa.
- Nutritional counseling: Dietitians help individuals develop a balanced eating plan, restore regular eating patterns, and address nutritional deficiencies.
- Interpersonal psychotherapy (IPT): Improves interpersonal relationships and communication skills, reducing binge eating and purging behaviors.
- Family-based therapy: Involves the family in the treatment process for adolescents and young adults, creating a supportive home environment and assisting in the recovery process.
Commonly asked questions
Bulimia, or bulimia nervosa, is an eating disorder characterized by recurrent episodes of binge eating, during which the person cannot stop eating. It is then followed by inappropriate compensatory behaviors to prevent weight gain.
The two subtypes of bulimia nervosa are the purging type, which involves self-induced vomiting or misuse of laxatives, and the non-purging type, which involves fasting or excessive exercise.
The two classic characteristics of bulimia nervosa are recurrent episodes of binge eating and inappropriate compensatory behaviors to prevent weight gain.


















-template.jpg)


















































































